Fig. 24.1
Direct repair of the extensor mechanism with a braided monofilament polypropylene mesh. Additional fixation of the mesh is achieved transfixing it with a screw and washer

Fig. 24.2
The mesh is positioned anterior to the patella and then fixed with multiple nonabsorbable sutures
Once the host tissue has been brought to the correct position and the appropriate tension has been restored, the mesh is brought over the patella and secured proximally to the remnant quadriceps tendon or vastus lateralis muscle. At the end, the vastus medialis is mobilized to overlap the graft and underlying vastus lateralis. The outcomes of this technique have been reported in a series of 13 patients [39]. Although the outcomes were generally positive, three patients suffered a mesh rupture in the first 6 months after surgery.
24.7.5 Partial Allografts
Allografts allow for extensor mechanism reinforcement or reconstruction with the advantages of being a biological tissue, with good mechanical strength and no donor site morbidity. However their use is associated with several risks such as disease transmission, immune response (since they keep their allogenic properties), graft infection, and progressive stretching of the graft. Fresh frozen grafts are preferable since they have reduced allogenicity. Three options are currently available: Achilles tendon allograft, partial extensor mechanism allografts (PEMA), and complete extensor mechanism allografts (EMA). The use of Achilles tendon allograft with its calcaneal bone block is particularly indicated in cases of an intact patella and correct patellar height. Good recovery in terms of range of motion with no extension lag at final follow-up has been reported, although associated with a reoperation rate of 30 % [49].
Zanotti described partial extensor mechanism allograft (bone-patellar tendon-bone allograft) in 1995 [50]. It can be considered when the quality of the residual patellar tendon is poor and the patella is in good condition and can be left in position. Although it is more technically demanding compared to the whole EMA, it ensures a solid construct with the preservation of the remaining anatomic structures.
The patella is initially prepared to optimize the fixation on the host patella and maximize the surface area for the insertion of the quadriceps and patellar tendons. It is prepared to have an hourglass shape in the coronal plane, wider at the proximal and distal poles and thinner in the middle part and to obtain a bone block of about 1 cm thickness. The bone block should be slightly wider in its distal portion to increase its primary stability. The preparation of the host patella is carried out with a burr or an oscillating saw to prepare a trench hourglass-shaped and around 10 mm deep. On the tibia a bone trench is prepared in a similar manner with a wider distal part to increase primary stability and avoid proximal migration. The patella is positioned first, without impacting it, to avoid any risk of damage. Primary fixation is achieved with two or three metallic wires, whereas the quadriceps tendon is sutured with nonabsorbable stitches to the middle portion of the native quadriceps tendon. A metallic wire is positioned in the tibial graft. The tibial bone block is positioned in the trench with the knee in full extension in order to restore proper patellar height. Fixation and tensioning is ensured with multiple metallic wires and tightening of the metallic wire around a screw and washer. Additional stability may be achieved with staples. All soft host tissues are then mobilized to cover and protect the allograft. A PDS strip may also be applied and fixed in front of the allograft in order to help distribute the stresses during the postoperative period (Fig. 24.3).
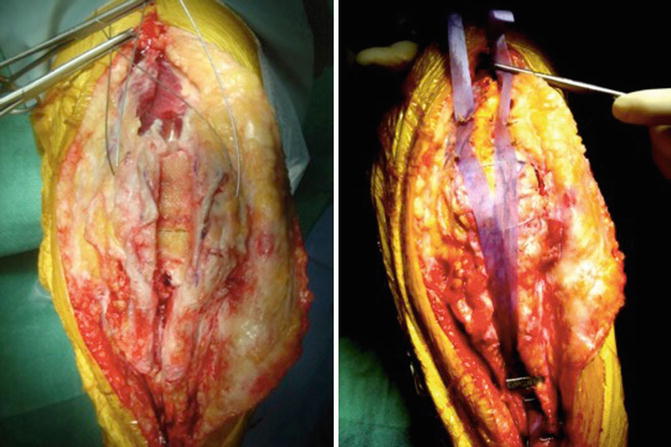
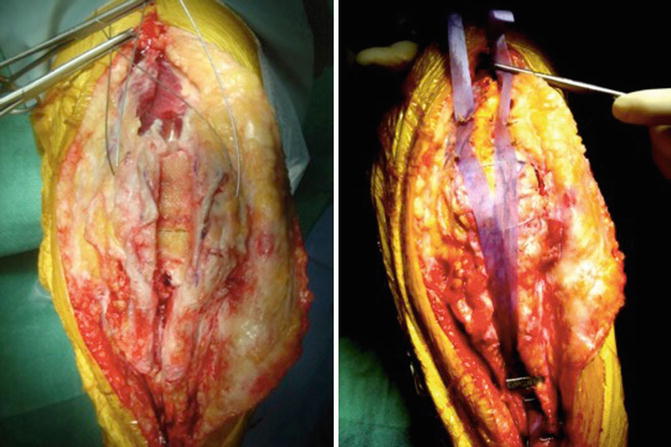
Fig. 24.3
A polydioxanone (PDS) strip is applied and fixed in front of the allograft to increase primary resistance of the construct
24.7.6 Extensor Mechanism Allograft
When the remaining native tendon had poor quality and tissue healing is considered to be difficult or impossible, EMA should be considered. This technique was initially introduced and popularized by Emerson in the late 1980s [51] for its superior mechanical properties compared to traditional allografts. However it should be considered as a salvage procedure in those cases where restoring the continuity and function of the extensor mechanism is impossible with traditional techniques [52]. When considering an EMA, the most critical aspect is the restoration of a correct patellar height. The patella is generally retracted proximally and usually extensive release is required to draw it back to the appropriate level. The allograft tissue usually includes a tibial tubercle of variable size, the entire patellar tendon and patella, and a large portion of the quadriceps tendon (at least 5 cm). The patella can be preserved or resurfaced; however, the bone of the allograft is at risk of further fracture due to its mechanical weakness [51]. When the option of preserving the patella is chosen, it is prepared in an hourglass shape (wider at the top and bottom and narrow in the middle) to increase the fixation area to the native patella and quadriceps tendon. After removing the cartilage layer and part of the subchondral bone with an oscillating saw, a graft of 10 mm thickness is obtained. The tibial bone block should be around 6–8 cm in length and 2 cm in width and depth. The bone block is prepared with a wider distal part in order to increase its fixation and reduce the risk of migration. In a similar way the proximal part is prepared in a dovetail shape to achieve a locking of the graft into the host native tibial allowing a press fit fixation.
The procedure is performed with a tourniquet inflated at 350 mmHg. The surgical incision should begin 10 cm above the proximal pole of the patella and extend 3 cm below the distal insertion. This guarantees enough space for proximal and distal fixation of the EMA. When multiple incisions are present, the most lateral should be preferred in order to respect the vascularization that comes from the lateral branches of the geniculate arteries [53]. Soft tissue dissection must respect blood supply; medial and lateral flaps of residual retinaculum are obtained before exposing the joint.
In addition the medial and lateral gutters and suprapatellar pouch must be released, and the medial and lateral soft tissue sleeves of the distal quadriceps must be prepared to host the EMA. The first step is the creation of the recipient site on the patella. It is prepared with an oscillating saw to match graft shape; redundant cancellous bone is removed to obtain a 10 mm deep trench. Once the correct height and match have been confirmed, two metallic wires are positioned transversely through the patella deep to the bottom of the trench. The tibial recipient site is created at a proper site with a saw. The trench is then prepared to ensure a perfect housing for the allograft. To prevent proximal migration of the graft, a host bony bridge of 10–15 mm should be kept in place below the tibial component anteriorly. Fixation of the graft begins with the patella. With the knee at 30° of flexion and once the correct patellar height has been identified, the bone block is placed into the trench. The graft should not be impacted to avoid any damage to the patellar cartilage and to decrease the risk of fractures. The two wires are then tightened, cut short, and buried. Additional fixation of the quadriceps tendon graft is achieved suturing it into the previously prepared center of the host quadriceps tendon with n.2 absorbable sutures. On the tibial side, a metallic wire is positioned into the bone block. A screw and washer is inserted distally to the tibial trench. With the knee in full extension, the graft is impacted in the trench and then secured looping the wire around the distal screw and tightening it. Additional fixation may be obtained with staples or screws. Soft tissue coverage may be increased detaching and advancing the remaining native patella tendon. The wound is then closed over a drain with absorbable sutures (0 or 2–0) being used for the deep dermal layer and staples or interrupted nylon sutures for the skin depending on the skin quality.
24.8 Conclusions
Complications involving the extensor mechanism after TKA are usually difficult to manage. Early diagnosis is crucial to prevent the potentially devastating effects on knee function. Patellar fractures can be treated conservatively with positive outcomes in the majority of cases. Patellar instability may be the consequence of a traumatic event or have an insidious onset. In this latter case the positioning of the components must be investigated as soft tissue procedures are usually ineffective in case of concomitant component malposition. In cases of traumatic disruption or when the components have been properly implanted, reconstruction of the medial patellofemoral ligament (MPFL) with the quadriceps tendon can be considered with or without additional lateral release or tibial tubercle transfer. Patellar or quadriceps tendon ruptures may have devastating effects. Direct repair is usually associated with poor outcomes. Direct repair with biological or synthetic augmentation can be performed in acute cases when the quality of the soft tissues is good. In chronic cases and when the quality of the surrounding tissues is poor, EMA represents the only option. Although it is considered a salvage procedure and is technically very demanding, it usually yields positive functional outcomes.
References
1.
Parker DA, Dunbar MJ, Rorabeck CH (2003) Extensor mechanism failure associated with total knee arthroplasty: prevention and management. J Am Acad Orthop Surg 11:238–247PubMed
2.
3.
4.
Rand JA, Lynch AF, Rorabeck CH, Bourne RB (1989) Patellar tendon rupture after total knee arthroplasty. Clin Orthop Relat Res 244:233–238PubMed
5.
Rosenberg AG (2012) Management of extensor mechanism rupture after TKA. J Bone Joint Surg Br 94:116PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








