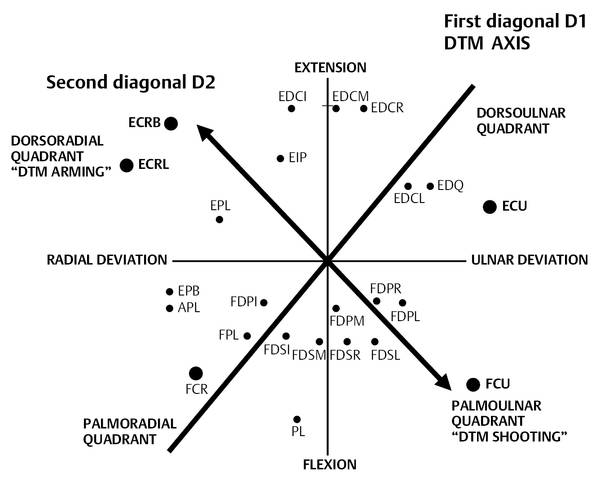
Role of Hand Therapy in the Treatment of Wrist Instability The wrist is an extremely complex structure that needs to be both mobile and stable to place the hand in space and hold it in a given position while transmitting incredible forces from the body to the hand or from the hand to the body. Any lesion to this delicate mechanism can alter this paradoxical balance of mobility versus stability and lead progressively to wrist instability. This chapter does not address wrist deformities caused by rheumatoid arthritis. The biomechanics of the wrist are so complex that different theories exist and there is still no consensus. The two-row theory is widely accepted1 although Taleisnik’s columnar theory has made wrist collapse deformities easier to understand.2 The wrist can be compared to a universal joint with nonintersecting axes. It allows the cardinal motions of flexion, extension, radial and ulnar deviation, and some longitudinal rotation. These motions combined with forearm pronosupination permit an asymmetrical circumduction. These movements are, however, purely theoretical. To describe and classify anatomy and movements, the first anatomists started from the existing system of planes of space. This classification gave birth to the single joint motion exercises and rehabilitation that we all learned during our training. If indeed single joint motion is possible, it can be done only under volitional control and only against small resistance. As Duchenne de Boulogne wrote: “Isolated movement is not in nature.” Due to the osteoarticular oblique geometry and diagonal axis and the muscles’ diagonal and spiral trajectories, all movements cross the three planes of space and have both spiral and diagonal character. From observing efficient compound movements in professional and sporting activities, Kabat and Knott observed patterns of motion that follow precise diagonal and spiral axes.3 For the wrist, Kabat ascertained four patterns or compound movements always associated with forearm pronation and supination. These four patterns follow two routes or “grooves” called “diagonals” (▶ Fig. 28.1). On each diagonal there is an agonist and an antagonist pattern. On the first diagonal the wrist starts from a position of extension, ulnar deviation, forearm pronation—from the dorsoulnar quadrant—to end in flexion, radial deviation, and forearm supination in the palmoradial quadrant. This movement corresponds to the precision grip of the hand of dexterity described by Napier.4 On the second diagonal the wrist starts from a position of extension, radial deviation, forearm supination—from the dorsoradial quadrant—to end in flexion, ulnar deviation, and forearm pronation in the palmoulnar quadrant. This movement corresponds to the dart thrower’s motion (DTM) and to the power grip of Napier’s hand of strength. Fig. 28.1 Diagram of the wrist’s four quadrants and two diagonal axes around which compound physiological hand and wrist functional movements occur. The schematic position of wrist and finger flexor and extensor tendons in relation to the wrist axis. D1: first diagonal and axis for DTM arming and shooting: Napier’s hand of strength. D2: second diagonal and axis for movements of Napier’s hand of dexterity. In 2007 the Wrist Biomechanics Committee of the International Federation of Societies for Surgery of the Hand (IFSSH) described DTM as a compound movement in a plane oblique to the flexion-extension and the radioulnar axis “in which wrist functional oblique motion occurs.”5 This pattern of motion is the most commonly used wrist motion in activities of daily living. Physiological wrist axis and movements should be the vector for both surgery and rehabilitation instead of single joint, analytical motion. Discussion of the anatomical factors that induce the DTM is beyond the scope of this chapter.6 Rehabilitation techniques, particularly muscle reinforcement presented in this chapter, emphasize the adaptation of proprioceptive neuromuscular facilitation (PNF) techniques as described by Kabat for hand therapy management of wrist instability. There is still no consensus on the definition and classification of carpal instability. According to Stanley, it is the term used for a group of conditions that result from injuries to the carpus, ranging from a simple sprain to a major fracture-dislocation. For the Mayo Clinic group, a traumatic carpal instability results from an injury in which loss of normal alignment of carpal bones develops early or late.7 Any injury or pathology to the wrist’s bony and/or fibrous skeleton structures will eventually evolve into carpal instability, articular cartilage degradation, and degenerative osteoarthritis. Trauma is the first cause. Severe fracture-dislocation calls for immediate open reduction and repair of bone and capsuloligamentous structures, allowing hand surgeons to establish a thorough diagnosis. Repetitive-motion low-grade injuries resulting from professional activities, and fibrous skeletal attenuation from sports such as gymnastics or activities of daily living such as pushing a wheelchair are also agents. Chronic instabilities evolve over years, sometimes after a neglected “sprain.” Occasional pain becoming constant leads the patient to consult. Often radiographs taken after a second trauma reveal a neglected former injury. At that time treatment will be conservative, rarely orthopedic, and often surgical. Associated ligamentous lesions are a common complication of supposedly noncomplicated wrist fracture. These cases, considered initially as benign and treated conservatively by orthopedic immobilization, may later cause more problems than severe cases treated surgically. Fracture of the distal extremity of the radius, if not properly reduced and stabilized, will create a “long ulna” in relation to the radius shortened by the fracture, resulting in a positive ulnar variance and an ulnocarpal abutment syndrome. If the height of the scaphoid is not maintained, a scaphoid nonunion will evolve into a scaphoid nonunion anterior collapse—a “SNAC wrist.” Likewise, a scapholunate interosseous ligament rupture will evolve into a scapholunate anterior collapse—a “SLAC wrist.” These are only a few examples. The Mayo Clinic team proposed a terminology for classifying the four most frequent forms of instability as follows: Rupture of the scapholunate interosseous ligament leading to scapholunate instability or dorsal intercalated segment instability (DISI) Rupture of the lunotriquetral interosseous ligament leading to a volar intercalated segment instability (VISI) Ulnar translocation of the carpus Dorsal subluxation instability Many less common forms, the names of which vary according to authors, can be cited. This list is far from being exhaustive: radiocarpal instabilities, perilunar instability, transscaphoid perilunate dislocation, retroulnar carpal dislocation, distal radioulnar joint (DRUJ) injuries, and triangular fibrocartilage complex (TFCC) injuries. Taleisnik introduced the concepts of static and dynamic instability. Static instability marks a carpal bone dissociation evident on radiographs, and dynamic instability appears only in stress or clenched-fist radiology or arthroscopy. Instabilities were further classified by the Mayo Clinic group as follows: Carpal instability, dissociative (CID) which involves intrinsic ligament disruption of the same row Carpal instability, nondissociative (CIND) which involves extrinsic ligament disruption between distal radius and proximal or distal row Carpal instability combined: CIC7 Up-to-date knowledge is indispensable for establishing a proper treatment and prevention program. As young, inexperienced general practitioner therapists, we often had referrals to treat patients for “wrist sprain.” Sometimes the prescription would indicate “improvement of range of motion and muscle reinforcement.” At the time, unaware of the natural history of wrist instability, in following these instructions we certainly accelerated the evolution of disability. Appropriate hand therapy management requires a working knowledge of wrist anatomy, biomechanics, traumatology, and pathology leading to acute or chronic instability and degenerative osteoarthritis. The hand therapist must have a basic knowledge of Imaging Radiographs, static and dynamic views Computed tomography (CT) Magnetic resonance imaging (MRI) Arthrography Hand therapists should also know what the main surgical procedures are and be aware of their benefits and limitations and of the modifications they bring to biomechanics. The hand therapist should be familiar with Surface anatomy and clinical palpation of anatomical landmarks following the five classical palpation zones: radial dorsal, central dorsal, ulnar dorsal, radial palmar, ulnar palmar Provocative tests Pain evaluation Outcome evaluation Besides the classical objective range of motion (ROM) and strength tests, which are often contraindicated because of tissue fragility or pain, the subjective wrist specific disability questionnaire developed by MacDermid8 has become a standard evaluation tool alongside the Disability of the Arm, Shoulder, and Hand (DASH) for rating wrist pain and disability. The outcome forms are administered before therapy, during intervention, and at discharge to document wrist status. Although it is not the therapist’s role to establish a diagnosis, the hand therapist may be the first to suspect carpal instability. Communication with the referring doctor should be immediate: a suggestion of additional examinations to produce evidence, for instance, of an abnormal scapholunate gap and provide the patient with the opportunity to be evaluated by a hand surgeon. Communication between the surgeon, physician, and therapist is mandatory to optimize patient outcome and to adapt hand therapy techniques, especially concerning range of motion, joint passive mobilization, and strengthening exercises and about what long-term results should be expected. Full range of motion is not necessary for satisfactory function. A painless stable wrist is more functional than a mobile painful one. Axial loading and resisted finger flexion create compression forces that tend to spread open the carpus. In the presence of carpal instability, osteoarthritis, or surgery on bone or soft tissues (such as capsuloligamentous repair, reconstruction, or augmentation), axial loading and resisted finger flexion must not be started until satisfactory healing is evident. In contrast, improvement of wrist stabilization by addressing and reinforcing wrist flexors and extensors is recommended. Resisted exercise of finger intrinsic muscles and the pronator quadratus tends to stabilize carpal bones. Specific exercises and neuromuscular stimulation can address these muscles.9 Muscle reinforcement will emphasize physiological muscle exercises and not single joint motion. At 30° of ulnar deviation and palmar flexion, compression forces acting through the carpal condyle are perpendicular to radioulnar joint surfaces. This wrist position on the DTM axis is privileged when practicing reinforcement techniques. Compression forces as well as pronation augment positive ulnar variance, increasing ulnar carpal abutment conflict. Exercises should be performed in neutral pronation-supination. In case of abutment syndrome, activities should be modified to include less pronation. The hand therapist will adapt the treatment protocol to each type of instability and each phase of the conservative, orthopedic, or surgical management. Conservative treatment is used both for mild and for severe cases. It can be a temporary solution before surgery or a permanent one when surgery is not indicated or is not accepted by the patient. It does not cause regression of instability and/or osteoarthritis but is important to decrease pain and maintain function. It is a “crutch” that compensates for anatomical damage and allows use of the hand. Conservative treatment options include steroid injections, pain-relieving modalities, splint use, and activity modification. Patient education regarding treatment options and realistic outcomes is crucial. The conservative treatment consists of
28.1 Introduction
28.2 Biomechanics
28.3 Carpal Instability
28.4 Etiology and Evolution
28.5 Classification
28.6 Prerequisites for Hand Therapy; Philosophy of Management
28.6.1 Basic Knowledge of Wrist Anatomy, Biomechanics, Traumatology, and Pathology
28.6.2 Clinical Evaluation
28.6.3 Diagnosis
28.7 Principles of Hand Therapy Treatment of Wrist Instabilities
28.7.1 Carpal “Spreading” under Compression
28.7.2 Wrist Muscles Work in Cocontraction
28.7.3 Safe Exercise Position
28.7.4 Positive Ulnar Variance
28.8 Clinical Forms of Instabilities: Chronic and Acute Instabilities
28.8.1 Conservative Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








