Rotator Cuff Arthropathy: The Unconstrained Arthroplasty
Ori Safran
Joseph P. Iannotti
O. Safran: Fellow, Orthopedic Department, Cleveland Clinic Foundation, Cleveland, Ohio.
J. P. Iannotti: Chairman, Orthopedic Department, Cleveland Clinic Foundation, Cleveland, Ohio.
INTRODUCTION
The combination of an irreparable rotator cuff tendon tear and severely damaged glenohumeral joint is the common end-stage result of several disease processes such as rheumatoid arthritis (RA), rotator cuff tear arthropathy (RCTA), and Milwaukee shoulder syndrome. By creating a substantial defect in the rotator cuff tendons, these disease processes lead to destabilization of the glenohumeral joint with subsequent superior migration of the humeral head and secondary severe damage to both the intra-articular and extra-articular elements. The result is a painful, dysfunctional shoulder that necessitates, in many cases, a surgical solution to be carried out to decrease patients’ morbidity. However, to date there has been no one surgical procedure to provide an optimal solution for this difficult problem. The aim of this chapter is to focus on the unconstrained arthroplastic solutions for the RCTA. We will begin by reviewing the pathomechanics, differential diagnosis, and some of the nonarthroplasty solutions available.
PATHOMECHANICS
The glenohumeral joint lacks significant intrinsic bony stability and thus relies largely on its soft tissue components. The rotator cuff tendons provide a major contribution to the dynamic stabilization of the glenohumeral joint by increasing the concavity-compression force in the joint.5,19,22,25,45 By their synchronous action, the rotator cuff tendons oppose the displacing effect of the strong deltoid muscle, keeping the humeral head centered in the glenoid fossa throughout its movement.37,46,47 The coupled work of the infraspinatus and subscapularis muscles has been shown to be a major factor in superior glenohumeral stability, whereas the contribution of the supraspinatus is less significant.18,40 A massive tear, consisting of the supraspinatus and at least one of the other rotator cuff tendons17 (in most cases the infraspinatus), may render the rotator cuff’s anterior and posterior force couple ineffective in both the vertical and the transverse planes. The result is a diminution of joint reaction force and a change in the overall direction of the joint force that leads to the destabilization of the glenohumeral joint.32 In cases in which the long head of biceps is still functional, it may oppose, to some extent, the superior migration of the humeral head.23,24 Once the proximal pull of
the deltoid is left unopposed, the humeral head migrates superiorly toward the coracoacromial (CA) arch. The humeral head articulates with the CA arch superiorly and the superior glenoid rim inferiorly, leading to flattening of the superior part of the humeral head and tuberosities (“femoralization”), rounding and thinning of the CA arch (“acetabularization”), and destruction of the superior glenoid region (Fig. 25-1). The acromioclavicular joint is also frequently involved in the process, joining its cavity with that of the now joined synovial intra-articular and subacromial bursae spaces. The deltoid, which has lost its fulcrum, has a smaller mechanical advantage and. Therefore, must generate more force to perform its function.40 The end result is an incongruous, unstable joint with a higher joint friction and superiorly malpositioned center of rotation.
the deltoid is left unopposed, the humeral head migrates superiorly toward the coracoacromial (CA) arch. The humeral head articulates with the CA arch superiorly and the superior glenoid rim inferiorly, leading to flattening of the superior part of the humeral head and tuberosities (“femoralization”), rounding and thinning of the CA arch (“acetabularization”), and destruction of the superior glenoid region (Fig. 25-1). The acromioclavicular joint is also frequently involved in the process, joining its cavity with that of the now joined synovial intra-articular and subacromial bursae spaces. The deltoid, which has lost its fulcrum, has a smaller mechanical advantage and. Therefore, must generate more force to perform its function.40 The end result is an incongruous, unstable joint with a higher joint friction and superiorly malpositioned center of rotation.
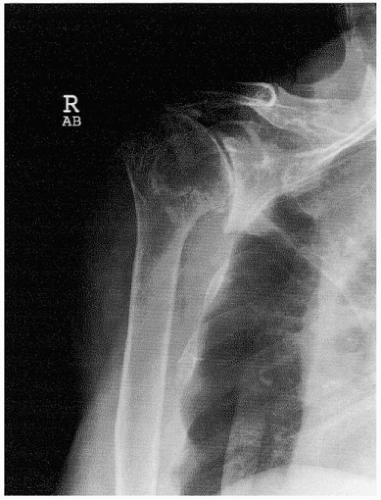 Figure 25-1 X-ray of shoulder joint with rotator cuff-deficient arthritis (RCDA). Notice the “acetabularization of the “socket.” |
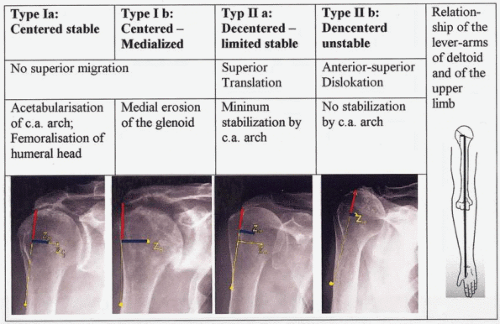
A pathomechanistic and pathomorphologic classification of glenohumeral rotator cuff-deficient arthritis (RCDA), based on the position and stability of the humeral head, is presented in Figure 25-2.36
The classification is independent of the underlying pathologic conditions and is based on two critical issues for the function of the deltoid muscle: the glenohumeral center of rotation and the degree of anterior-superior instability.
DIFFERENTIAL DIAGNOSIS
Although the end result is similar, it is important to recognize the various disease processes leading to glenohumeral RCDA.
Rheumatoid arthritis is the most common cause of RCDA. Between 48% and 65% of patients with RA have significant glenohumeral joint involvement. Approximately 24% of those having glenohumeral arthritis will have a simultaneous rotator cuff tear.26,38 Superimposed on the aforementioned changes are severe osteopenia, erosions of the entire glenoid without osteophyte formation, and medialization of the glenohumeral joint.
Rotator cuff tear arthritis is the extreme product of a massive rotator cuff tear. The term, coined by Neer et al. in 1983,30 refers to a primary massive rotator cuff tear that by virtue of mechanical superior instability and nutritional effects leads to a secondary glenohumeral joint destruction.21 It is believed that between 0% and 25% of massive rotator cuff tears will result in RCTA, but it is difficult, if not impossible, to predict which of the massive tears will result in RCTA.
The Milwaukee shoulder syndrome was originally described by McCarty et al. in 1981.29 This is an uncommon entity affecting shoulders of elder people, predominantly women. It consists of a massive rotator cuff tear, joint instability, bony destruction, and large, bloodstained joint effusion containing basic calcium phosphate crystals, detectable protease activity, and minimal inflammatory elements. Its relation to RCTA is not clear, and it might represent one of the elements just described.1 The role of the basic calcium phosphate crystals in creating this syndrome is still controversial. Whether it is the cause of the articular damage, through macrophage spillage of proteases, or just the result of the osteoarthritic process is still unknown.21
Primary glenohumeral osteoarthritis is the most common cause for shoulder joint replacement. Although recent data have shown an increase in glenohumeral cartilage damage in cadavers with concurrent rotator cuff tears,13,20 cartilage damage did not correlate with the size of tear. Clinically, primary glenohumeral osteoarthritis is infrequently associated with irreparable rotator cuff tears.
CLINICAL PICTURE
Patients with an arthritic shoulder and irreparable massive cuff deficiency are primarily elderly people, with female gender predominance. Their main complaints are of severe shoulder pain, limited range of movement, and, in some cases, recurrent swelling of the shoulder. The pain is constant, aggravated by shoulder motion and at nighttime,30 and felt at the periacromial region and glenohumeral joint line. On physical examination, atrophy of the infraspinatous and supraspinatus muscles, decrease in active and passive glenohumeral motion, and crepitus while moving the patient’s shoulder is observed.21 The x-ray image is typical and consists of a superiorly positioned humeral head, an “acetabularized” socket built up from thinned sclerotic acromion, and an eroded upper glenoid fossa (Fig. 25-1). Occasionally, the acromioclavicular joint and distal clavicle are also damaged and are thus included in the “socket.” Cases of secondary stress fractures of the thinned acromion have also been published.9
The combination of the clinical and radiologic information is, in most cases, sufficient to make the proper diagnosis, although other modalities such as computed tomography and magnetic resonance imaging may be needed for treatment planning.
TREATMENT
Rotator cuff tear arthropathy combines severe articular damage, bone destruction, osteoporosis, and loss of stabilizing rotator cuff tendons. In contrast with the more common primary degenerative shoulder arthrosis, the inherent instability of the rotator cuff-deficient shoulder necessitates specific consideration. Severe pain and shoulder dysfunction lead many of these patients to seek medical advice. Treatment armamentarium available is variable and includes both conservative and nonsurgical treatment, as well as surgical procedures such as humeral head replacement, total shoulder arthroplasty, and even arthrodesis and resection arthroplasty.
The responsibility of the orthopedic surgeon is to tailor the best treatment option for the particular patient, taking into account the patient’s symptoms, functional needs, and the bone and soft tissue conditions of the shoulder joint.
TREATMENT OPTIONS
Conservative Nonsurgical
Patients with mild symptoms and mild limitation in functional range of motion and activities of daily living should be treated nonsurgically. This includes the use of analgesics and physical therapy to maintain range of motion and strengthen the deltoid muscle. It has been shown that by strengthening the middle third of the deltoid, some improvement with superior stability control can be gained.16 The use of repeated steroid injections is discouraged, but an occasional injection may be helpful in managing the most acute symptoms.
Surgical intervention should be considered in those patients with unremitting pain, significant motion-related pain, and limitation in range of motion and activities of daily living.
Glenohumeral Arthrodesis
The basic concept of fusion is to eradicate pain with elimination of motion. However, there are several drawbacks to its use in patients with glenohumeral arthrodesis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree