Revision Anterior Cruciate Ligament Reconstruction
David R. McAllister
Kristofer J. Jones
Frank Petrigliano
DEFINITION
The anterior cruciate ligament (ACL) is the primary stabilizer preventing anterior displacement of the tibia. The ligament is composed of two functional bundles, namely the anteromedial and posterolateral bundles. These bundles are named after the position of their insertion site on the tibia.
The ACL plays a significant role in assisting capsular structures, the collateral ligaments (ie, medial collateral ligament [MCL] and lateral collateral ligament [LCL]), joint surface, and meniscal geometry to prevent rotational instability.
Failure of a primary ACL reconstruction may be due to traumatic rerupture, graft attenuation, failure of graft incorporation, failure to diagnose and treat concomitant injuries (ie, posterolateral or posteromedial corner injuries), or technical errors during primary ACL reconstruction (ie, tunnel malposition, loss of graft fixation, etc.; see Chap. 50).
ANATOMY
The anatomy of the ACL (described in previous chapters) and also that of the secondary stabilizers of the knee are critical in revision surgery. Secondary restraints to anterior translation of the tibia include the MCL, the posterior horn of the medial meniscus, and the posterior aspect of the capsule.6
Unrecognized rotatory instability patterns play a significant role in failures of primary ACL reconstruction.
Primary ACL reconstruction can be performed using a number of different graft sources, including autograft bone-patellar tendon-bone, hamstring, and quadriceps tendon. Allograft sources include bone-patellar tendon-bone, Achilles tendon, hamstring, anterior tibialis, and quadriceps tendon.4
Synthetic graft sources have been investigated; however, these materials have demonstrated poor clinical outcomes and high reoperation rates due to recurrent pain, synovitis, joint effusion, and ultimately, graft failure.
Graft fixation can be achieved with a number of commercially available devices. In the revision setting, it is important to understand the technique and materials used in the initial reconstruction because it is often necessary to remove existing fixation devices to obtain optimal tunnel placement and secure graft fixation during the revision procedure.
PATHOGENESIS
Poor clinical outcomes following primary ACL reconstruction can be due to a multitude of factors. Primary surgical failure can be generally classified into one of four areas, including recurrent instability, motion loss, persistent pain, or extensor mechanism dysfunction. This chapter will focus on the diagnosis and surgical management of recurrent instability.
The incidence of recurrent instability after primary ACL reconstruction is 3% to 10%.11
Graft failure has been reported as the primary cause of recurrent instability. Three different categories of graft failure have been described: (1) failure of graft incorporation, (2) suboptimal surgical technique (eg, tunnel malposition, loss of fixation), and (3) traumatic rerupture. Although recurrent instability may be due to a combination of these factors, it is important to determine the primary mode of failure in order to address this issue during revision reconstruction.
NATURAL HISTORY
The natural history of the ACL-deficient knee is not well understood.
It is commonly thought that patients who experience episodes of recurrent instability may place the knee at risk for potential damage to the articular cartilage and menisci.
Although it may be possible for some patients to avoid activities that result in instability, others may continue to participate in sports, and some patients may even experience episodes of instability with activities of daily living.
PATIENT HISTORY AND PHYSICAL FINDINGS
A detailed history of the primary mechanism of injury, associated pathology, reconstruction technique, postoperative rehabilitation, ability to return to activity, and current symptoms are helpful to determine potential reasons for failure and subsequent optimal treatment.
It is helpful to determine the time from the initial injury to the index reconstruction.
An explanation of the postoperative rehabilitation program and timing of progression through therapy should be obtained (ie, time to return to running and sport-specific activities). Any traumatic episodes after surgery should be noted.
A copy of the operative report from the primary procedure should be obtained to note graft type, tunnel placement, fixation methods and materials, and condition of the articular surfaces and menisci at the time of the procedure.
An antalgic gait may be the result of persistent pain after surgery or a recent second traumatic event.
A varus thrust during gait is highly suggestive of incompetence of the lateral or posterolateral structures and requires further evaluation with standing long-film anteroposterior radiographs to determine mechanical alignment.
Buckling of the knee, especially in the initial phase of gait, may suggest quadriceps weakness and may give the patient the subjective sensation of knee instability.
Common examinations to determine instability patterns of the knee include the following:
Anterior drawer test: When compared to the contralateral knee, increased anterior laxity may indicate an ACL-deficient knee.
Posterior drawer test: When compared to the contralateral knee, increased posterior laxity may be indicative of a posterior cruciate ligament (PCL)-deficient knee.
Lachman test: This is a sensitive test for ACL deficiency, especially when the contralateral knee has an intact native ACL.
Varus/valgus stress testing: Increased joint space widening at 30 degrees of flexion is consistent with injury to the collateral ligaments. If joint space opening occurs in both 0 and 30 degrees, severe injury to collateral ligaments and other ligamentous structures, such as the cruciate ligaments or capsule, is suggested.
Pivot shift: This is a highly sensitive test for ACL deficiency.1 It is a complex, multiplanar maneuver that includes coupled translation (the anterior subluxation of the lateral tibia followed by its reduction) and rotation (rotation of the tibia relative to the femur). It is often difficult for the patient to relax in the setting of a painful knee, however.
Posterolateral drawer test: Increased posterolateral translation compared with the intact, contralateral knee may suggest posterolateral rotatory instability.
Dial test: A difference of more than 10 degrees at 30 degrees of flexion is consistent with injury to the posterolateral corner (PLC). A difference of more than 10 degrees at 90 degrees of flexion is consistent with a combined injury to both the PLC and PCL.
The varus recurvatum test reveals varus angulation, hyperextension, and external rotation of the tibia. A positive test suggests posterolateral rotatory instability of the knee.
Testing for intra-articular injuries should be performed to detect concomitant meniscal, articular cartilage, or patellofemoral injuries.
Large effusions are common in the setting of a native ACL tear. In the revision setting, graft disruption may not result in a large hemarthrosis given the decreased vascularity of the graft material compared to the native ACL. Effusions in the setting of a failed ACL reconstruction may be small or even nonexistent.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Routine radiographs, including weight-bearing anteroposterior and lateral views as well as patellar views, should be performed. In the revision setting, these images facilitate critical assessment of previous tunnel placement and evaluation of any bone loss at previous tunnel sites, which may require further evaluation and treatment.
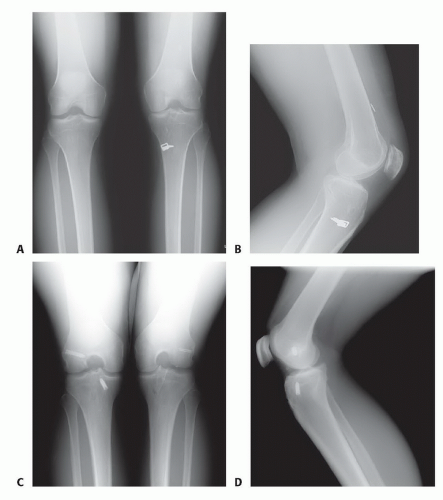
Metallic graft fixation devices make previous tunnel placement easy to identify, but bioabsorbable screws and other types of fixation can also be evaluated to determine tunnel placement on these images (FIG 1). These images also facilitate evaluation for possible evidence of osteoarthritis.
If concern regarding a significant amount of bone loss is present after initial radiographic evaluation, three-dimensional imaging with computed tomography (CT) scan or magnetic resonance imaging (MRI) can facilitate precise quantification of tunnel enlargement (FIG 2). MRI may also aid in the evaluation of tunnel size, graft continuity, and the status of other intra-articular structures (eg, articular cartilage, menisci). Metallic graft fixation devices may create significant artifact on both of these imaging techniques, thus limiting their use in some cases.
For varus alignment, or chronic posterolateral rotatory instability, radiographs that facilitate evaluation of mechanical alignment may be necessary. These will help the surgeon to determine whether there is a significant varus deformity of the knee.
In ACL-deficient knees with varus malalignment, any ligament reconstruction may be predisposed to gradual attenuation and eventual failure if the alignment is not first addressed with an osteotomy procedure.
Bone scan and serologic tests, including complete blood count, erythrocyte sedimentation rate, C-reactive protein, and bacterial cultures of knee aspirates, should be performed in any case that is suspicious for infection, including those cases with significant osteolysis of previous tunnels.
DIFFERENTIAL DIAGNOSIS
Meniscal injury
Osteochondral injury
Subjective weakness or anterior knee pain secondary to quadriceps weakness
Patella subluxation or dislocation
Multiligamentous injury (eg, PCL, PLC, MCL, LCL)
NONOPERATIVE MANAGEMENT
Patients with complaints of knee pain in the setting of a nonfunctioning ACL graft must understand that revision ACL reconstruction will not alleviate their pain and that
nonoperative management may be a better approach to address their symptoms.
The basis of any nonoperative treatment approach for an ACL-deficient knee is to avoid those activities that put the knee at risk, such as cutting and pivoting sports.
Strengthening the dynamic stabilizers of the knee such as the hamstrings (an antagonist to anterior translation of the tibia) may increase stability of the knee for routine activities.
Functional bracing is a nonoperative treatment alternative to provide kinematic restraint, reduce functional deficits, and prevent subsequent injury. However, it has variable success in controlling instability.
SURGICAL MANAGEMENT
Revision ACL reconstruction is primarily indicated in any patient with a chief complaint of symptomatic knee instability during physical activity. It is important to review the following expectations of revision surgery with the patient:
Revision ACL reconstruction does not address pain that may be experienced with physical activity. In these patients, contributing intra-articular pathology should be investigated as the cause of subjective pain.
Revision ACL reconstruction may prevent the progression of intra-articular pathology but will not, in itself, treat other lesions that may be present.
In general, the subjective outcomes following revision ACL reconstruction are inferior to primary ACL reconstruction.
Preoperative Planning
A common cause of failure related to surgical technique is anterior placement of a femoral tunnel, which can be detected on the lateral radiograph (FIG 1D).6 This may lead to excessive tightening of the graft with knee flexion, thus leading to graft attenuation and subsequent failure.
A preoperative plan should take all of the preoperative findings, including patient history, examination, and imaging for other intra-articular pathology, into consideration. The surgeon should be prepared to address these comorbidities at the time of revision surgery.
Even if the surgeon does not expect to discover additional pathology at the time of revision surgery, it is important to be prepared to address any concomitant findings. All treatment options must be covered in detail during preoperative discussions with the patient.
In the setting of possible posterolateral rotational instability, varus malalignment, or significant bone loss requiring bone grafting, the patient must be aware of the potential decision to perform a staged procedure, and the details of alterations in the postoperative course should be discussed preoperatively.
The possibility of hardware removal requires knowledge of any previous implants used and extraction tools, such as a commercially available ACL revision tray, should be available in the operating room at the time of surgery.
Once anesthesia has been induced, a thorough examination of the knee relative to the contralateral extremity is critical. Concerns regarding posterolateral or varus instability will not be answered during arthroscopic evaluation and are best assessed prior to prepping and draping.
Positioning
We prefer to position the patient supine on the operating room (OR) table and use a lateral post throughout the case.
The lateral post should be placed proximal enough to ensure the surgeon has unobstructed access to tibial tunnel drilling when the patient’s knee is flexed over the edge of the table (FIG 3).
Approach
The standard anteromedial, anterolateral, and superolateral outflow portals are used for diagnostic arthroscopy.
If the previous incisions were adequately positioned, they may be used, but the placement of portal incisions should not be compromised for the sole purpose of reusing the previous incisions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree