Repair of Congenital Pseudarthrosis of the Tibia with the Williams Rod
Perry L. Schoenecker
Margaret M. Rich
DEFINITION
In most cases, the pseudarthrosis is preceded by increasing anterolateral bowing of the tibia.8
Spontaneous healing does not occur; shortening and angulation with instability are progressive and impair ambulation.
Surgical treatment with a solid intramedullary rod and bone graft and long-term protection with a total contact orthosis can provide lasting consolidation and minimize secondary deformity.1, 3, 5, 7, 9
ANATOMY
The tibia is abnormal from birth; however, this may not become apparent until weight bearing begins. The remainder of the extremity is normal.
Most patients will have anterolateral bowing that increases to the point of pathologic fracture.
Shortening is common and tends to increase after fracture.
As the anterior bowing increases, the foot may assume a dorsiflexed position to maintain contact with the floor.
Involvement of the fibula is variable and may worsen as the tibial pseudarthrosis progresses.
Nearly all cases are unilateral.
PATHOGENESIS
Anterolateral bowing, when present, increases with weight bearing as the mechanical axis falls farther behind the axis of the tibia. Additionally, the calf musculature acts like a bowstring and increases tension within the tibia, leading to failure.
Most pseudarthroses occur in the middle to distal third of the tibia.
The pseudarthrosis comprises hamartomatous fibrous tissue, not neurofibroma.
NATURAL HISTORY
Rarely, bowing or sclerosis is present and does not progress to fracture and pseudarthrosis.
Once established, the pseudarthrosis remains and does not resolve spontaneously. The resultant instability and shortening interferes with normal ambulation.
Use of a total contact orthosis may slow the progression and postpone, but, not eliminate the need for surgical intervention.
More severe deformities become symptomatic at an earlier age, occasionally presenting in infancy.
PATIENT HISTORY AND PHYSICAL FINDINGS
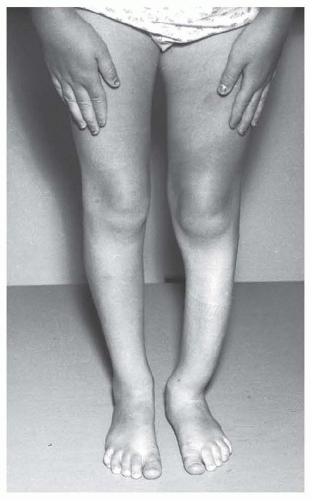
The most common presenting complaint is anterolateral bowing of the tibia (FIG 1).2, 4 Shortening of the involved extremity may not be apparent at presentation.
Pain is absent unless the tibia has fractured acutely.
Limp or dull aching may precede pathologic fracture.
The skin should be closely inspected for café-au-lait spots, axillary or inguinal freckles, or neurofibromas as signs of underlying NF.
A family history of NF may be present.
Referral to a geneticist is recommended for confirmation of the diagnosis and genetic counseling.
IMAGING AND OTHER DIAGNOSTIC STUDIES
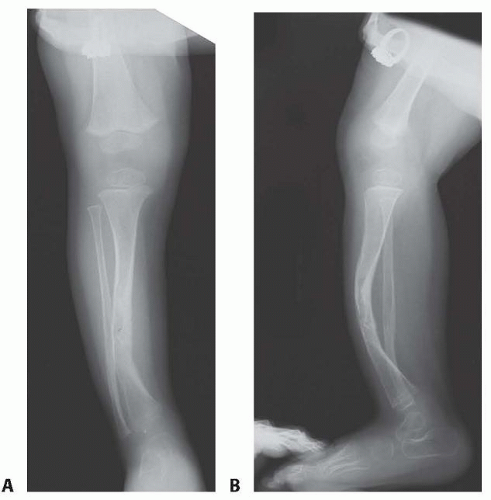
Anteroposterior (AP) and lateral plain radiographs of the affected tibia are sufficient for diagnosis (FIG 2).
The radiographic appearance of the tibia is variable: it may be cystic, sclerotic, or atrophic. There may be involvement throughout the tibia.2, 3, 4
Mild deformities present with bowing and mild sclerosis at the apex. The medullary canal can be narrow or expanded, with a cystic appearance.
After fracture, little callus forms and the bone tends to become more atrophic in appearance.
Severe deformities show resorption of bone at the pseudarthrosis, increasing fibular deformity, and tapering of the bone ends (the “pulled taffy” appearance).
DIFFERENTIAL DIAGNOSIS
Ring constriction or amniotic band syndrome
Fibrous dysplasia
Osteofibrous dysplasia
Osteomyelitis
Fibrosarcoma of infancy
Fibular hemimelia (total absence of the fibula)
NONOPERATIVE MANAGEMENT
Use of a total contact ankle-foot orthosis (AFO) or knee-ankle-foot orthosis (KAFO) provides mechanical support for the tibia, particularly in toddlers and young children.8
Pathologic fracture in a very young child can be treated with cast immobilization if the bowing deformity is mild.
Nonoperative measures are useful to postpone the age for surgical treatment, allowing the use of a larger intramedullary rod and greater volume of available autologous bone graft.
SURGICAL MANAGEMENT
The presence of a pseudarthrosis warrants operative treatment to stabilize the tibia and provide a sufficient biologic framework for healing.1, 3, 5, 6, 7, 8, 9
The intramedullary rod is designed to provide long-term stabilization of the tibial pseudarthrosis as the child grows. The rod remains in place, anchored by press-fit in the medullary canal. The proximal tibia and the distal tibia grow away from the ends of the rod.10
Younger children may require exchange with a longer rod if needed to maintain support of the tibia and stabilization of the pseudarthrosis.
Preoperative Planning
The dimensions of an appropriate-sized rod can be determined from the plain films. The width of the medullary canal adjacent to the pseudarthrosis dictates the diameter of rod to be used. The length of the rod is determined from the lateral film.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree