(1)
Department of Orthopedic Surgery Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands
Abstract
Large talar cystic lesions located in the posterior talus can be treated by retrograde drilling through the posterior talar process. By means of a two-portal endoscopic approach of the hindfoot with the patient in the prone position, it is possible to visualize, debride, and graft these large cystic lesions. In this chapter, the etiology and treatment options are mentioned. The operative technique is described by means of two case reports.
Retrograde drilling for large talar cysts can best be performed from posterior.
By means of a two-portal endoscopic approach of the hindfoot with the patient in the prone position, it is possible to visualize, debride, and graft these large cystic lesions.
17.1 Introduction
Intraosseous ganglia are benign lesions which usually occur in the metaphysis or epiphysis of long bones, in the near proximity of a joint. The first description of an intraosseous ganglion comes from Fisk in 1949 (Fisk 1949). Since then, various authors have used different names, like subchondral bone cyst and synovial bone cyst (Crabbe 1966; Hicks 1956; Woods 1961). The cause of this diversity is the difference in interpretation of their etiology (Schajowicz et al. 1979).
Intraosseous ganglia have been observed somewhat more often in males than in females, predominantly in middle-aged adults. The lesions are most frequently located in the lower extremities, usually involving the distal tibia (Andrews et al. 1991; Nigrisoli and Beltrami 1971).
Patients present with intermittent pain, frequently increasing with activity. Sometimes local swelling is seen (Nigrisoli and Beltrami 1971). On X-ray, the lesion appears as a well-demarcated circular to oval radiolucent defect, outlined by a rim of sclerotic bone (Murff and Hisham 1994). In most reports curettage or excision of the lesion with destruction of the surrounding zone of sclerosis, along with bone grafting, is the treatment of choice. This method is quite effective, with approximately 7 % of the cases reporting recurrence of the lesion (Nigrisoli and Beltrami 1971).
17.2 Etiology
It is estimated that patients with intraosseous cystic lesions report a prior trauma in 10 % of the cases (Nigrisoli and Beltrami 1971). It is postulated that synovial fluid is being pumped under pressure into the adjacent bone through a transarticular crack caused by the initial trauma (Nigrisoli and Beltrami 1971). Other etiological theories that gained support are the proliferation of synovial rests (Murff and Hisham 1994), local vascular disruption (Woods 1961), aseptic necrosis, and local metaplasia (King 1956).
17.3 Treatment
The operative approach for treatment of posttraumatic cystic lesions in the talus can be difficult. Our preferred treatment of a large symptomatic intraosseous cystic lesion is retrograde debridement of the cyst with drilling of the cystic wall and the surrounding sclerotic bone and filling the defect with an autologous bone graft (Baker and Parisien 1996; Kleiger 1988; Stone and Guhl 1995). In cases where the cystic lesion cannot be reached by means of anterior arthroscopy or arthrotomy, a malleolar osteotomy has to be made to be able to treat the lesion (Özner 2001). A two-portal endoscopic approach offers an excellent alternative with obvious advantages (Van Dijk et al. 2000). The articular origin of the cyst can be identified under direct arthroscopic vision. A second portal makes it possible to probe and subsequently treat the lesion by debridement, retrograde drilling, and trans-trocar bone grafting.
17.4 Operative Technique
17.4.1 Introduction
The operative approach is by means of the standard two-portal hindfoot approach which is described in Sect. 12.4 in detail. The retrograde drilling is performed through the posterior talar process. The technique is explained by means of the following two case reports and illustrated in detail in Figs. 17.1 and 17.2 (Scholten et al. 2006).
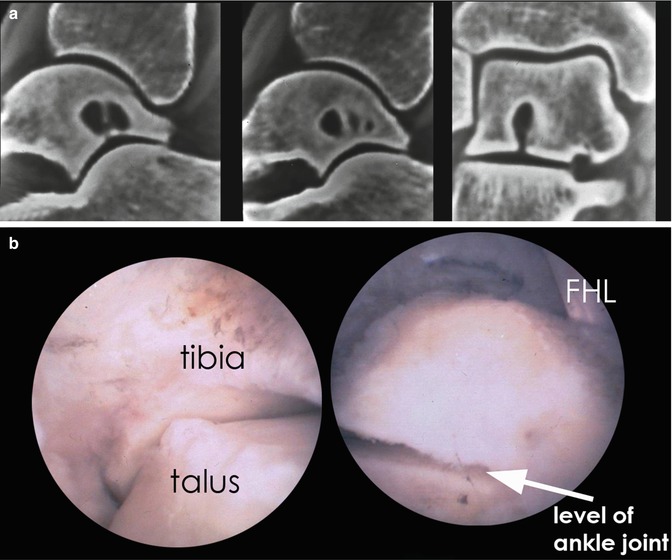
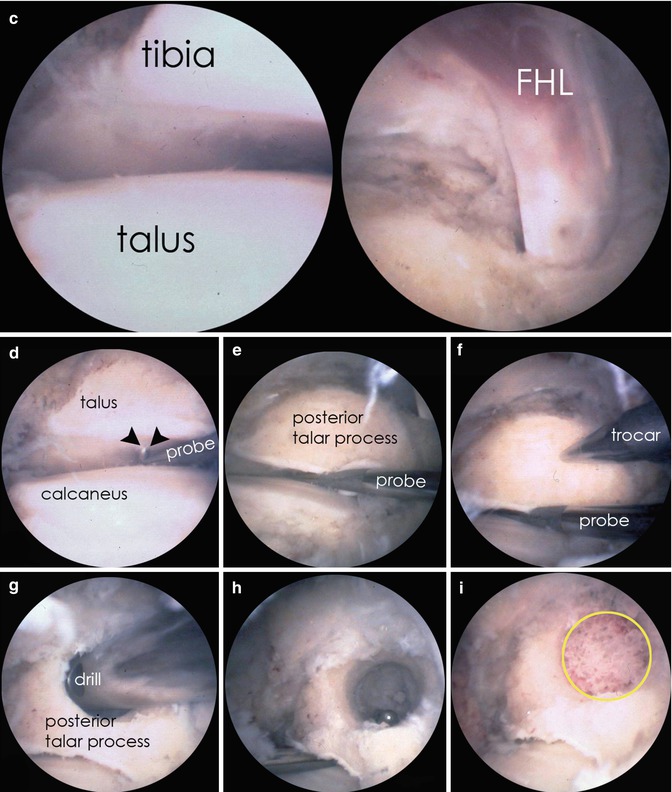
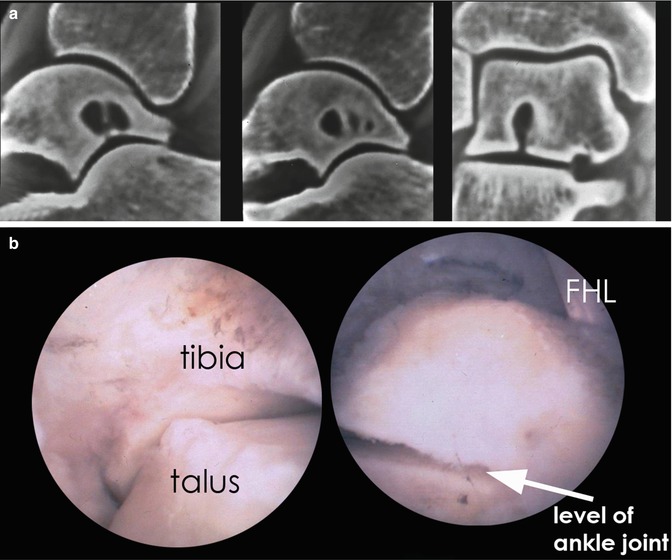
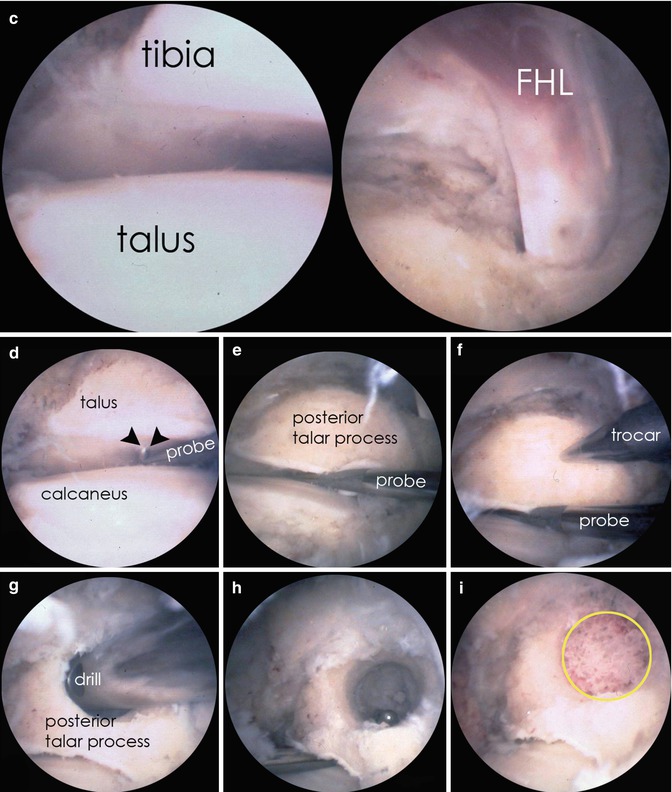
Fig. 17.1




Patient with deep ankle pain after axial trauma years before. Gradual increase in pain. On physical examination normal range of motion ankle joint, slight decrease range of motion subtalar joint. No local tenderness on palpation. X-ray shows no abnormality. CT scan shows intraosseous talar ganglion with opening towards subtalar joint. Retrograde drilling of this cyst was performed by means of two-portal hindfoot approach and retrograde drilling through the posterior talar process. (a) Two sagittal CT scan slices showing the multilocular intraosseous talar cyst with opening towards the subtalar joint. The coronal view is important for preoperative planning. The opening is in the center of the posterior calcaneal joint facet. (b) Patient in the prone position (left ankle). Scope is in the posterolateral portal looking anterior. Removal of fatty tissue and joint capsule subtalar joint by means of shaver. On the right we see the FHL and just lateral from it we see the ankle joint. The subtalar joint is clearly visible between the talus and calcaneus. (c) Same view as in 1B, but the scope has been brought in exactly at subtalar joint level. On the right the tendon of the FHL. We know from the preoperative frontal plane CT scan that the opening of the cyst is located exactly in the center of the joint surface (see a). (d) The arthroscopic hook is brought in the subtalar joint, and the tip of the hook (arrows) palpates the defect in the subchondral bone. (e) Now that the opening of the cyst is located, we know that the cyst is directly superior from the tip of the probe. If we now create a drill hole in the posterior talar process and place the drill parallel to the probe, the drill will exactly end up in the cyst. (f) The cannula with blunt trocar (4.5-mm diameter) is placed through the same posteromedial portal as through which the probe is placed. This ensures that the cannula is parallel to the probe. The blunt trocar is replaced by a 4.5-mm drill and a hole is drilled in the posterior talar process. (g) Situation after drilling a 4.5-mm drill hole into the cyst. (h) The scope is now in the posteromedial portal and the probe is placed in the posterolateral portal. The probe is located in the subtalar joint and the tip of the probe can be seen in the cyst. Following this autologous bone graft (in yellow circle) from the iliac crest is obtained and applied through the cannula to fill the cyst (i)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








