Scapula Fractures: Open Reduction Internal Fixation
Peter A. Cole
Indications/Contraindications
In 1938, Wilson recorded a 1% incidence of scapula fractures in a comprehensive review of 4,390 broken bones. It is estimated that scapula fractures account for 3% to 5% of all fractures about the shoulder girdle. The well-endowed parascapular musculature, the oblique plane mobility of the scapula on the thorax, and the surrounding skeletal structures (which usually yield first) explain the relative rarity of scapula fractures. However, increased recognition of shoulder morbidity after high-energy trauma as well as improving familiarity with surgical approaches to the scapula have clarified the indications for nonoperative versus surgical treatment.
Fractures of the scapula follow a bimodal pattern of injuries based on the vector and mechanism of force to the shoulder. Low-energy and sporting accidents often lead to partial articular fractures that usually involve the anterior glenoid process and are commonly associated with anterior shoulder dislocations. These fractures are often referred to as bony Bankart lesions and may be characterized by anterior shoulder instability. If shoulder instability is present either clinically or on radiographic examination, then operative intervention in an appropriate surgical candidate is recommended. These criteria are usually present with fractures involving more than 20% of the articular surface.
A second variety of scapula fractures involves the glenoid neck and body, and they generally occur as a result of high-energy trauma. These fractures may or may not involve the glenoid articular surface. Because of the mechanism causing the fracture, associated injuries occur in many of these patients. In seriously injured patients, diagnosis and subsequent treatment of a scapula fracture are often delayed due to treatment of other life-threatening or limb-threatening conditions. According to a common misconception, scapulothoracic dissociation frequently occurs in the setting of scapula fractures; however, scapulothoracic injury results from a violent traction force to the upper extremity, which is quite the opposite mechanism of a typical scapula fracture.
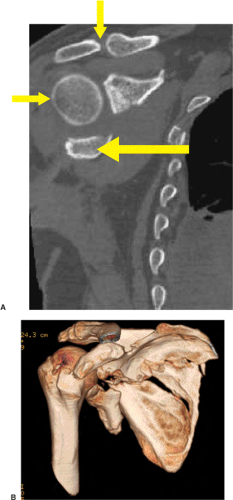
Displaced scapular fractures that extend into the glenoid articular surface often require surgical treatment. Articular fractures should be treated with open reduction and internal
fixation (ORIF) if a step off of 3 to 4 mm is encountered and more than 20% of the joint is involved (Fig. 2.1). Lesser degrees of articular step off, gap, and percentage of joint involvement, must be placed into the context of the patient’s occupation, age, activity level, physiologic status, and hand dominance.
fixation (ORIF) if a step off of 3 to 4 mm is encountered and more than 20% of the joint is involved (Fig. 2.1). Lesser degrees of articular step off, gap, and percentage of joint involvement, must be placed into the context of the patient’s occupation, age, activity level, physiologic status, and hand dominance.
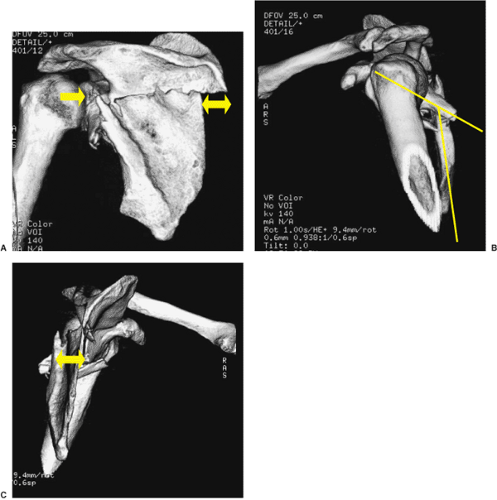
The optimal treatment of displaced extra-articular scapular fractures remains controversial. Recent studies support internal fixation of scapula neck fractures since large displacement or angulation leads to compromise of shoulder function. Ada and Miller have recommended ORIF of scapular neck fractures when the glenoid is medially displaced more than 9 mm or angular displacement exceeds 40 degrees. Their recommendation is based on a review of 16 patients treated nonoperatively: 50% had pain, 40% had exertional weakness, and 20% had decreased motion at a follow-up of 15 months or later. Eight patients in this same study were treated operatively, and all achieved a painless range of motion.
In the experience of other authors, medialization of the glenoid up to 1 cm has been well tolerated in most patients. Therefore, ORIF should be considered when medialization of the glenohumeral joint measures more than 15 mm, angular deformity in the semicoronal plane is more than 25 degrees, or fracture translation exceeds 100% at the lateral border of the scapula (Fig. 2.2). The indications for surgery are even stronger when two or more of the noted severity criteria are met.
In 1993, Goss described the superior shoulder suspensory complex (SSSC), an osseoligamentous ring made up by the acromion, coracoid, clavicle, and glenoid (Fig. 2.3). Goss theorized that if two disruptions are found in the ring structures, including their capsuloligamentous connections, then the glenohumeral joint would be “floating”, a condition that describes discontinuity between the axial and appendicular skeleton (Fig. 2.4). Although this theory has been challenged by some authors, Goss advocated surgery if two or more components of the SSSC are injured simultaneously. Further studies have suggested that surgery is indicated when the SSSC complex structures are displaced and unstable. Somewhat arbitrarily, if each SSSC injury causes displacement of more than 1 cm, the floating shoulder condition warrants surgery in an appropriate candidate. Most commonly, the decision-making process leads to surgical fixation of both injuries, which facilitates early rehabilitation.
Isolated fractures to the acromion or coracoid process are less common. Acromion process and spine fractures occur as a result of direct and concentrated blows to the superior shoulder region, whereas coracoid process fractures result from traction injuries through the biceps and coracobrachialis. If either an acromion or coracoid fracture is displaced more than 10 mm, ORIF may be indicated in a physiologically young and active patient. If the acromion fracture is displaced, then a supraspinatus-outlet x-ray should be evaluated for acromial depression, which may contribute to impingement syndrome, and therefore warrant operative correction.
Surgery is contraindicated when an extra-articular scapular fracture is displaced less than 10 mm and angulated less than 25 degrees because the outcomes of nonoperative treatment for even moderately displaced scapula fractures are uniformly good. Active mobility of the elbow and wrist are encouraged immediately, but a sling and rest are indicated for 10 to 14 days. Scapula fractures heal rapidly due to the rich blood supply in the shoulder girdle. Active range of motion can be started by 4 weeks and maximized quickly. Resistive exercises are begun by 8 weeks, and return to full activities is usually possible by 12 weeks.
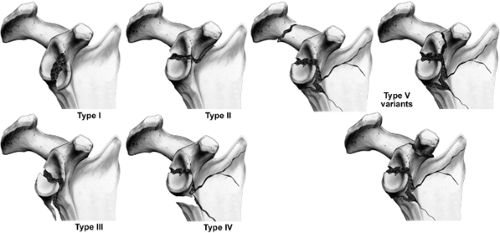
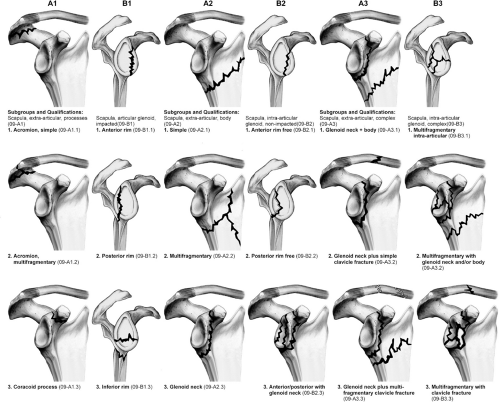
Classification
Only a few classifications have been developed for scapula fractures. The classification of Ada and Miller, as well as that of Hardegger et al, are anatomically defined and comprehensive. The classification scheme developed by Mayo et al is a reorganized version of the Ideberg classification and is based on a consideration of the imaging and operative findings of 27 intra-articular glenoid fractures. The latter classification is helpful in directing surgical decision making, and it takes into account the associated scapula body and process fractures (Fig. 2.5). The Orthopaedic Trauma Association (OTA) Classification System is an alphanumeric system in which both intra-articular and extra-articular variants are classified (Fig. 2.6).
Preoperative Planning
History
As with many fractures, indications for surgery can be less than distinct. Manual laborers who work with heavy loads and high-demand athletes may need surgery with relatively few indications. Also, if the injury occurs in the dominant extremity of an active individual, or if a patient requires engagement in significant overhead activity, then ORIF may be an attractive alternative treatment. However, injuries more than 3 weeks old, in elderly patients, and in individuals with multiple confounding co-morbidities, nonoperative treatment is likely the best choice.
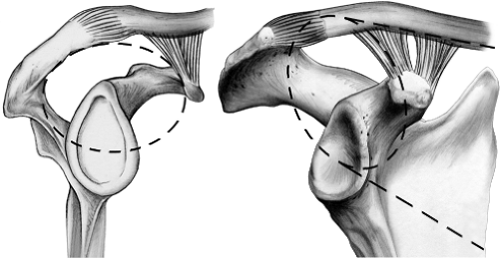 Figure 2.3. This illustration depicts the SSSC, which is an osseoligamentous ring made up of the structures along the broken line circle in this illustration. Goss theorized that if two structures in the ring are disrupted, then a floating shoulder lesion, without osseous or ligamentous continuity between the axial skeleton and the forequarter, would exist. A case of a floating shoulder lesion is illustrated at the end of this chapter (Figs. 2.17, 2.18, 2.19, 2.20, 2.21, 2.22, 2.23, 2.24, 2.25, 2.26). |
Physical Examination
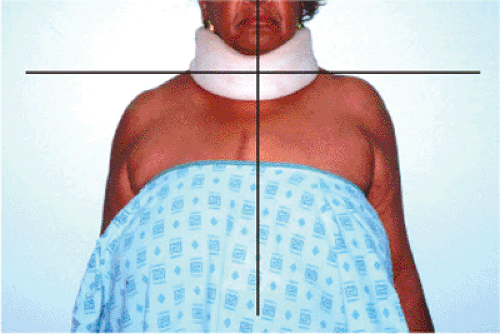
The physical examination in the multiply injured patient should follow the advanced trauma life support (ATLS) guidelines. In less seriously injured patients, inspection of the shoulder in a standing or sitting patient is helpful (Fig. 2.7). Medial and caudad displacement of the shoulder may be obvious and cause asymmetry, and it correlates well with the degree of medialization and depression of the glenoid found on radiographs. Because of pain, patients with displaced scapula fractures, particularly when associated with multiple rib or clavicle fractures, cannot voluntarily forward elevate or externally rotate their shoulders to any significant degree.
Ipsilateral, concomitant, neurovascular injuries, while uncommon, require a careful assessment of the brachial plexus and distal limb perfusion. Brachial-plexus injuries occur in up to 10% of patients with scapula fractures and may at times be subtle. Axillary nerve sensation should be documented; however, motor assessment is frequently impossible with displaced fractures. The integrity of the skin should be assessed because abrasions are common after the typical direct-blow mechanism to the shoulder that causes scapula fractures (Fig. 2.8). If the circulation in the upper extremity is questionable, vascular surgery consultation and angiography is strongly recommended.
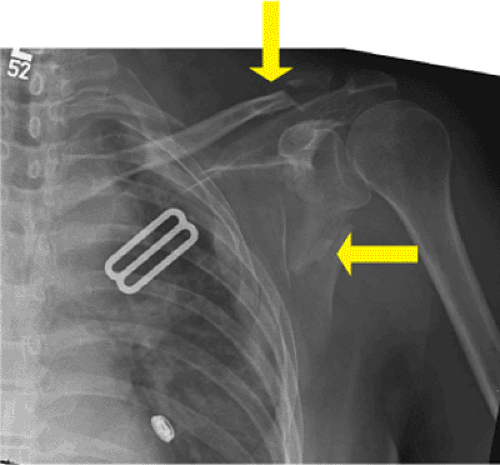
Radiographic Studies
Three plain x-ray views should be evaluated before proceeding to other studies, which include anteroposterior (AP), scapula Y, and axillary views. The AP x-ray of the scapula should be taken 35 degrees off the sagittal plane to correspond with the same angular position of the scapula on the thorax. The orthogonal scapula Y view is 90 degrees to the AP. The axillary lateral is the most difficult to obtain because of patient discomfort, but it is extremely important.
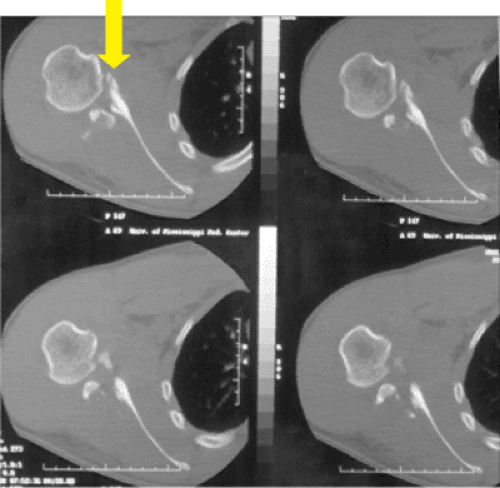
If an intra-articular glenoid fracture is detected on any x-ray view, then a two-dimensional computed tomography (2D-CT) scan with 1 mm axial cuts, together with coronal and sagittal reconstructions, are helpful to delineate articular displacement, comminution, and fracture location (Fig. 2.9). If more than 1 cm of fracture displacement is found at the scapula neck in any x-ray view, then an opposite shoulder AP radiograph and a three-dimensional (3D)-CT scan should be obtained to better define the fracture displacement. Being misled with an AP view of the injured shoulder is common because the glenoid may be significantly angulated through the lateral border so that visualization of the glenohumeral joint (clear space) is impossible. In these circumstances, a 3D-CT scan is helpful in evaluating angular deformity and medialization of the glenoid.
Surgical Considerations
The scapula is part of a suspensory mechanism of the shoulder, which attaches the upper extremity to the axial skeleton through the clavicle. Eighteen muscular origins and insertions on the scapula aid in providing a stable base for glenohumeral mobility. The goal of surgery is to restore this stable base as well as the relationship of the axial and appendicular skeleton and thus allow for early rehabilitation.
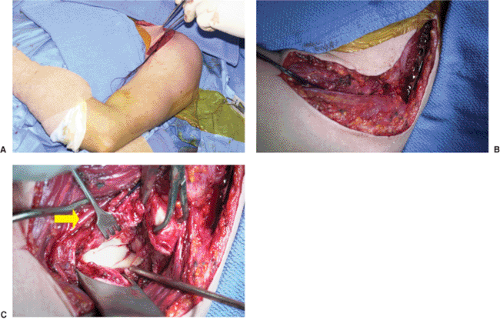 Figure 2.10. A.
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|