Fig. 19.1
Schematic of the relationship between subscapularis repair and the supraspinatus. (a) Massive retracted and contracted tear of the subscapularis and supraspinatus tendons. (b) Repair of the subscapularis partially reduces the supraspinatus retraction. (c) Repair of the supraspinatus can then be accomplished with minimal tension (Reproduced with permission from Burkhart SS, Lo IK, Brady PC, Denard PJ. The Cowboy’s Companion: A Trail Guide for the Arthroscopic Shoulder Surgeon. Philadelphia: Lippincott, Williams, & Wilkins, 2012)
Repair of the subscapularis tendon begins with proper recognition. Once recognized, a systematic approach can be utilized to arthroscopically repair all subscapularis tendon tears regardless of the degree of retraction or fatty degeneration. This chapter describes our current approach to arthroscopic management of retracted subscapularis tendon tears.
Surgical Technique
We repair all subscapularis tears arthroscopically and have found that these tears are essentially always repairable with meticulous mobilization. Three unique aspects of the subscapularis make it more challenging to repair than posterosuperior rotator cuff tears. First, the chronic subscapularis tear tends to retract much more than the remaining rotator cuff tendons, causing mobilization to be more difficult. Second, mobilization of the retracted subscapularis can be intimidating because it scars against the coracoid process, in close proximity to important neurovascular structures. Third, visualization, arthroscopic instrument manipulation, and knot tying in the limited subcoracoid space are more challenging compared to working in the subacromial space.
Order of Steps
Repair of the subscapularis requires working in the subcoracoid space. Since this space can become compromised rapidly by soft tissue swelling from fluid extravasation, it is critical to address the subscapularis prior to repairing the rest of the cuff. In general, when the subscapularis is torn, the order of steps is as follows:
1.
Arthroscopic recognition
2.
Biceps tenotomy and whipstitch in preparation for tenodesis
3.
Creation of window in the rotator interval
4.
If the subscapularis tendon is adhesed, skeletonization of the posterolateral coracoid, as well as a three-sided release
5.
Coracoplasty if indicated (i.e., if subcoracoid coracohumeral distance is <7 mm)
6.
Preparation of the lesser tuberosity bone bed
7.
Repair of the subscapularis tendon
8.
Completion of the biceps tenodesis
9.
Repair of the remainder of the rotator cuff
Diagnostic Arthroscopy
The patient is placed in the lateral decubitus position and the arm is placed in balanced suspension or an articulating arm holder at 20–30° of abduction and 20° of forward flexion. The subscapularis is initially inspected with a 30° arthroscope viewing through a posterior portal. During subscapularis tendon repair, we view exclusively through a posterior portal and switch between 30° and 70° arthroscopes as needed.
Retracted tears are the most obvious and are located by a torn medial biceps sling which creates a “comma sign.” [13] The medial sling, composed of the medial coracohumeral ligament and the superior glenohumeral ligament, normally inserts at the superior lesser tuberosity adjacent to the superolateral subscapularis footprint (Fig. 19.2). When the upper subscapularis tears away from its bone attachment, the medial sling also tears away from the bone and forms a distinctive comma-shaped arc of soft tissue (comma sign) at the superolateral corner of the subscapularis (Fig. 19.3). Identification of this structure therefore always leads to the superolateral subscapularis tendon, even when the tendon is severely retracted and adhesed medially. If the subscapularis tendon is not immediately visible at the front of the joint, it is probably retracted medially to the level of the glenoid margin. It can usually be located by placing the tip of a blunt instrument (e.g., a switching stickor shaver introduced through an anterosuperolateral portal) into the soft tissue adjacent to the glenoid rim at the level of the mid-glenoid notch. The mid-glenoid notch is the level at which the upper border of the subscapularis tendon usually crosses transversely. The tip of the switching stick is used to hook into the junction where the superolateral border of the subscapularis tendon joins the comma tissue at approximately a right angle.
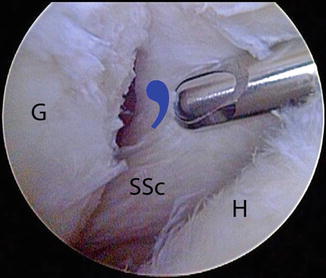
Fig. 19.2
This drawing (a) and corresponding arthroscopic photo (b) represent the view of the anterior structures from a posterior viewing portal of a right shoulder. The medial sling (M) of the biceps tendon (BT) inserts onto the lesser tuberosity of the humerus (H) along with the superolateral margin of the subscapularis (SSc). C coracoid, G glenoid (Reproduced with permission from Burkhart SS, Lo IK, Brady PC, Denard PJ. The Cowboy’s Companion: A Trail Guide for the Arthroscopic Shoulder Surgeon. Philadelphia: Lippincott, Williams, & Wilkins, 2012)
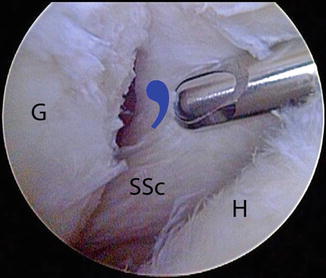
Fig. 19.3
Right shoulder, posterior viewing portal. In the setting of a retracted subscapularis tear, the medial sling tears away from the bone with the subscapularis tendon. The medial sling forms a distinctive comma-shaped arc of soft tissue (blue comma shape) at the superolateral corner of the subscapularis. As demonstrated in this photo, the comma sign serves as a landmark for locating a retracted subscapularis tendon. G glenoid, H humeral head, SSc subscapularis tendon (Reproduced with permission from Burkhart SS, Lo IK, Brady PC, Denard PJ. The Cowboy’s Companion: A Trail Guide for the Arthroscopic Shoulder Surgeon. Philadelphia: Lippincott, Williams, & Wilkins, 2012)
With a posterior viewing portal, the subscapularis footprint can only be fully visualized by using a 70° arthroscope. Visualization can also be enhanced with a posterior lever push and internal rotation of the arm. In the case of retracted tears, the lesser tuberosity will be bare.
Biceps Tenodesis
With the exception of very young individuals and throwing athletes, we routinely perform a biceps tenodesis in conjunction with repair of a subscapularis tear. Tenotomy is reserved for patients over the age of 70 or with multiple comorbidities. Poorer results have been reported when the biceps is left in place in the setting of subscapularis repair [14]. After identifying a subscapularis tear, an anterosuperolateral (ASL) portal is established viewing with a 30° arthroscope, using an 18-gauge spinal needle as a guide. This portal is typically 1–2 cm lateral to the anterolateral acromion but can vary, and placement should be such that it provides a 5°–10° angle of approach to the lesser tuberosity and is parallel to the subscapularis tendon. An 8.25 mm threaded clear cannula is placed in this portal.
Our technique for arthroscopic biceps tenodesis is briefly summarized here but has been described in detail previously [15]. Through the ASL portal, 2 half-racking #2 FiberWire (Arthrex Inc., Naples, FL) sutures are placed as traction sutures in the biceps tendon and then a tenotomy is performed. The biceps is then exteriorized, secured with a whipstitch, sized, and left outside of the ASL portal for later tenodesis. Performing the biceps tenotomy first provides greater access to the subscapularis insertion.
Accessing the Subcoracoid Space
Accessing the subcoracoid space is an essential component of subscapularis repair. A 30° arthroscope is used to initially locate the coracoid tip. Using the 30° arthroscope helps to maintain proper orientation so as to avoid inadvertent dissection as all important neurovascular structures are greater than 2.5 cm from the tip of the coracoid [16]. In non-retracted tears, the coracoid tip is usually just anterior to the upper subscapularis tendon and can be palpated with an instrument inserted through the ASL portal. A shaver or electrocautery is used to make a window in the rotator interval just superior to the subscapularis tendon and medial to the comma tissue. We strongly believe it is important to preserve the comma tissue during this step because of the connection to the supraspinatus tendon and its ability to afford margin convergence suturing to the posterior cuff.
With retracted tears, the tendon is usually initially resting medial to the coracoid, and the coracoid tip is frequently hidden behind bursal leaders that extend from the lateral border of the subscapularis to the anterior internal deltoid fascia. These bursal leaders must be released to access the subcoracoid space. Once the comma sign is identified, an electrocautery can be used to free these adhesions by working parallel and slightly anterior to the comma tissue. Usually after just a few sweeps of the electrocautery, the conjoined tendon and coracoid tip will be visualized, providing access to the subcoracoid space. A 70° arthroscope is then inserted and attention is turned to the 3-sided release. The 70° arthroscope offers a much wider field of view medially for skeletonizing the coracoid neck and coracoid base.
Three-Sided Subscapularis Tendon Release
Retracted tears of the subscapularis require a three-sided release. A traction suture is placed in the superolateral tendon medial to the comma tissue using an antegrade suture passer (FastPass Scorpion; Arthrex, Inc., Naples, FL). In order to maintain freedom in the ASL working portal, it is helpful to briefly remove the cannula and replace it so that the traction suture remains in the ASL portal but outside of the cannula. A hemostat can be placed on the traction stitch to separate it from the biceps whipstitch sutures which exit the same portal. While pulling laterally on the traction suture, the coracoid is then identified and a window is created in the rotator interval as described previously (Fig. 19.4).
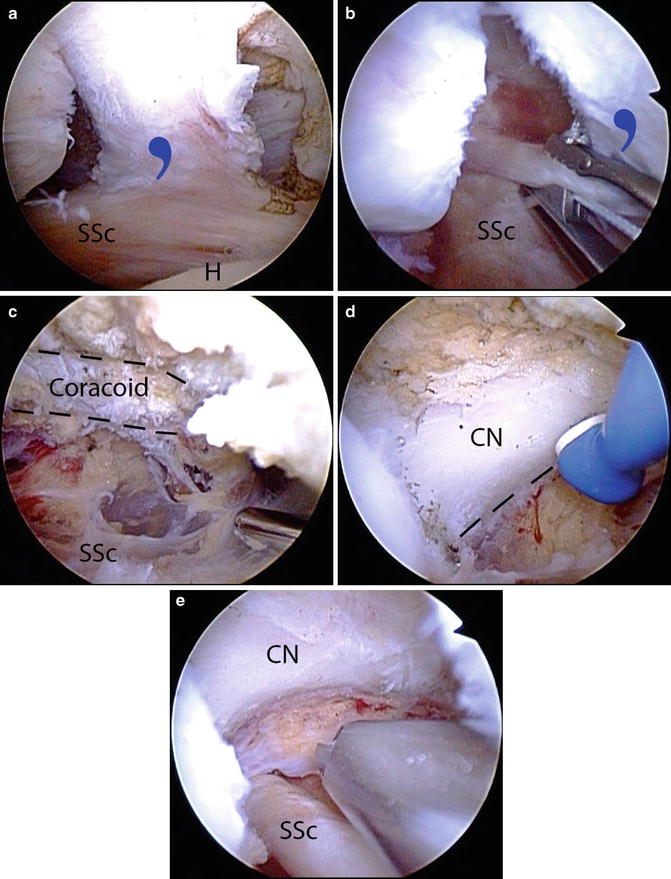
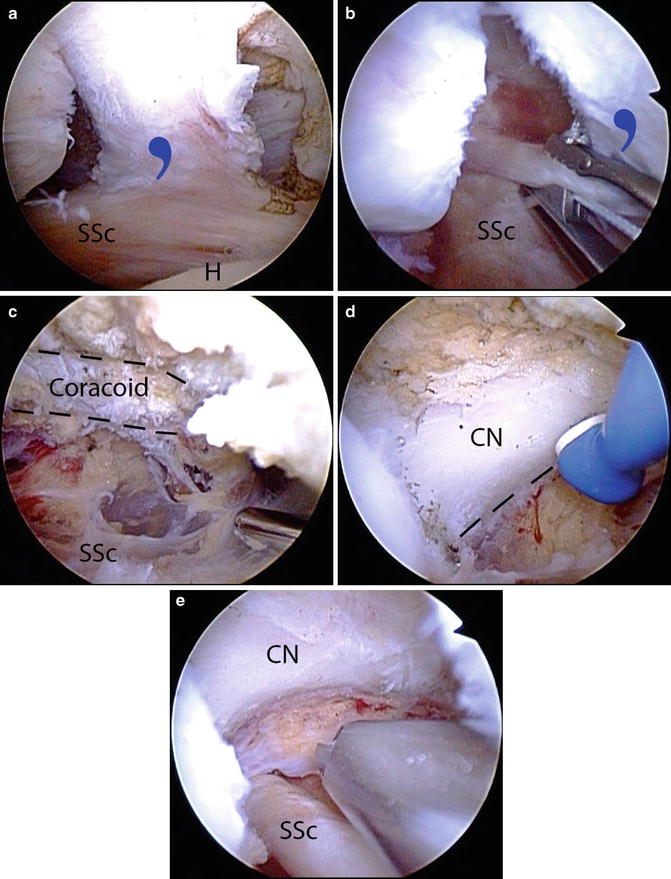
Fig. 19.4
Anterior release of a retracted adhesed subscapularis tendon tear in a right shoulder, viewed from a posterior glenohumeral portal. (a) While viewing with a 30° arthroscope the comma sign is identified. (b) A traction stitch is placed in the upper subscapularis tendon. (c) The arthroscope is placed through a window in the rotator interval to indentify the coracoid. (d) While viewing with a 70° arthroscope, the posterolateral coracoid is skeletonized to the level of the coracoid neck and coracoid base using an electrocautery. (e) After the anterior release is completed the coracoid neck and underlying subscapularis tendon are clearly visualized. CN coracoid neck, H humerus, SSc subscapularis tendon, blue comma symbol, comma sign (Reproduced with permission from Burkhart SS, Lo IK, Brady PC, Denard PJ. The Cowboy’s Companion: A Trail Guide for the Arthroscopic Shoulder Surgeon. Philadelphia: Lippincott, Williams, & Wilkins, 2012)
The posterolateral coracoid tip is skeletoniz ed with an electrocautery and a shaver is used to remove the fibrofatty bursa between coracoid and the anterior aspect of the subscapularis tendon. This step constitutes the anterior release.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








