Ulnar collateral ligament tears
Ulnar neuritis
Flexor-pronator sprain, tear or tendinopathy
Medial epicondyle apophysitis or avulsion (little league elbow)
Lateral epicondylar tendinopathy
Olecranon osteophytes
Olecranon stress fractures
Osteochondritis dissecans
Loose bodies
17.2 Physical Adaptations to Overhead Activities
Adaptations in range of motion, ligamentous laxity and muscular compensation are seen in the throwing limb compared to the contralateral upper limb. This means comparisons with the non-injured limb may not be adequate, when restoring an athlete back to their pre-injury baseline [10, 2]. Preseason/pre-injury assessments establishing baselines of range of motion, strength, kinetic chain evaluation and upper limb and scapula stability can help inform the rehabilitation team regarding the necessary function an individual needs to regain, to compete once again. Subjective functional outcome measures such as DASH, MEPI, Oxford Elbow Score and Dutch Elbow Score can also be utilised to help monitor an athlete’s progress over time [11].
A body of evidence shows the presence of medial elbow laxity, significant elbow flexion contractures and a significant decrease in wrist flexibility in the dominant arm of overhead athletes [12]. There is also an increased strength profile for the dominant arm in the glenohumeral joint internal rotators, elbow, wrist and forearm muscles and grip strength, seen in tennis players, baseball pitchers and javelin throwers [13–18].
However, it should be noted that muscle group strength ratios are sport specific. In some overhead activities such as volleyball, tennis and handball, high elbow extensor to flexor ratios are seen [18], whereas in activities such as judo, there is an almost equal ratio of elbow extensors to flexors [19]. This should be borne in mind when designing individual rehabilitation programmes.
17.3 General Rehabilitation
The aim of rehabilitation is to expose healing tissues to appropriate stress and avoid the adverse changes to tissue biomechanics and morphology seen after prolonged immobilisation. According to Wilk [10], rehabilitation following elbow injury or surgery follows a sequential, well-defined approach, where phases overlap to ensure the athlete returns to their previous functional level, as quickly and safely as possible. The approach is based on best current available evidence, adapted to each individual and their respective sport. Each phase is entered when an athlete reaches physical milestones in terms of range and strength, rather than being time dependent. Timings are also influenced by whether an athlete has been conservatively or surgically managed.
17.4 Acute Phase
The first phase is the immediate motion phase, where the goals are to reduce the deleterious effects of immobilisation, re-establish motion, decrease pain, decrease inflammation and prevent muscle atrophy [10, 20]. Movement is initiated as soon as it is safely possible, as progressive mechanical loading is more likely to restore the morphological characteristics of capsuloligamentous, osteochondral and muscular structures [21, 22]. Animal models have demonstrated that loading upregulates genetic expression for key proteins associated with tissue healing [21–23]. Clinical studies have demonstrated that immediate elbow mobilisation, even after a simple posterolateral dislocation, results in less loss of motion with no apparent increase in instability [24]. The safe arc of motion is dictated by healing constraints of soft tissues as well as the specific pathology or surgery [10].
Mobilisation exercises are performed, in a protected range, as defined by the nature of surgery or injury. Exercises must be performed frequently throughout the day and involve all planes of elbow, forearm and wrist motion. There should be a bias towards active mobilisation, as studies show muscular activation stabilises the elbow, when compared to passive mobilisation alone [25].The elbow joint is especially prone to flexion contractures; therefore, the primary goal of this phase should be to establish full pre-injury range, especially extension.
The overhead position described by Wolffe and Hotchkiss [26] is the optimal mobilisation position to achieve this goal (Fig. 17.1).This position has been demonstrated to maximise elbow stability, by minimising ulnohumeral distraction [27]. Distraction is most marked with the arm hanging dependent by the side [27], especially when wearing a cast or hinged elbow brace, so this position for exercises should be avoided. The overhead position also has the added benefit of minimising biceps EMG activity seen clinically in the painful stiff elbow [28]. It also enhances triceps activity thereby maximising elbow extension range [29]. This position is suitable for the majority of individuals with conservatively managed elbow pathology. However, in post-operative patients, it is only suitable where a triceps-sparing approach has been taken.
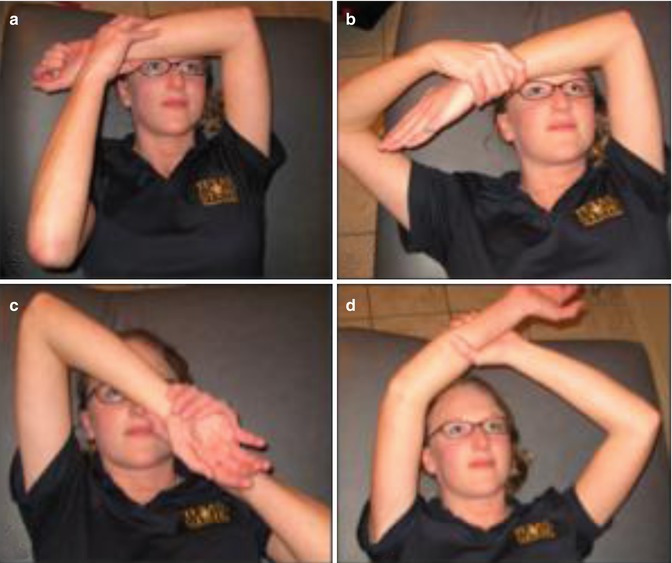
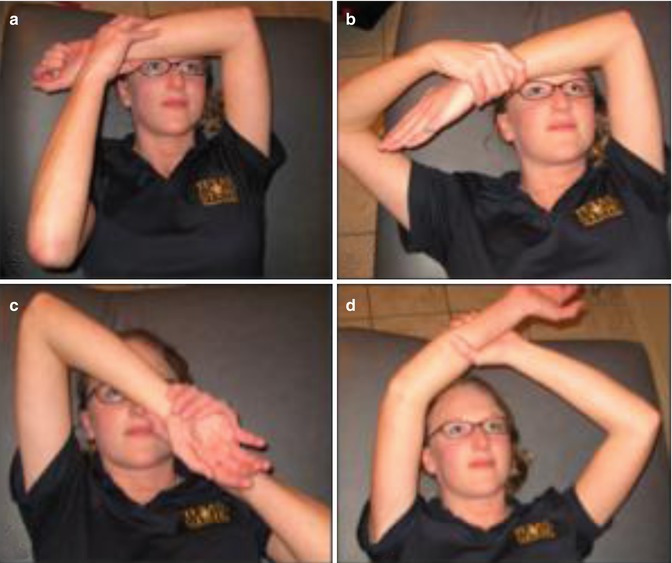
Fig. 17.1
The overhead position described by Wolffe and Hotchkiss 26 is the optimal mobilisation position to achieve this goal. This position has been demonstrated to maximize elbow stability, by minimising ulno-humeral distraction
Initially active assisted flexion/extension is performed with the contralateral upper limb providing support where needed. The forearm position during this exercise is dictated by the capsuloligamentous structures that need protecting. With lateral compartment lesions, the forearm is placed in pronation, whereby passive tension in the common extensor origin contributes to lateral stability. It follows therefore that with medial compartment lesions, exercises are performed in supination, and stability is afforded by passive tension in the common flexor origin [25]. Exercises are progressed to active movements without assistance, as soon as comfort allows. It is very important that any exercise or alternative techniques used in this stage produce minimal pain, as neuropeptides such as substance P, involved in pain transmission, can be associated with increased myofibroblastic activity [30]. This is seen in individuals with contracted elbow capsules, a common complication seen after elbow trauma or surgery. Supplemental manual therapy may also be used in the early phase, to modulate pain, by stimulating type I/II articular receptors [10]. In elbow tendinopathy, mobilisations with movements can be applied, where they have a demonstrable effect on decreasing pain on symptomatic activities [31], e.g. grip. During this phase, focus is also placed on voluntary activation of muscles and reducing muscular atrophy. Isometric exercises of the major elbow, forearm and wrist muscle groups are performed, which have been shown to place no additional strain on healing ligamentous grafts [32]. Contractions are performed at the common flexor pronator group and the common extensor group, which are secondary stabilisers of the medial and lateral compartments, respectively [33]. Also the dynamic stabilisers, producing compression at the elbow, are targeted including triceps, biceps and anconeus [33]. Anconeus appears from both EMG and anatomical studies to be a lateral elbow stabiliser, co-apting the ulna to the humerus, reducing posterolateral rotatory displacement [34–36], and can be facilitated isometrically even when the elbow is immobilised in a plaster cast or splint.
Isometric contractions also have the additional benefit of reducing pain, via a generalised, centrally induced, pain inhibitory response. The magnitude of this effect increases with contractions of longer durations and of moderate or above intensity (40–50 % MVC) and is not constrained to the exercising limb [37–42]. Some therapists advocate the use of neuromuscular electrostimulation (NMES) to facilitate this process; however, more good quality evidence regarding its beneficial effects is limited. One consideration for post-operative patients is which surgical approach was used and the condition of the muscle origins, in order to guide early resistance work [43]. Therefore, good communication between the surgical and therapy team is essential. Shoulder isometric work may be performed with caution with resistance applied proximal to the elbow. However, care should be taken with positions of extreme glenohumeral external rotation, as they produce a valgus moment at the elbow, possibly compromising vulnerable tissues [43].
17.5 Intermediate Phase
This is started when the following is achieved, a return to pre-injury range, with minimal pain and tenderness and good strength of elbow and forearm musculature [10], usually at 4–6 weeks post-injury/surgery. Elbow extension and forearm pronation are of particular importance for effective performance in throwing sports [10, 20]. Local strengthening exercises are progressed to isotonic contractions, beginning with concentric work, then eccentric work, with emphasis placed on the secondary stabilisers [10] (Fig. 17.2). With medial compartment symptoms, emphasis should be placed on the flexor pronator mass, especially flexor carpi ulnaris, which anatomical and EMG studies have been shown to contribute to valgus stability, by reducing forces placed on ulnar collateral ligament, during throwing [44 – 47]. With tendinopathy, the key goal is improving the capacity of the tendon and muscle to manage load. Several strengthening options exist, as described previously, as well as heavy slow resistance work, all sharing a common goal of gradually increasing load, whilst carefully monitoring pain. This approach for tendinopathy has been supported by clinical trials, with long-term benefits seen compared with pharmacological and electrotherapy interventions [48–50].


Fig. 17.2
Local strengthening exercises are progressed to isotonic contractions, beginning with concentric work, then eccentric work, with emphasis placed on the secondary stabilisers [10]
Counterforce bracing is only useful in individuals where it demonstrably reduces pain or improves grip and is only worn during pain-provoking activities [51]. Emphasis is also placed on exercises improving endurance and neuromuscular control of the elbow complex [10, 20, 52]. Loss of kinaesthetic awareness of upper extremities can occur post-injury and has been shown to decrease proprioceptive accuracy in throwers [53–56]. Proprioceptive neuromuscular facilitation, rhythmic stabilisation drills and open and closed kinetic chain activities, which promote cocontraction and mimic functional positions with joint approximation, are now implemented [10]. Studies show a decrease in neuromuscular control, kinaesthetic detection strength and throwing accuracy is associated with muscular fatigue; therefore, exercises, including multiple sets [2], to promote endurance are a key component of this stage.
Shoulder flexibility is also addressed at this stage, as loss of total shoulder rotational range or glenohumeral internal rotation deficit (GIRD) has been shown to place strain on medial elbow structures during throwing [57, 58]. It is advised that between sides, differences should be less than 18° and the difference in total range of motion should not be more than 5°. The assessment of rotational range of motion can be measured with a goniometer or an inclinometer. Posteroinferior glenohumeral capsular tightening and shrinkage, along with adaptive humeral head changes, are well-documented problems in long-term throwers [57, 58, 59]. For this group, stretches such as a sleeper stretch are thought to be effective in addressing the posterior capsular tightness [60] and significantly increase acromiohumeral distance in overhead athletes with GIRD, after a 6-week stretching programme. Care should be taken with stretches at extremes of glenohumeral external rotation, as mentioned previously. According to Ellenbecker [9] you see the modified sleepers stretch in sidelying with a towel beneath the upper arm to provide horizontal adduction to achieve more stretch on the capsule in the 90 degrees abduction position.
It is also important not to apply this to all individuals with elbow injury or pathology. It must be considered that the GIRD may be a problem, not just due to capsular pathology [57]. For this group stretching may not be as effective, and the problem should be addressed by performing eccentric and concentric rotator cuff exercises through range. It is essential that the individual is carefully assessed to ensure that any deficit is managed appropriately. Therefore, a comprehensive assessment of the shoulder and the scapula should be undertaken, as scapula dysfunction prevents optimum energy transfer in the upper limb. Glenohumeral rotational strength and scapula strength are addressed during this phase [10, 2, 20, 43] and are incorporated in the throwers TEN strengthening programme [61]. This has been designed, from EMG evidence, to illicit muscular activity most needed to provide upper limb dynamic stability [62, 63] and has been demonstrated to increase throwing velocity, following a 6-week programme [64]. Attention should be paid to global upper limb strengthening, even with elbow tendinopathy, as previous studies have shown global weakness, affecting all major shoulder groups, and the triceps, with this condition [65], probably due to pain inhibition and disuse. The use of flywheel and fly pull devices has been advocated in restoring muscle strength and neuromuscular coordination and endurance. In these athletes eccentric training with maximum of coordination and kinetic chain position is provided in tennis (adolescent and ATP level) and Gymnastics (Olympic level) to restore muscle strength and coordination or maintain during the season their high level of sports in training the kinetic chain by squats or IR/ER in 90 degrees of abduction.










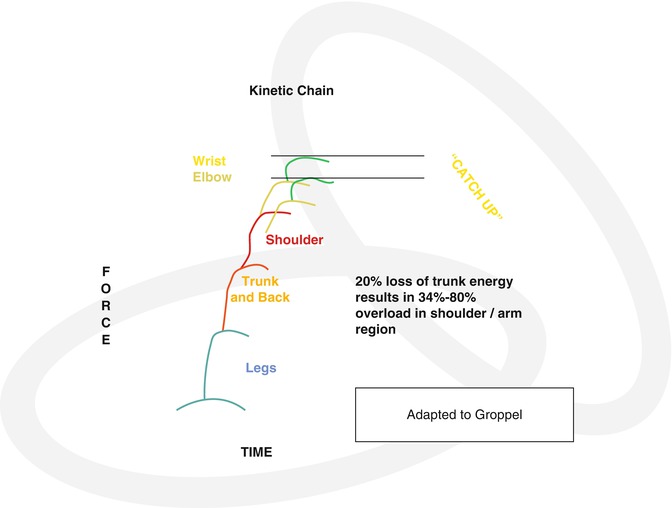
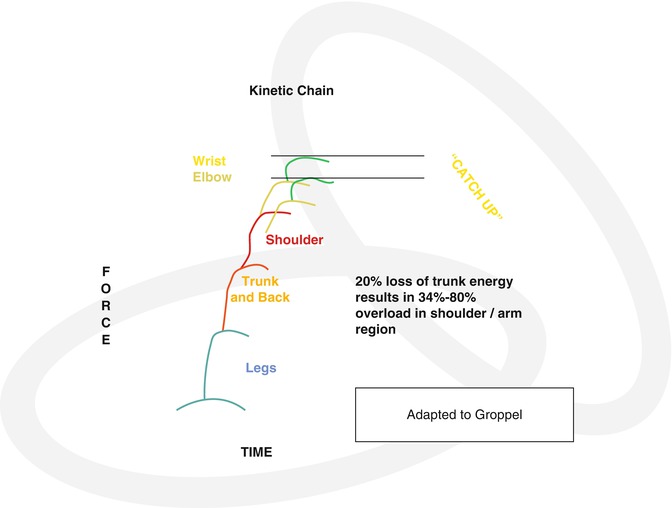
It is vital to concentrate not only on the upper limb but also on the whole kinetic chain at this stage in rehabilitation, the kinetic chain being a specific sequence of movement which allows efficient accomplishment of a task. Injuries or adaptations in remote areas of the chain can cause problems not only locally but also distally, as joints such as the elbow compensate for lack of force production and energy delivery through more proximal links [10, 66]. Kibler and Chandler [67] calculated a 20 % reduction in kinetic energy delivered from the hip and trunk to the upper limb and require a 34 % increase in rotational velocity of the arm, to impart the same amount of force to the hand. Hannan et al.’s study [68] has shown a link between lower limb balance deficits in throwers with medial elbow ligament injuries compared with healthy controls. These balance deficits disappear following a 3-month throwers rehab programme including the trunk and the lower limb. Therefore, in this early stage, whilst the elbow is recovering, leg and trunk exercises involving sport-specific activation patterns can be initiated, so that the base of the kinetic chain is ready for the next phase, late-stage rehabilitation.
17.6 Late-Phase Rehabilitation
This stage involves progression of activities to prepare the athlete for a return to sport. The goal of this stage is to gradually increase strength, power, endurance and neuromuscular control. Physical criteria to progress to this phase include full active range of movement, no pain or tenderness, strength that is 70 % of that of the contralateral limb and a functional score that indicates less than 15 % impairment on QuickDASH or similar subjective outcome score [10]. Usually, progression to late-stage rehabilitation will commence between 7 and 12 week and depends upon whether an athlete has been conservatively or surgically managed. Strengthening exercises emphasising higher resistance and functional sports-specific movements, including eccentric and plyometric activities, are now employed. Elbow flexion exercises are progressed to emphasise eccentric control, as biceps is an important stabiliser, during the follow-through stage of throwing. Eccentric control prevents pathological abuttal of the olecranon in the olecranon fossa. Concentric triceps activity is also emphasised during this phase, because of the triceps activity seen during the acceleration phase of throwing.
Resistance exercises should be chosen that closely stimulate the demands of an athlete’s individual sport. In ground-based sports, exercises that simulate throwing or service action in tennis, with the glenohumeral joint in 90° of abduction in the scapula plane, are advocated. Regimes such as the Advanced Throwers Ten Programme incorporate exercise and movement patterns specific to the throwing motion. The programme utilises the principle of co-activation, high level neuromuscular control, dynamic stability, endurance and coordination that are vital in the overhead athlete. However, in swimmers, Swiss ball exercises, performed in the prone position with the feet off the floor, may appear to be more specific to the demands of this particular sport. Exercises to promote endurance should be emphasised during this phase, because the overhead athlete is at risk of injury, if throwing whilst fatigued. Endurance drills using lower weights and higher repetitions are advocated, which have been shown to preferentially load key muscle groups required in overhead sport. Fatigue also adversely affects proprioception; therefore, endurance activities are critical in improving coordination and joint stability. This stage should also commence plyometric exercise and controlled impact work. Plyometric drills can be a beneficial form of functional exercise for training the elbow and have been shown to increase throwing and service action speeds, increase elbow extension power and improve measures of proprioception and kinaesthesia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








