Rib to Pelvis Vertical Expandable Prosthetic Titanium Rib Insertion to Manage Neuromuscular Scoliosis
Anish G. R. Potty
John M. Flynn
DEFINITION
Vertical expandable prosthetic titanium rib (VEPTR) has gained enormous worldwide popularity in the last decade as an effective method to manage potentially lethal chest and spine deformity in children.
Initially, VEPTR was used primarily to expand the congenitally abnormal chest, particularly in circumstances where there were fused, absent, or hypoplastic ribs.
As surgeons gained familiarity with the technique, the VEPTR device was adopted as a very effective nonfusion method to manage severe early-onset neuromuscular scoliosis in conditions such as spinal muscular atrophy (SMA), spina bifida, and cerebral palsy.
With refinement, the rib to pelvis bilateral VEPTR technique has become one of the most commonly used initial implant strategies for these conditions because the technique can be done through a few small incisions, the spine is left untouched (and thus hopefully, unfused), and the expansions for growth are simple and of low morbidity.7
ANATOMY
The thoracic cage is composed of 12 pairs of ribs, the sternum, and 12 thoracic vertebrae. The ribs are interspaced with intercostal muscles. The external intercostals arise from the inferior border of one rib and attach to the superior border of the caudal rib with the external intercostal membrane lying posterior to it. Below this is the internal intercostal which has its fibers running at right angles to the external intercostal and the internal intercostal membrane deeper to the internal intercostal.
The neurovascular structures which are composed of the intercostal vein, artery, and nerve live beneath the internal intercostal muscle. It is important to understand that the vein lies superior to the subcostal groove, whereas the artery and the nerve reside inferior to the subcostal groove. This nerve innervates the adjacent intercostal muscles. Further deeper to the internal intercostal but above the parietal pleura is the innermost intercostal muscle, which becomes the transversus thoracic muscle anteriorly.
A normal thoracic development during childhood is essential for lung growth. Hence, respiratory function will depend on the lung growth and ability of the thorax to act as a dynamic pump to facilitate inhalation and exhalation.
The complexity of thoracic growth is not well understood but it is believed that the thoracic spine plays a critical role and contributes to vertical growth of the rib cage.
The thoracic spine grows 1.4 cm per year from birth to 5 years of age, 0.6 cm per year from 6 to 10 years of age, and 1.2 cm per year from 11 to 15 years of age.1, 3
The expected shortening of the thoracic spine can be calculated in congenital scoliosis or early spine fusion but the complex relationship between loss of thoracic volume and thoracic spine shortening and its indirect adverse effect on lung volume and expansion has yet to be quantified and remains unclear.
However, studies done on a natural history model of spondylothoracic dysplasia (Jarcho-Levin syndrome),4 in which the thoracic spine is only one-fourth of normal height in adults, have shown most surviving adults to have restrictive lung disease with an average vital capacity of only 27%.
Symmetric growth and the correct orientation of the ribs for the age of the child contributes to the width and depth of the rib cage and helps to maximize volume expansion and make respiration more effective. The thoracic cross-sectional volume is directly proportional to the length of the ribs and the degree of rib obliquity. At birth, infants have a square-shaped thoracic cross-section, which becomes a more rectangular-shaped thoracic cross-section in adults.
The ribs are oriented horizontally and the growth of the ribs occurs primarily at the anterior physis. At birth, the thoracic volume is only 6.7% of the adult volume. By 2 years of age, the ribs grows downward more obliquely and the thoracic cross-section changes to an oval shape. By 5 years of age, the thoracic volume increases to 30% of the adult size and to 50% of the adult size by 10 years of age. From age 10 years to skeletal maturity, the thorax grows rapidly and doubles itself to the adult size.
Almost 85% of lung alveolar cells are formed immediately after birth, with only slight increase in the first 2 years of life. The end age of alveolar cell formation is controversial and so is the concept of alveolar cell hypertrophy. The lungs still continue to increase in size even if the alveolar cell formation ceases due to compensatory lung growth triggered by a lung “stretch reflex.” Experimental pneumonectomy in young animals and partial pneumonectomy in children aged 30 months to 5 years showed compensatory lung growth by alveolar cell multiplication.
PATHOGENESIS
VEPTR is currently widely accepted treatment for volume depletion deformities of the thorax (VDD). VDD can be classified into three main types:
NATURAL HISTORY
Thoracic insufficiency may initially present with early occult respiratory deficiency when the child begins to show signs of limited pulmonary capacity. They fatigue easily with play activities and compensate with an increased respiratory rate at rest but do not yet require oxygen support. The final sequela of progressive thoracic insufficiency syndrome is respiratory insufficiency.
An increase in the ventilation requirements reflects an exponential clinical deterioration in respiratory function with important consequences for the family and the child.
Early-onset scoliosis in neuromuscular conditions such as SMA begins in the first decade of life due to truncal weakness. It then progress steadily unless managed surgically and can become lethal. It occurs in 100% of the type I SMA and most of the type II SMA when they become nonambulators.
PATIENT HISTORY AND PHYSICAL FINDINGS
Physical examination should include careful evaluation of the spinal deformity, pelvic obliquity, sitting balance, and shoulder balance.
Respiratory effort is assessed by determining the rate of respiration, lung auscultation for abnormal breath sounds, anthropomorphic measurements (height, weight, chest circumference at the nipple line, and limb length) looking for failure to thrive, and the thumb excursion test to evaluate thoracic wall expansion during respiration.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The radiographic assessment includes standard posteroanterior (PA) (FIG 1) and lateral views of the spine with rib cage. The Cobb angle is measured for the scoliosis, and the head and truncal decompensation is assessed. The space available for the lungs to expand is measured by the ratio between the concave heights to the convex height.
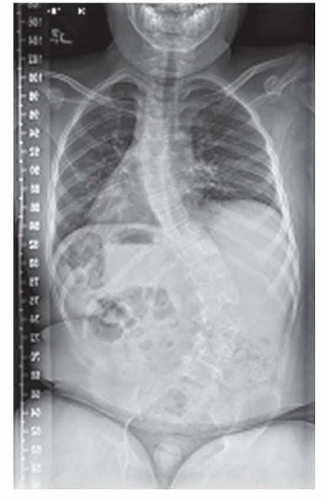
FIG 1 • Preoperative radiograph of a 10-year-old boy with SMA and progressive scoliosis. The preoperative Cobb angle was 56 degrees and a 3.5-cm pelvic tilt.
If cervical spine instability is a possibility, a cervical spine series including flexion and extension views is performed.
A formal consultation with a pediatric pulmonologist, including pulmonary function testing, is very valuable to establish baseline function and counsel the family appropriately regarding risk of postoperative pulmonary complications.
Magnetic resonance imaging (MRI) of the entire spine should be ordered to evaluate the spinal cord and those children who have any physical findings concerning for tethered cord.
Computed tomography lung volumes can be compared with normative values to provide more information but such results may not be available.
Dynamic MRI may be performed to assess the function of the diaphragm, and a screening MRI is routinely performed to look for abnormalities such as cord tethering or syrinx.
Echocardiogram can be done to detect early-onset cor pulmonale.
NONOPERATIVE MANAGEMENT
The primary nonoperative option is observation, with serial radiographs and close monitoring of pulmonary function.
In some cases, braces or serial casting can be offered, although it is often impractical in children with neuromuscular spinal deformity at risk for thoracic insufficiency.
SURGICAL MANAGEMENT
Bilateral rib to pelvis VEPTR technique offers a relatively minimally invasive way to manage early-onset neuromuscular scoliosis associated with thoracic insufficiency. The technique can be performed with relatively low blood loss and morbidity and with much less risk of autofusion as is seen in standard dual growing rod techniques.
The bilateral rib to pelvis VEPTR technique is generally contraindicated in ambulatory children because a recent report shows a significant incidence of crouched gait, likely due to mechanical factors at the lumbosacral junction.7
Indications
A rapidly progressive curve with pelvic obliquity and nonambulatory patients. Thoracic insufficiency may or may not be present.
A greater than 10% reduction in the height of the hemithorax on the concave side of the curve compared with the height of the contralateral hemithorax (space available for the lung is <90%)
Progressive thoracic insufficiency syndrome
An age of at least 6 months up to skeletal maturity. The younger the patient, the more likely there will be beneficial lung growth with thoracic expansion.
Concurrent approval of the previously mentioned indications by a pediatric orthopaedist, a pediatric general surgeon, and a pediatric pulmonologist
Contraindications
Inadequate soft tissue coverage for the devices. Generally, this correlates clinically with a child with a body weight below the 25th percentile.
Inadequate rib bone stock for device attachment, such as in a patient with severe osteogenesis imperfecta
Absence of cephalad osseous ribs for attachment of the devices
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








