Fig. 8.1
Smaller but medial Hill-Sachs lesion which will “engage”

Fig. 8.2
Large, engaging, Hill-Sachs lesion
While viewing from above, the shaver is inserted posteriorly. In preparation for the remplissage, the Hill-Sachs defect is gently debrided down to its bleeding base.
After preparation of the Hill-Sachs, a cannula is placed through the posterior portal. Using this cannula, a double-loaded anchor is inserted just lateral to the myotendinous junction of the infraspinatus, and it is inserted into the Hill-Sachs defect, making sure that the trajectory remains perpendicular to the bone. If the initial portal is deemed too medial, an additional, more distal, and lateral portal is created. After anchor placement, all four suture limbs are withdrawn outside of the body, and the cannula is pulled from the joint and into the sub-deltoid space, just external to the infraspinatus muscle. A penetrating grasper is then inserted into the cannula and across the infraspinatus tendon, superior to the site of the tendon where the anchor was passed. One suture limb from the first pair is grabbed and retrieved. This step is performed again, this time with another suture limb from the other suture pair. This time, the penetrating grasper is inserted inferiorly, in order to effect a stronger tenodesis. In the presence of good tissue, only two suture limbs will suffice. Once all four sutures are outside the body, the inferior pair is tied first within the sub-deltoid space. The superior suture limb pair is subsequently tied. The infraspinatus is thus tenodesed within the Hill-Sachs lesion, and the remplissage is complete (Fig. 8.3). If an additional anchor is necessary, it is important to proceed with the distal most aspect of the lesion first. The senior author prefers to complete the tenodesis first in the distal anchor before proceeding to the more proximal region. Often an additional more proximal portal is necessary for the second anchor. The capsulolabral repair can then be performed, and a sharp obturator is used to reestablish a new posterior portal which will be used for suture shuttling during the Bankart repair.


Fig. 8.3
Post-remplissage: arthroscopic view of infraspinatus tenodesis into Hill-Sachs lesion
Results
Overall, arthroscopic remplissage has proven to be safe in the treatment of recurrent anterior glenohumeral instability. Compared to other methods of addressing humeral head defects, remplissage provides several distinct advantages. The procedure can be performed entirely arthroscopically, thus avoiding the morbidity and the prolonged recovery often encountered with open procedures. Likewise, it is a procedure that can be performed in conjunction with other arthroscopic procedures, such as Bankart repair , without adding substantial operative time [17]. The infraspinatus does appear to integrate well into the defect as Park [19] has shown at least 75 % fill of the lesion on post-op magnetic resonance imaging (Fig. 8.4). Likewise, the presence of fibrocartilaginous-like signal on postoperative magnetic resonance imaging scans suggests the potential for the infraspinatus tissue to have more bony properties in time [19] (Fig. 8.5).
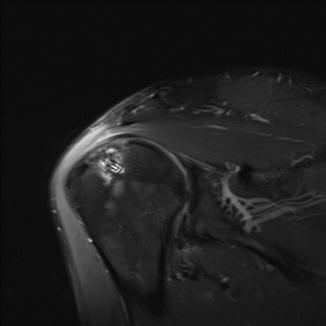
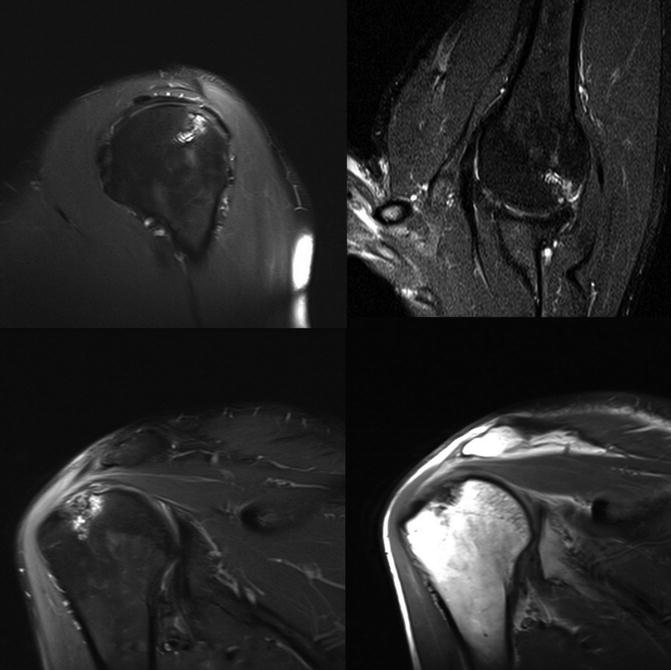
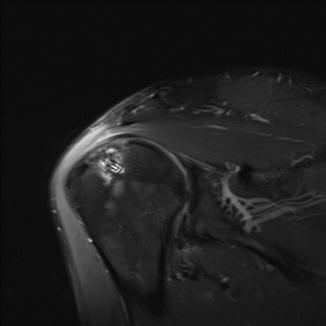
Fig. 8.4
Postoperative magnetic resonance imaging demonstrating healing of remplissage into defect
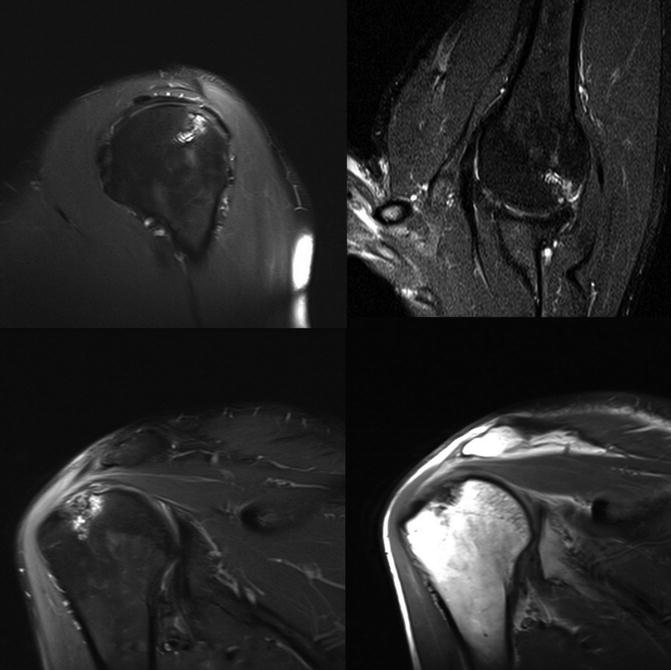
Fig. 8.5
5.5 months status post-remplissage demonstrating infraspinatus integration into bone
Several biomechanical studies have been performed to evaluate the effectiveness of remplissage. In 2012, Giles et al. evaluated cadaveric specimens with Hill-Sachs lesions on a shoulder simulator and found that remplissage was effective in preventing engagement and dislocation of humeral heads with Hill-Sachs defect sizes of both 30 % and 45 % [20]. A separate cadaveric analysis by Elkinson et al. in 2012 helped further elucidate this. In their investigations, the authors evaluated Hill-Sachs lesions sized at 15 % and 30 % and treated with a combination of Bankart repair with remplissage. They found that when treated with Bankart alone, none of the 15 % Hill-Sachs lesions engaged and dislocated, whereas all of the 30 % lesions did. However, the dislocation rate of the 30 % Hill-Sachs lesions was significantly reduced if remplissage was added in conjunction to Bankart repair—thus helping to corroborate the notion that remplissage is most effective in the setting on minimal glenoid bone loss and sizable engaging Hill-Sachs defects [21].
Clinically, several studies have been performed highlighting the effectiveness of remplissage with both good clinical and functional outcome scores [7, 14, 22, 23]. In 2001, Park et al. examined a series of 20 patients who underwent the procedure and concluded that remplissage was an effective procedure to help restore function, alleviation, and patient satisfaction [23]. Complications , such as posterosuperior shoulder pain as well as loss of shoulder motion, particularly external rotation, have been described [24, 25]. Despite this, several investigations have revealed that arthroscopic remplissage is well tolerated without postoperative shoulder pain or loss of motion [1, 14, 22, 23, 26]. In a systematic review, Buza et al. concluded that the results of remplissage compared favorably to those of Bankart repair performed in the absence of appreciable bone loss [7].
Conclusion
Several treatment options exist for the management of recurrent anterior shoulder instability. Defining the pathogenesis of this instability is an important first step in helping to guide these options. It is generally accepted that management of large glenoid defects (greater than 25 % width) typically demands bony augmentation techniques, such as coracoid transfer. However, management of the engaging Hill-Sachs lesion is likely best served with a biologic and focal solution. The premise of “tissue filling” was initially described in the 1970s. Since that time, the field of orthopedic surgery has witnessed the maturation of this method into today’s arthroscopic remplissage procedure. The indications for remplissage have become better defined, but as the pathogenesis and the pathomechanics of shoulder instability continue to become more elucidated, they will surely continue to evolve. Both safe and effective, arthroscopic remplissage continues to gain widespread acceptance as a treatment option for shoulder in the setting of humeral head defects. Is has proven effective in minimizing recurrence, has been shown to incorporate, and has not been shown to appreciably affect motion. Remplissage will undoubtedly continue to remain an important part of a surgeon’s armamentarium in the treatment of shoulder instability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








