(1)
Department of Orthopedic Surgery ASAN Medical Center, University of Ulsan College of Medicine, Seoul, Korea, Republic of South Korea
Abstract
Artificial joints do not assimilate into the human body and are not as durable as the human joints. Hence, artificial joints require a revision surgery after a certain period of time. Even though the artificial joint has not been used for a long time, revision arthroplasty may be needed in cases of severe pain and significant functional loss or when complications develop.
Artificial joints do not assimilate into the human body and are not as durable as the human joints. Hence, artificial joints require a revision surgery after a certain period of time. Even though the artificial joint has not been used for a long time, revision arthroplasty may be needed in cases of severe pain and significant functional loss or when complications develop.
Operative procedures for revision arthroplasty are generally more difficult than those for primary TKA and their prognosis is not as good as that of primary TKA. The operation may fail in the absence of thoughtful planning.
I would like to describe aseptic and septic revision arthroplasty separately as there are several differences between the two operations.
9.1 Introduction
The number of patients requiring revision arthroplasty is increasing. There are many reasons for this. First, the number of primary TKAs has increased significantly. Second, the indication for primary TKA has extended to young active patients. Third, the life span has prolonged and the patients now live longer than the expected TKA survival.
The need for revision before the average survival time of the artificial joint is considered to be a failure of the artificial joint under any circumstance. The most common indications of revision TKA are infection, followed by wear and loosening. Other causes are osteolysis, instability, stiffness, extensor mechanism dysfunction, and fracture.
The outcomes of revision TKA are not as good as those of primary TKA, but the results vary from surgeon to surgeon. Ritter et al. reported that the survival rate of revision TKA was 97 % at 6 years, while Haas and Dennis reported a survival rate of 83 % at 8 years. Sheng et al. analyzed 2,637 cases of revision TKA performed in Finland and reported that the 2-year survival rate was 96 %, 5-year survival rate was 89 %, and 10-year survival rate was 79 %. Prognosis was better when the patients were older than 70 years of age, when 5 years had elapsed from the time of primary TKA, and when the patellofemoral alignment was good. Singh et al. reported that activity is often restricted after revision TKA in case the patient is a woman, is over 80 years of age, and/or is exceedingly overweight (BMI > 40). Suarez et al. reported that 46 % of cases of failed revision TKA were due to infections.
Similar to primary TKA, the goal of revision TKA is to reduce pain, to improve function, and to provide a mechanically stable joint. For this purpose, it is necessary to reconstruct the bone defect, to establish mediolateral and extension–flexion gap balance, and to restore the extensor mechanism.
There are several factors to be considered while performing a revision TKA. First, it is necessary to know the causes of a failed TKA. Wear and loosening which has developed after 15 years of use is considered to be natural, whereas early wear and loosening is caused due to surgical failure, prosthesis defect, or overactivity of the patient. Revision TKA should be done to correct the causative factors. The probability of failure is high when revision TKA is performed simply to relieve pain without identifying the causes of failure. Revision TKA should be performed only when it is certain that the cause of pain is not reflex sympathetic dystrophy or the pain is not due to extrinsic causes. Second, the necessity and timing of the operation should be considered. Revision TKA should be performed when the pain is very severe, the patient cannot walk, or the lesion is progressing rapidly. It is not appropriate to perform revision simply because there are complications and the clinical manifestations are progressing. Patient’s general condition, activity, and life expectancy should also be considered. Just as there are indications for primary TKA, there also are indications for revision TKA. Indications for revision TKA should be decided more carefully as revision TKA is technically more demanding and has a poorer prognosis. However, once the decision has been made to perform revision TKA, it should be done as soon as possible in order to reduce the bone defect caused by osteolysis and instability and to prevent the progression of synovitis. Third, surgeons should be humble when evaluating their experiences or level of skills since an operation beyond their abilities can worsen the results of revision TKA.
9.2 Revision for Aseptic Failure
If there is no infection, revision TKA can be largely classified into partial replacement and total replacement of the component. If the wear is confined to the PE or loosening has developed in only one component despite of the long-term use, it may not be necessary to replace all the components. Engh et al. reported that isolated PE exchange for wear or osteolysis showed similar result with full revision when the component are well aligned and well fixed. However, many surgeons report that when partial replacement is done, the results are not good. Hence, it is increasingly recommended to replace all the components even when the problems are confined to one component. In cases of early wear and loosening, replacing all the components is required as it is likely to be caused due to surgical failure or implant defect.
9.2.1 Preoperative Checkup
9.2.1.1 General Condition
As revision surgery takes a long time and considerable bleeding is expected, patient’s general conditions including cardiopulmonary function and compromised immune system should be carefully evaluated. Also, infections in the other organs and diabetes mellitus should be treated or controlled before the revision TKA since the risk of infection is high.
9.2.1.2 Analysis of the Causes
The causes of failure of primary TKA should be identified before revision TKA based on the patient’s medical history, physical examination, and X-rays.
Loosening of the tibial or femoral component was the most common cause of revision TKA when the first-generation prosthesis and constrained type prosthesis were used, while patellar component loosening occurred mostly with the use of the second-generation prosthesis due to improper selection of implant or maltracking. The causes of loosening include an obese patient, overactivity, malalignment, instability, osteoporotic bone, and constrained type of prosthesis. Most of the times, it is necessary to establish a method for reconstructing the bone defect and for ensuring stable fixation. Currently, wear is one of the major reasons for performing revision TKA. This may be related to the patient, implant, and surgical factors. The method of treatment varies according to the causes, period from primary TKA, and extent of wear. If motion limitation is simply due to adhesions, enhanced rehabilitation program should be started first, and brisement and simple adhesiolysis with arthroscopy can be followed in order to increase the ROM. If the ROM is limited due to the flexion/extension gap discrepancy or other surgical faults, revision TKA should be performed to correct the gap discrepancy. The incidence of revision TKA due to instability is not high, but surgical correction is needed in severe cases. The cause of instability is mostly surgical failure to achieve the balance, which includes flexion/extension gap imbalance, inadequate release of the ligament, and patellar maltracking in addition to wear and loosening. Muscle weakness or trauma is another cause of instability.
An extrinsic lesion can affect the results of primary TKA and it should be evaluated before revision surgery. The hip and ankle joint pathology and the deformity of the femur and tibia are another cause of failure of primary TKA.
9.2.1.3 Preoperative Knee Joint Assessment
Physical Examination
The first step in preoperative assessment is to check the skin condition. The site and condition of the incision scar, the elasticity of skin, and vascularity are the important elements that affect the prognosis of revision. Second, the treatment method for revision TKA can differ according to the condition of the knee joint and its function. This includes the degree of instability, deformity, limited ROM, and muscle strength. It is necessary to determine the degree, site, direction of deformity and whether it is a fixed or flexible deformity in order to plan the revision. The degree of limited motion and its causes are very important factors for deciding the revision and for choosing the method of revision. The methods of revision can be different according to the causes of limited motion such as adhesions of soft tissues or gap discrepancy due to surgical failure. Dorr stated that soft tissues often need special management when the preoperative flexion motion is less than 90° or the flexion contracture is greater than 15°. The quadriceps muscle power also has a significant impact on the prognosis of revision TKA, and hence its tension and extensor lag should be evaluated before surgery.
Radiological Examination
The degree of deformity, bone defect, instability, and patellar tracking should be examined on the plain X-ray. Loosening may only be seen when the projection is accurate and its accuracy increases with the use of fluoroscopy. On X-ray, bone defect appears much smaller than its actual size. Stress X-ray also helps in checking the instability whether it is due to PE wear, relaxation of ligaments, or prosthesis instability. X-ray of the contralateral knee is necessary in order to compare both sides and to check the prosthesis size.
In some cases, CT scan can be of great help to assess the degree of osteolysis, rotational deformity, and the position of the prosthesis.
Miscellaneous
Before revision TKA, the possibility of an infection should always be ruled out and any suspicious factor should be thoroughly examined. Barrack et al. and Duff et al. suggested performing a routine arthrocentesis before revision TKA.
Finally, the size and brand of the primary prosthesis should be checked to determine whether that product had any material or design defect, whether it is appropriate for revision and which options are available.
9.2.2 Surgical Procedure
The surgical procedures that can be considered based on the preoperative analysis include which type of prosthesis is to be used, which approach will be better, how the prosthesis can be removed, how to perform osteotomy and bone reconstruction, how the soft tissue treatment can be done to achieve balancing, and how to fix the prosthesis.
9.2.2.1 Implant selection
Implant selection is usually done before the operation, and it is desirable to select an implant that offers all the options since the surgical procedure may change during the operation. Since the current prostheses have a modular system, all sizes of each component need to be kept ready. Metal augment and an extended stem with an offset stem, should be available. Also, it is desirable to use the prosthesis which has an instrument for easy removal of the implant.
Factors that affect implant selection include range of motion, instability of the joint, amount and type of bone defect, alignment of lower limbs, patellar tracking, and type and shape of the prosthesis used in the primary TKA.
The most important factor is the motion constraint of the implant. Less constraint is better for long-term survival of the implant, but constrained prosthesis may be required in some cases of revision TKA. The CR type of prosthesis can be used when only the PE needs to be replaced in patients in whom this type of prosthesis has been used before and in whom the PCL is sound. The benefit of using this type of prosthesis is that it minimizes the bone loss. However, there are a few problems when revision is to be done; it is not easy to correct the deformity and it is difficult to achieve the balance. If the PCL is not normal, it might be difficult to achieve stability in flexion or the ROM may be limited. Clinically, this type of prosthesis can be used by experienced surgeons only when there is little deformity, instability, and bone loss.
The PS type of prosthesis is the most appropriate implant when the flexion and extension gaps have been restored, the joint line is retained, and the collateral ligament has been balanced. The benefit of using this type of prosthesis is that it provides reliable substitution when the PCL is missing or incomplete, it makes it easy to correct the deformity, it is stable in flexion, and the patient can achieve a good range of motion. The drawbacks of PS type of prosthesis is that posterior dislocation may occur if the collateral ligaments are not balanced or when there is flexion and extension gap discrepancy. Gustke reported that 82 % of cases of revision TKA can be done with semiconstrained implants.
Constrained type of prosthesis is used when there is marked instability due to severe collateral ligament deficiency or when there is moderate to severe flexion/extension gap discrepancy. In other words, a constrained prosthesis is used when there is mediolateral instability in extension or dislocation of the prosthesis occurs in flexion. There are two types of constrained prosthesis, VVC (varus–valgus control) type and linked type, and some of the linked types allow for rotation. The appropriate type of constrained prosthesis should be selected according to the degree of instability. In general, the linked type can correct the instability in a more strict sense than the VVC type, but the motion constraint is increased. The linked type can be used in severe instability, severe bone defect, or hyperextension as it constrains motion more than the VVC type. As a result, the linked type is associated with a higher rate of loosening.
Author’s Method

I recommend the PS type in most revision cases, and the constrained type is used only if it is absolutely indicated. The decision for using of constrained type is determined by the balance of extension and flexion gaps and the status of the collateral ligament before or during the operation. When an infection and severe instability have persisted for a long time, when AORI Type III bone defect exists or when joint dislocation has occurred, I use the constrained type for revision TKA. In such cases, the collateral ligaments are unreliable even though they appear sound in the operation field. Also, the constrained type is used if dislocation in flexion develops with an adequate extension gap state during the operation.
I decide to use the constrained type by increasing the PE thickness step by step. I start with a PE that seems to fit the flexion/extension gap and followed by inserting a one-size thicker PE in flexion state. In most cases, the flexion gap adapts to this thickness, but flexion contracture occurs because the extension gap becomes narrow. I extend the knee forcefully. If the flexion contracture is corrected with the one-size thicker PE, I try the same procedure again with a two-size thicker PE. If the flexion contracture disappears with a two-size thicker PE, a constrained prosthesis is used since these findings indicate that the joint capsule or ligament tissues are unreliable for stability.
Custom-made prosthesis has fallen out of favor since the modular type component has been introduced. APC (allograft prosthesis composite) can be used when there is a severe bone defect, but the junction with the host bone site may not be well united, and infection may occur more frequently. Therefore, it would be more convenient and safer to use the tumor prosthesis rather than the APC in the patient with a severe bone defect.
In patellar revision, biconvex prosthesis, inset patella, or trabecular metal augment can be considered when there is a severe cavitary defect.
9.2.2.2 Approach
The most important surgical step in revision TKA is the approach. Wound edge necrosis and extensor mechanism rupture are the most critical complications that can adversely affect the outcome of revision TKA. If the approach is insufficient and lateral traction or eversion of the patella cannot be achieved, revision TKA cannot be performed properly and it is highly likely to fail. Harwin recommended brisement before skin incision in patients with ankylosed knee. Approach varies based on the previously used approach, soft tissue coverage, deformity, and joint motion, but it is recommended to use the same approach as that used in primary TKA. However, the subvastus approach should be avoided even though it has been used before. If problems with the skin and/or soft tissues are suspected, a plastic surgeon should be consulted in advance. If excessive tension in the skin is expected, tissue expanders may be used before revision TKA. Arthrotomy is done along the previous incision line if there is remaining suture material.
If the patient has good preoperative range of motion, a routine medial release allows the tibia to be rotated externally and subluxated anteriorly, which is usually sufficient for exposure. If there is contracture of the ligamentous tissues, it is necessary to release the tissues en bloc. The medial contracture may require release up to the whole superficial MCL, pes anserinus, and semimembranosus tendon, thereby allowing anterior translation and external rotation of the tibia so that the tibia can be exposed as much as possible. If there is a lateral contracture, the iliotibial band, joint capsule, and popliteus tendon may be released step by step.
If exposure is not enough for revision arthroplasty using the above methods, ancillary procedures for the quadriceps mechanism such as rectus snip, V–Y quadricepsplasty, tibial tubercle osteotomy, or subperiosteal peel can be performed subsequently.
Author’s Method

I believe that the approach is the most important factor in revision TKA. If the patella is not everted or laterally retracted during revision TKA, the exposure will be limited and the surgical procedure will be restricted.
In order to do patellar eversion, hypertrophic fibrous tissues on the lateral side of the quadriceps and patella tendon is removed completely and adhesiolysis is done as well in advance. On careful observation, I can easily define the junction between tendinous and fibrous tissue. Once this is done, the patella can be everted or laterally retracted in most of the cases (Fig. 9.1). During eversion of the patella, the patellar tendon may be stripped off or an avulsion fracture may develop. I use a protector or mini plate to prevent this occurrence. I had used the rectus snip approach to ensure an adequate operation field until I developed this technique. But I have not needed any ancillary procedures to the quadriceps tendon ever since I used this technique.
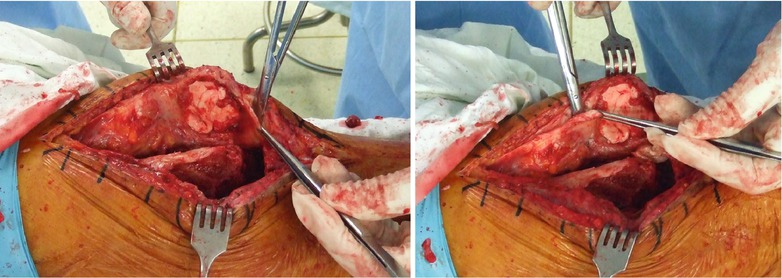
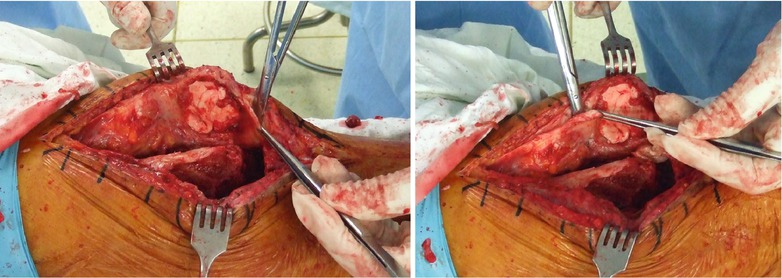
Fig. 9.1
Removing the hypertrophic fibrous tissues from patella tendon (a) and quadriceps tendon (b) Thick fibrous tissue should be removed
9.2.2.3 Implant Removal
Implant removal is an even more critical procedure during revision TKA. If it is done with less amount of bone loss, the subsequent procedure becomes easier and the operation has good prognosis. Hence, implant removal should be done carefully in order to minimize the bone loss.
For easy removal of the implant, sliding hammer, microsaw, Gigli saw, diamond-tipped drill, etc., should be kept ready. At first the PE is removed. There is usually no problem while removing the snap-fitted PE, but it is sometimes necessary to cut the PE which was fixed with screws or metal rod. After removal of the PE, the femoral, tibial, and patellar prostheses are removed in that order. It is technically more difficult to remove the tibial prosthesis first and the tibial bone might be injured while removing the femoral prosthesis. Patellar component is removed lastly because removing the patellar component first may weaken the patella and a patellar fracture may occur during the subsequent surgical procedures.
Microsaw is more recommended than Gigli saw for separating the prosthesis from the bone. Gigli saw can separate only the anterior portion of the femur, it can cause too much bone loss at the chamfer area and may cause contamination as the handle portion of the Gigli saw can get easily slipped off (Fig. 9.2). On the other hand, microsaw can reach almost all areas except for the posterior portion of the prosthesis. So, the use of microsaw can minimize the bone loss and it is also convenient to use (Fig. 9.3).

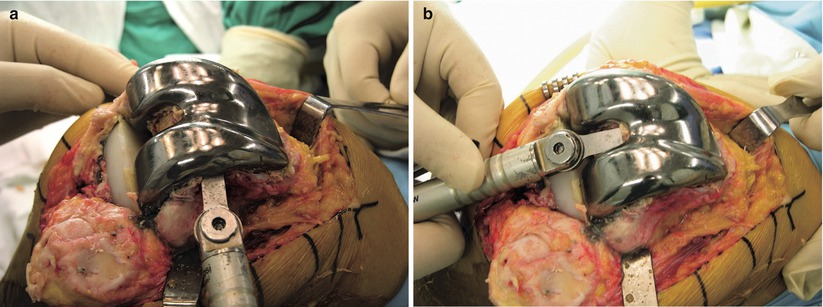

Fig. 9.2
Separating the prosthesis using a Gigli saw
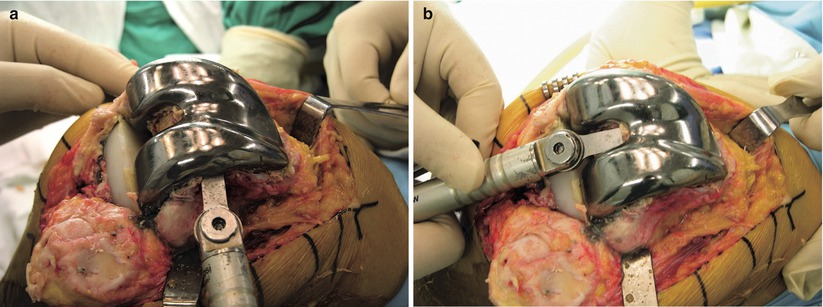
Fig. 9.3
Separating the prosthesis from the bone using a microsaw. The distal (a) and notch area (b) is separated
Finally, an extractor is used to remove the prosthesis. If the stem does not come out, a window can be made in the anterior cortex of the femur. In the tibia, a window can be made in relation to the tibial tubercle osteotomy.
Author’s Method

My method of implant removal is different from the others. It is a very simple and effective technique and it reduces the amount of bone loss. First, I drill a hole to make a mark at around 5–6 cm proximal to the joint line on the lateral side of the femoral metaphysis before removing the femoral prosthesis and measure its distance from the joint line. Even in revision TKA, the height of the femoral prosthesis is usually maintained. So this hole is used as the index of the joint line which is one of the most important points of the surgical technique for revision TKA (Fig. 9.4). After making a mark, I remove the fibrous tissues around the femoral prosthesis using a knife or a thin osteotome to define the boundaries.
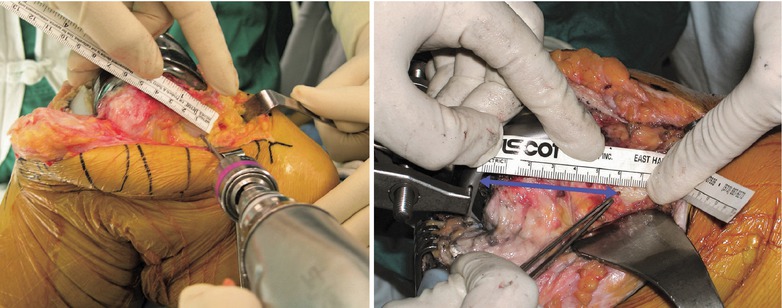
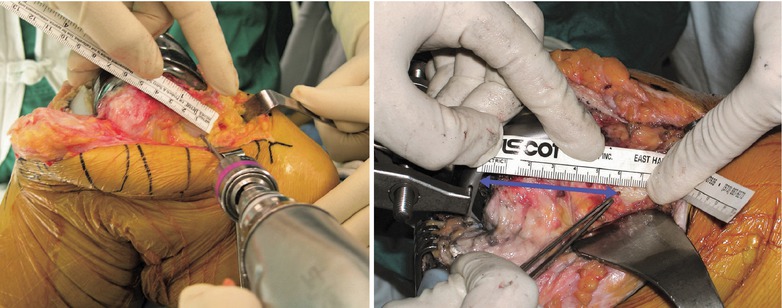
Fig. 9.4
The method to maintain the joint line. The left image shows a marking about 5–6 cm proximal to the joint line before removing the prosthesis. The right image shows the technique of measuring the size of bone defect after inserting a trial implant up to the marked level
I use a microsaw to separate the prosthesis from the bone, and then instead of using an extractor, I tap the medial and lateral sides alternately with a hammer. The seesaw effect helps to separate the prosthesis from the bone. Then, I use an impactor to tap the anterior flange of the femoral prosthesis. This makes it easy to remove the prosthesis as it has already been separated. In this manner, the prosthesis can be removed with almost no bone loss (Fig. 9.5).
While removing the tibial component, the anterior and medial sides are separated using a microsaw, while the lateral and posterior sides are separated using a Gigli saw. Again, the mediolateral and anteroposterior sides are tapped alternately with a hammer and impactor (Fig. 9.6). While removing the prosthesis, the tibial plateau can get compressed if the osteotome is used as a lever. Hence, I use the extractor or impactor in the reverse direction. In the modular type, it is sometimes easier to separate the tibial plate and the stem first. After removal of the tibial plate, the stem is separated from the bone with a gouge and is removed.
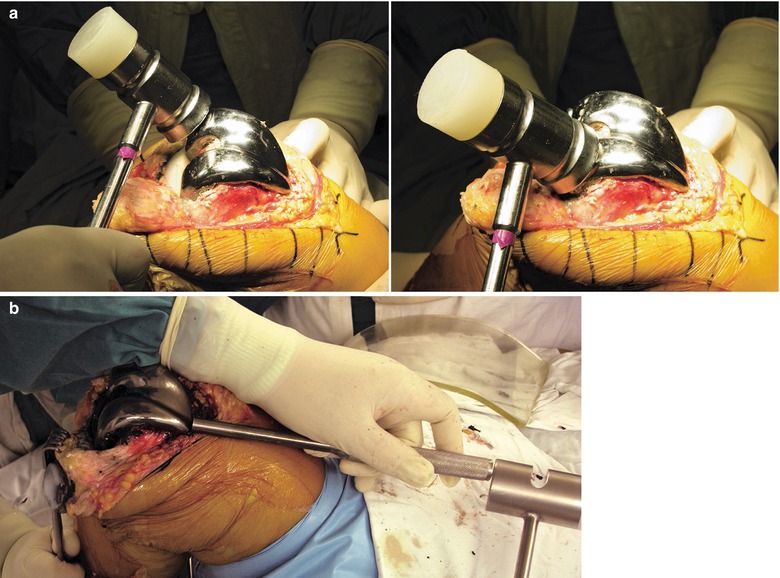
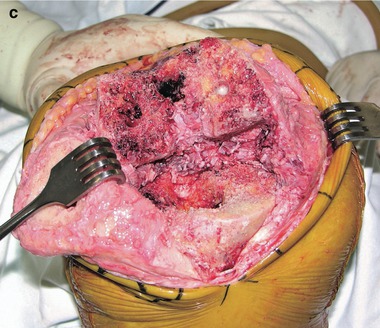
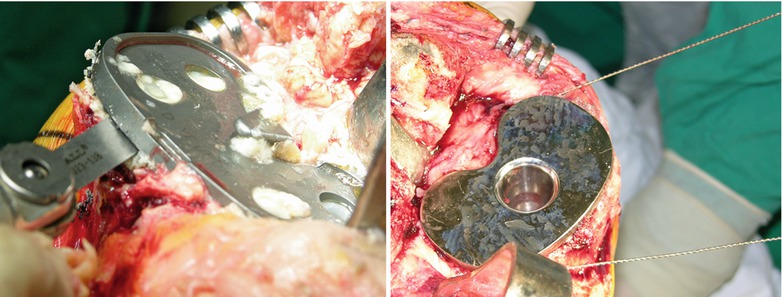
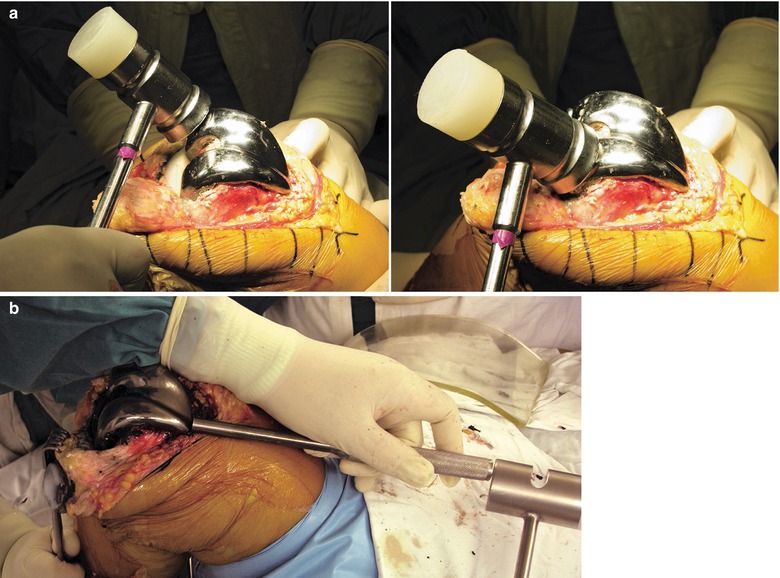
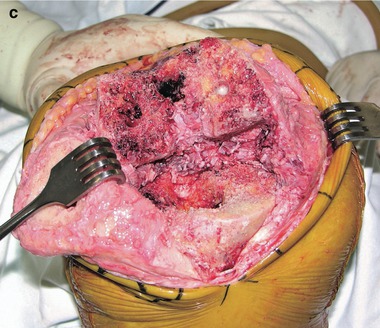
Fig. 9.5
Method of removing the femoral prosthesis. (a) Separating the femoral prosthesis from the bone by tapping the medial and lateral sides alternately with a hammer. (b) Removing the prosthesis with an impactor. (c) After removal of the prosthesis using my technique (There is almost no bone loss after removal of the prosthesis.)
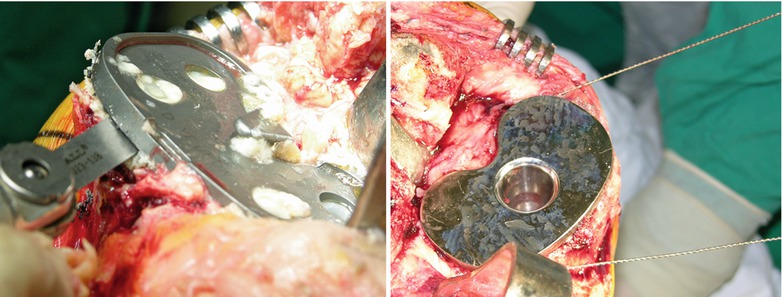
Fig. 9.6
Method of removing of tibial component. Left: Anterior portion is separated using microsaw. Right: Posterior portion is separated by Gigli saw. Next procedure is same with removal of femoral prosthesis
Removal of the patellar component is done in the end. The patella is removed by stripping off the fibrous tissues and bony overgrowth from margins of the prosthesis and followed by separating the prosthesis from the bone using a microsaw. And then I remove the patellar component using an osteotome and the instrument that I have designed (Fig. 9.7). In a metal-backed patella, I remove the PE first to see the outline of the metallic component. I sometimes cut the lugs using Midas Rex (Medtronic, Minneapolis) and then dig them out. Since the removal of the patellar component is likely to cause a fracture due to excessive bone loss, I take special care to prevent this occurrence.
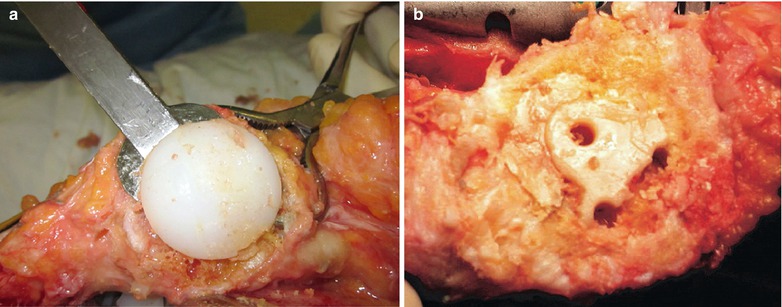
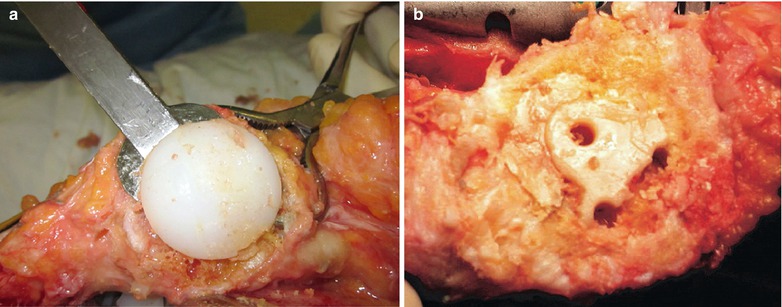
Fig. 9.7
Method of removing the patellar prosthesis using patella remover (a) and after its removal (b)
After removal of the prosthesis, it is recommended to remove the remaining bone cement. In aseptic revision TKA, cement may not be removed if its removal causes a large bone defect. But in septic revision, all the cement should be removed as the cement may be the source of infection. The reamer can be used to remove the cement from the medullary canal. While reaming, care should be taken so that the reamer does not perforate the cortex of the tibia instead of reaming the cement. This happens sometimes because the cement is too hard. If the cortex of the tibia is perforated, the neurovascular structures in the calf are likely to be injured. Therefore, it is recommended to use C-arm to check whether reaming is done correctly (Fig. 9.8).
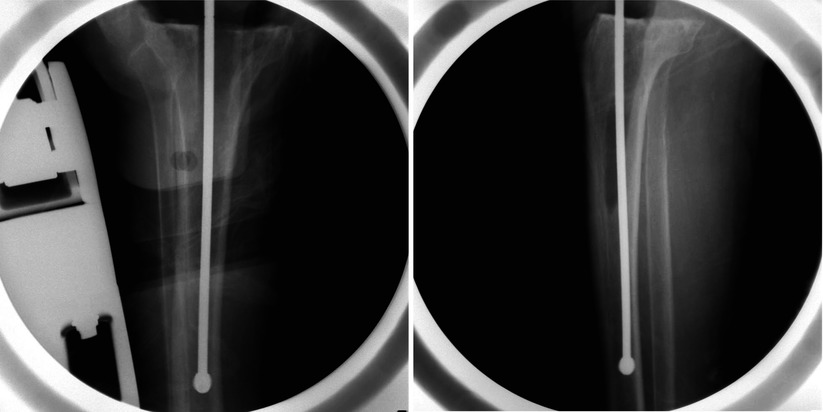
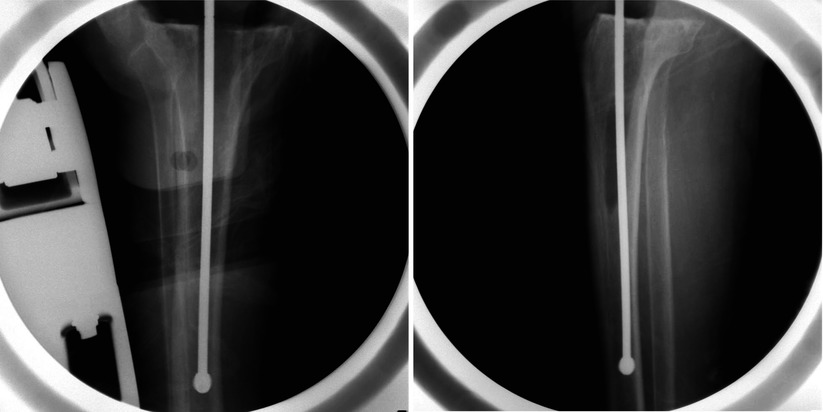
Fig. 9.8
Use a C-arm to check whether the medullary reamer is in its correct position or not. The reamer is located in the medullary canal
After removal of the cement from the medullary canal, the fibrous membrane on the inner surface of the bone and intramedullary canal should be curetted completely until the healthy bone is exposed in order to improve fixation of the prosthesis.
9.2.2.4 Soft Tissue Treatment
If wear has extended to the metal, synovium and soft tissues are stained black due to metallosis (Fig. 9.9). Even a small amount of metal debris can stain the bone, and hence it needs to be excised meticulously. In most cases, however, such meticulous excision is impossible as it is dangerous to the neurovascular system and it can be found outside of the joint. In revision for loosening or osteolysis, the color of the synovium may have changed to a grayish shade. This is the osteolysis phenomenon caused due to the PE particles rather than metallosis and these particles must be removed meticulously. As the synovial membrane is adhered to the surrounding soft tissues and the joint capsule is weak, caution is needed to prevent a neurovascular injury while performing debridement of the posterior synovial membrane and the capsule.
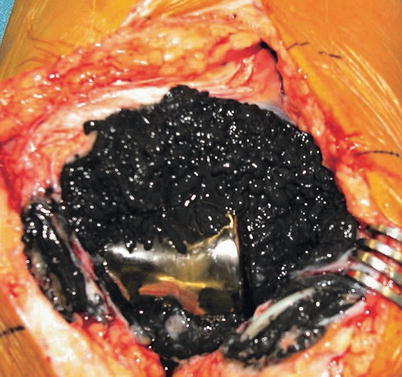
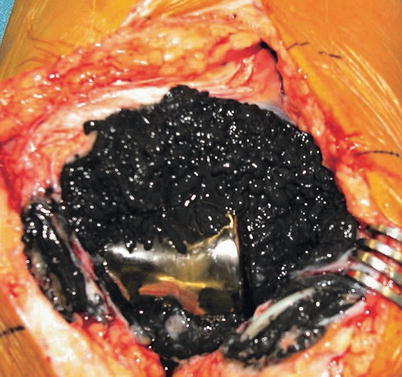
Fig. 9.9
Black colored soft tissue and synovium due to metallosis
After synovectomy, the hypertrophic fibrous tissues in the supracondylar area of the femur should be removed. If these tissues are not removed, they will worsen the patellar alignment, restrict flexion motion, and interfere with skin closure. Therefore, fibrous tissues in the supracondylar area must be removed without any hesitation not only for improving the extensor mechanism but also for achieving a better ROM.
9.2.2.5 Osteotomy and Bone Reconstruction
Removal of the prosthesis is followed by bone reconstruction and soft tissue balancing. The basic principle of revision arthroplasty involves maintaining the joint line and performing a kinematically stable arthroplasty that is well fixed and well aligned.
The causes of bone defect noted during revision TKA are infection, loosening, osteolysis, stress shielding, instability, etc. The bone defect becomes larger during removal of the implant.
Bone defect should be reconstructed by any method which achieves stability of the prosthesis and balancing of the knee joint. In the femur, maintenance of the joint line is strongly related to the amount of reconstruction. If the extension gap is narrow in an adequate flexion gap state, the joint line can be elevated by 4–5 mm using the PS type of prosthesis. Vince stated that it is much more important to establish the extension and flexion gap balance, ligament balance, and prosthesis fixation rather than retaining the joint line in revision TKA. An excessive tibial osteotomy weakens the bone that supports the prosthesis and a smaller prosthesis with a thicker PE may be required. Therefore, the bone defect should be reconstructed as much as possible. General principles of bone reconstruction are described in Sect. 5.1, and hence, surgical techniques for each part are briefly described here.
Tibia
The tibial bone reconstruction is the foundation of revision arthroplasty because the level of tibial osteotomy affects both the extension and flexion gaps. Hence, I will describe the tibial procedure first. Intramedullary method is strongly recommended for alignment and reconstruction of the tibia because an extension stem needs to be inserted in many cases, and the amount of resection increases when bone resection is performed by using the extramedullary method since additional bone cutting is needed more frequently. As the tibial component is usually perpendicular to the extension stem, the posterior slope of the tibia should be 0°. If the posterior slope is between 3 and 5° just like in primary TKA, the posterior portion of the tibial prosthesis does not make any contact with the bone when an extension stem is used. The size of the prosthesis and the length and diameter of the extension stem are chosen, and the medullary canal is reamed. After osteotomy, the center of rotation is determined. A little more external rotation is preferable for better patellar tracking. When bone grafting has been performed, the tibial prosthesis tends to be inserted in an internally rotated state if the rotation has been matched with the shape of the bone graft. To prevent this occurrence, the rotation should be checked with the tibial tuberosity as a landmark.
Femur
In femoral reconstruction, the first step is to determine the size of the femoral prosthesis. Since bone loss has occurred in the anterior or posterior portion of the femur while removing the prosthesis, many surgeons tend to make a mistake of choosing a smaller prosthesis. With respect to the prosthesis size, the A–P length is more important than the width. The size of the prosthesis that is removed, the contralateral X-rays, and the flexion gap may be helpful to determine the prosthesis size. A larger prosthesis is chosen if the flexion gap is wide and a smaller prosthesis is chosen if it is narrow.
Correct rotation of the femoral component is utmost important. If the rotation of the remaining bone is not aligned with the epicondylar axis, one side of the posterior condyle can be resected more and the other side may need metal augmentation for achieving correct external rotation. As there are many incidences of bone loss at the epicondylar area, it is convenient and reasonable to use the gap technique for determining the femoral rotation.
The next step is reaming the medullary canal and osteotomy is done as per the manual for each prosthesis. As most of cases have anterior bony defect, there is a tendency to set the reaming point on the posterior side. In such a case, the prosthesis is inadvertently inserted with anterior angulation when an extension stem is used. On the other hand, too little reaming of the posterior portion increase the size of prosthesis and the anterior gap between the prosthesis and the bone. In such a situation, it is not recommended to use a prosthesis that is too large, and hence, it needs to be decided whether to lower down the reaming point, whether to use an offset stem, or to insert the prosthesis at a slight anterior angulation. When the extension stem is already attached, the axis of distal osteotomy should be same with the stem axis of the prosthesis which is fixed between 5 and 7° in the coronal plane.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








