21
Rheumatological history and examination
History
The musculoskeletal history has the same basic framework as any medical or surgical history with details of the presenting complaint, history of presenting complaint, etc. There are, however, a number of features that should be highlighted when clerking and presenting a patient with rheumatological disease.
- The most crucial element in a musculoskeletal history is to differentiate inflammatory and degenerative joint disease:
- Joint swelling may occur with either inflammatory or degenerative disease. The detection of swelling, its character and distribution forms the basis of clinical examination.
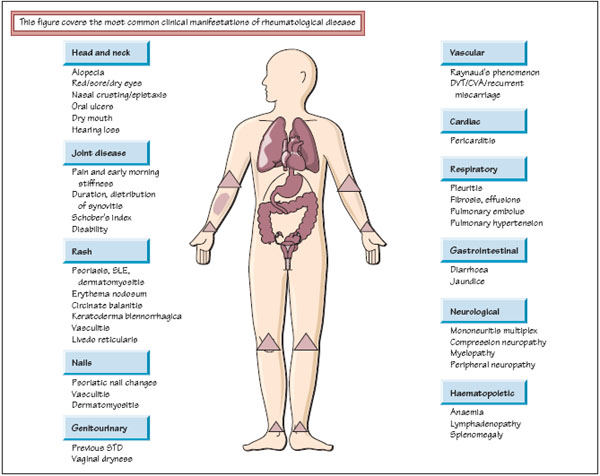
- Extra-articular disease is a frequent phenomenon in inflammatory conditions. Seeking examples of eye, skin and nail, respiratory or bowel symptoms may help not only in determining the underlying diagnosis but also its severity.
- Heritability plays a variable role in inflammatory disease and a family history of joint disease, psoriasis or autoimmune disease may be relevant.
- A summary of medications past and present is crucial. The efficacy and tolerability of, and patient’s compliance with, anti-inflammatories, disease-modifying antirheumatic drugs (DMARDs), immunosuppressives or biologic therapy is extremely helpful. A full alcohol and drug history is particularly pertinent in the assessment of a patient with gout.
- The degree of disability does not always correlate with the severity of joint deformity, so a full social history with particular attention to reports of work absenteeism and/or ability to self-care is mandatory.
Examination – general points
The purpose of joint examination is the detection of joint swelling, differentiation between inflammatory and degenerative joint disease and the assessment of disease activity in an individual patient.
- Joint swelling in inflammation (synovitis) is boggy in nature. The joint is often warm, with overlying erythema and there is often pain at the extremes of movement. Swelling due to degenerative disease is bony hard.
- Different inflammatory diseases have predilections for different sites. Rheumatoid arthritis, for example, favours the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints in the hand, with relative sparing of the distal interphalangeal (DIP) joints. However, osteoarthritis in the hand focuses on the first carpometacarpal (CMC) joint, the PIP joints (forming Bouchard’s nodes) and the DIP joints (forming Heberden’s nodes). The classic distribution for each inflammatory joint disease is covered in individual chapters.
- Many rheumatological conditions are systemic diseases. Potential extra-articular manifestations of disease must be sought in clinical examination (see figure opposite).
The GALS screen and detailed examination of the arm, leg and spine has already been described (see Chapter 3). The rest of this chapter is therefore devoted to examination of the hand, which follows the same paradigm of ‘look, feel, move’. For RA patients, the focus is not only the description of the classic bony deformity but also the detection of active synovitis (swollen and tender joints).
Hand examination
Look
- Stand back and take an overall view of the patient:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



