Injuries to the cervical spine during sports are relatively common, depending on the specific sport. Given the adjacent neurovascular structures, any injury to the cervical spine must be evaluated with caution to assess its severity. With proper management, most injuries resolve quickly and allow for rapid return to play (RTP). The purpose of this article is to synthesize the current literature on the most common cervical spine injuries in athletes, including injury prevalence, mechanisms of injury, and RTP decision-making processes.
Key points
- •
Describe typical mechanisms of injury for common cervical vertebral fractures.
- •
Understand the contribution of electrodiagnostic medicine to return to play considerations in stingers.
- •
Describe controversies in both screening for cervical stenosis in the athletic population and management of athletes with cervical injuries and identified stenosis.
- •
Know relative and absolute contraindications for return to play following cervical disc herniation.
Introduction
Cervical spine injuries are significant concerns in the athletic population, and they can occur with a variety of mechanisms and severities. Although catastrophic sports-related cervical spine injuries are relatively rare, they have been reported in multiple contact and noncontact sports, including American football, rugby, wrestling, hockey, recreational diving, horseback riding, skiing, and snowboarding. Sports injuries were the fourth most common cause of spinal cord injury (SCI) in the United States between 2005 and 2010, after motor vehicle accidents, violence, and falls, and are the second most common cause of SCI in the first 30 years of life.
Noncatastrophic injuries of the cervical spine occur with even greater frequency. These less grave injuries are typically amendable to functional rehabilitation and return-to-play (RTP) for the affected athlete. Although some cervical spine injuries have clearer guidelines, RTP decisions for many cervical injuries remain controversial. Authors have proposed criteria to guide RTP decision-making in cervical spine fractures, stingers, cervical stenosis and cervical cord neuropraxia (CCN), and herniated nucleus pulposis. However, the relative infrequency of these injuries has limited the ability to perform randomized clinical trials, elucidate their epidemiology and risk factors, or produce validated outcomes measurements. Much of the current RTP guidelines are based on retrospective case series and expert opinion pieces.
The general principles that guide RTP decision-making, namely being free of pain with full range of motion (ROM) and normal or near-normal strength, are not unique to injuries in the cervical spine. However, because of the presence of adjacent neurovascular systems, team physicians, trainers, and parents must proceed with care in deciding when an athlete may return to the field. This article attempts to aggregate both the current published literature and the clinical experience of field leaders in the recommendations that follow.
Introduction
Cervical spine injuries are significant concerns in the athletic population, and they can occur with a variety of mechanisms and severities. Although catastrophic sports-related cervical spine injuries are relatively rare, they have been reported in multiple contact and noncontact sports, including American football, rugby, wrestling, hockey, recreational diving, horseback riding, skiing, and snowboarding. Sports injuries were the fourth most common cause of spinal cord injury (SCI) in the United States between 2005 and 2010, after motor vehicle accidents, violence, and falls, and are the second most common cause of SCI in the first 30 years of life.
Noncatastrophic injuries of the cervical spine occur with even greater frequency. These less grave injuries are typically amendable to functional rehabilitation and return-to-play (RTP) for the affected athlete. Although some cervical spine injuries have clearer guidelines, RTP decisions for many cervical injuries remain controversial. Authors have proposed criteria to guide RTP decision-making in cervical spine fractures, stingers, cervical stenosis and cervical cord neuropraxia (CCN), and herniated nucleus pulposis. However, the relative infrequency of these injuries has limited the ability to perform randomized clinical trials, elucidate their epidemiology and risk factors, or produce validated outcomes measurements. Much of the current RTP guidelines are based on retrospective case series and expert opinion pieces.
The general principles that guide RTP decision-making, namely being free of pain with full range of motion (ROM) and normal or near-normal strength, are not unique to injuries in the cervical spine. However, because of the presence of adjacent neurovascular systems, team physicians, trainers, and parents must proceed with care in deciding when an athlete may return to the field. This article attempts to aggregate both the current published literature and the clinical experience of field leaders in the recommendations that follow.
Cervical fractures
Cervical spine fractures may occur by a variety of mechanisms in the athletic population. They vary greatly in severity depending on the location of fracture, extent of involvement of adjacent neurovascular structures, and time required for bone healing. In the 2012 assessment of spine injuries in National Football League (NFL) players from 2000 to 2010, the spectrum of cervical fractures occurred with the lowest frequency, 1.8% of all cervical injuries, but carried the longest mean number of days lost at 119.7 days. Tator and colleagues described 188 cervical fractures and/or dislocations in competitive ice hockey players between 1966 and 1993, 130 of which occurred without neurologic involvement.
Spinous process fractures are not uncommon forms of isolated cervical vertebral fracture and typically have a benign clinical course. They most commonly occur in the lower levels of the cervical spine and were described with 4 postulated injury mechanisms by Meyer and colleagues. The first mechanism involves avulsion of the spinous process by forceful co-contraction of trapezius, rhomboid minor, and/or serratus posterior muscles, the pattern of which is often referred to as “clay shoveler’s fracture ( Fig. 1 ).” Other injury mechanisms include hyperflexion-hyperextension whiplash injuries that have been observed in football, hockey, and gymnastics, as well as sharp direct blows to the spinous process, and avulsion injury associated with fracture/dislocation of the rest of the cervical spine.

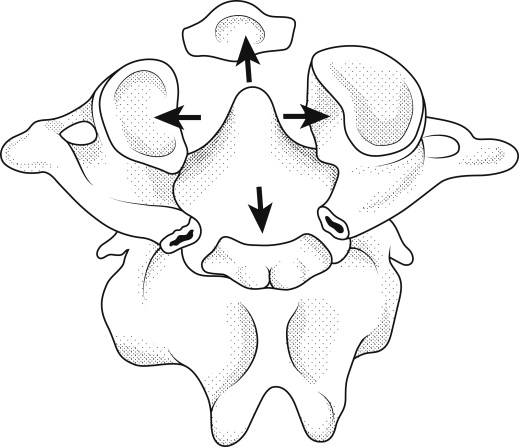
Jefferson described fractures of the C1 vertebrae following traumatic falls and direct cranial impact, with force transmission to the lateral masses from axial loading of head impact and continued torso momentum, with resultant fractures of the anterior and/or posterior vertebral arches ( Fig. 2 ). In the athletic population, inappropriate tackling technique with cervical flexion has been implicated in Jefferson C1 burst fractures in football and rugby players, as well as heads-first form checking into the boards in hockey players.
Compression fractures in the cervical spine are significantly less common than those in the thoracolumbar spine. Such injuries may happen sporadically in the athletic population, postulated as a result of hyperflexion forces in contact sports. The severity of the compression fracture may vary from mild deformation of superior or inferior endplate to significant anterior wedging of the vertebral body. Simple cervical compression fractures are typically benign in clinical course when properly identified, because they retain structural integrity of the anterior and posterior longitudinal ligaments as well as the posterior vertebral body. However, the mechanism of contact hyperflexion with higher magnitude forces may also result in more severe cervical fractures with posterior element involvement, often referred to as chance fractures; therefore, the clinician should proceed with caution when evaluating what appears to be an isolated cervical compression fracture ( Fig. 3 ).
A combination of cervical axial loading with flexion or distraction may result in more catastrophic cervical spine fractures with failure of 2 spinal columns and resultant involvement of the spinal cord. Classically, posterior element collapse is followed by anteroinferior fragmentation of the vertebral body, known as a teardrop fracture ( Fig. 4 ). However, there are multiple possible patterns of ligamentous and bony injury with 2-column instability, such as burst fractures with retropulsion involvement of the spinal canal and facet dislocation/distractions. In such cases, the degree of neurovascular involvement and resultant functional limitations will dictate treatment options and RTP decision-making.
Because of the necessity for completion of bone healing in simple cervical fractures without neurovascular compromise, no such injured athlete should return to full competition before a minimum of 8 to 10 weeks. Most fractures, including those only involving the spinous process, will require at least semi-rigid cervical collar immobilization until pain free. Once pain-free, the collar can be discontinued and a gradual resumption of ROM activities and subsequent cervical rehabilitation program that progresses to sports-specific activities can be engaged. Once pain-free, it is also recommended to obtain dynamic (flexion/extension) lateral radiographs of the cervical spine to assess cervical stability. The necessity of dynamic imaging may be illustrated by the Mazur and Stauffer discovery that 6 of 27 patients with isolated compression fractures of the cervical spine exhibited instability on follow-up radiographs.
Permanent avoidance of return to contact sports following some cervical fractures may be prudent when limitations from the initial injury persist or risk of additional injury is significantly increased. Such cases include atlanto-occipital and/or atlanto-axial fusion or instability, dynamic subaxial instability defined as greater than 3.5 mm translation or greater than 11° of angulation, multilevel fusions, and/or significantly limited cervical ROM. Diagnosis of spear tackler’s spine, which is the reversal of cervical lordosis and evidence of prior vertebral injury in a football player who has been confirmed to use a head first, or “spearing,” tackling technique is also an absolute contraindication to resumption of contact sports participation. Relative contraindications of RTP following cervical fracture include healed fractures of the C1-C2 complex such as type 1 or type 2 odontoid fracture and nondisplaced Jefferson fracture, minimally displaced compression fractures, and 1-level to 2-level posterior fusions.
Stingers
Cervical “Stingers” or “burners” are one of the most common sports-related injuries to the cervical spine and have perhaps the most well-delineated body of literature for their epidemiology, pathophysiology, and RTP decision-making. They are the most common complaint for which college football players are referred to emergency departments and orthopedic clinics for cervical spine evaluation. The prevalence of stingers in college football players has been estimated between 15% and 65% over their collegiate seasons, with recurrent injuries reported in up to 87% of players. In an electrodiagnostic assessment of 185 upper extremity nerve injuries in athletes, 40 (21.6%) were diagnosed with stingers, 30 of which occurred in football players and 10 of which occurred in wrestlers. Stingers may well be underreported in cases with only transient or mild symptoms.
Stingers represent transient peripheral nervous system injuries typically caused by either concussion or tensile/stretch overload to the brachial plexus or its supplying nerve roots. They typically present as radiating upper extremity pain and paresthesias in a dermatomal distribution with myotomal muscle weakness following a tackle or blow to the neck. Electromyographic evidence of axonal damage has been localized in different cases to the levels of the roots, trunks, divisions, cords, and branches of the plexus ; however, they most commonly affect the C5 nerve root. Strength evaluation for athletes with these injuries must include C5 innervated muscles, such as the deltoids and biceps. Stingers are exclusively unilateral, and when similar symptoms occur bilaterally, the physician should immediately consider and evaluate for SCI. Pain symptoms in stinger injuries often resolve over the course of hours, but may persist for up to several days or longer. Myotomal weakness may persist after resolution of pain, and physicians may consider electrodiagnostic testing if it lasts for greater than 2 weeks, to determine the extent of axonal involvement.
An athlete who sustains a first stinger may return to play once symptoms of pain and weakness have resolved, and full ROM of the neck and shoulder are assessed. In many transient cases, this could occur as early as minutes after sustaining the injury, but if symptoms persist, the player should be withheld from competition until they resolve. If the athlete sustains a second stinger during the same season, it is proposed that he or she should be withheld from the remainder of that game but may return the following game only if all symptoms have completely resolved. A third stinger, regardless of symptom duration, necessitates radiological evaluation of the cervical spine to assess for neuroforaminal or uncovertebral stenosis that may predispose the player to repeat injuries, or disc herniation with atypical radicular presentation. Prolonged persistence of pain and/or weakness of any stinger requires electodiagnostic testing to guide RTP decision-making. Although a normal electromyography is not required for the athlete to return to play, absence of ongoing acute denervation (spontaneous potentials) with evidence of reinnervation (polyphasicity with appropriate recruitment) should be established before the athlete is returned to competition ( Table 1 ).







