INTRODUCTION
Communication is the process by which people exchange information. Language is the process by which thoughts, feelings, and emotions are generated using a recognizable verbal or written system. It includes both receptive and expressive skills. Speech is the process of creating sounds and combining them to form words that are understood by a listener. It requires the integration of cognitive and neurologic abilities along with the musculoskeletal skills that support respiration, phonation, and articulation. Cognition refers to mental processes, including attention, memory, auditory processing, problem solving, and executive function. Some of the cognitive skills that are important for communication include processing speed, concentration, self-monitoring, thought organization, and memory. Verbal communication, the most common form, involves the use of speech, language, and cognitive skills, augmented by facial expressions and gestures.
Speech, language, cognitive, voice, and swallowing problems are key issues for patient management in acute rehabilitation settings. Speech–language pathologists (SLPs) assess and treat impairments in each of these domains. During the initial stages of a patient’s diagnostic workup, a speech and swallow evaluation is warranted, especially if caregivers and family members report changes in communication, cognitive, or swallowing ability. During the rehabilitation process, the SLP, along with other members of the multidisciplinary team, provides quality care to help the patient reach his or her fullest physical, psychological, social, vocational, and educational potential.
The main areas to be tested in patients undergoing evaluation include speech, language, voice, cognition, and swallowing. All parameters are assessed or at least screened using formal tests or informal measures. The primary objective is to determine the presence of impairment, classify the type, and determine the level of severity. Based on the results, recommendations and functional prognoses are made, a treatment plan is formulated, and measurable therapy goals are developed. The information from the initial assessment provides an important baseline for measuring change.
The goal of speech, language, and cognitive-based therapy is to improve communicative effectiveness, efficiency, and naturalness. Three main therapeutic approaches, outlined by Duffy, can be used to achieve these goals. The first is to restore lost function. This effort aims to reduce impairment and targets deficits directly. Achieving success with this approach depends on the etiology and course of the disease, as well as the type and severity of the disorder. The second approach is to promote compensatory abilities and the use of residual function. Compensation can take many forms; for example, a patient might be instructed in speech-enhancing strategies or the use of augmentative devices or alternative means of communication (gestures, functional communication board, etc). A third approach encompasses strategies to reduce a patient’s need for lost function by modifying the environment and facilitating more effective speaker–listener interactions. Through education and counseling, SLPs also help patients and their families adjust and cope.
The primary objective for swallow rehabilitation is to achieve the least restrictive dietary level while maintaining swallowing safety. Swallowing safety can be described as the maintenance of nutrition and hydration without medical complications. Specifically, SLPs aim to have a patient tolerate the least restrictive diet without aspiration. Dietary modifications focusing on liquid consistencies or food textures may be made. Dysphagia therapy entails teaching a patient compensatory swallowing strategies and targeting deficits directly through various exercises to change swallowing performance. Patient and family education is important to ensure compliance with diet modifications, aspiration precautions, and carryover of swallowing exercises and strategies.
When determining a treatment plan, all clinicians should consider patient, family, and caregiver needs and desires while simultaneously considering the patient’s level of impairment and functional abilities. Treatment can focus on functional goals, which may be tailored to a patient’s specific needs (eg, a personalized functional communication board for a patient with expressive aphasia) or traditional goals, which target specific deficits (eg, word recall for the patient with expressive aphasia). Therapy can be direct (eg, drills, structured tasks) or indirect (eg, informal therapy tasks such as board games). In all cases, treatment within the inpatient rehabilitation setting should aim to make the patient as independent as possible. Therapeutic change achieved in the medical setting that is effectively carried over to the patient’s daily life is considered to be a successful treatment outcome.
The human nervous system, comprising the central nervous system (the brain and spinal cord) and the peripheral nervous system (the sensory and motor nerves), is integral to our ability to formulate and express language. The brain initiates, controls, and regulates sensorimotor and cognitive functions through the functions of its various parts: the cerebral cortex, cerebellum, brainstem, and subcortical structures. Language and speech disturbances can be indicators of structural and physiologic impairment in the brain. A review of basic brain physiology is therefore essential to understanding the language disorders that derive from disease and injury affecting these structures. With knowledge of the area of neurologic insult, the SLP can predict what type of impairment to expect upon initial evaluation. An understanding of the neurologic bases of communication also contributes to a more effectively structured and realistic rehabilitation program.
The cerebral cortex is divided into two hemispheres, each comprising four lobes that regulate complex functions (Table 38–1). The cerebellum, located inferior to the occipital lobes and posterior to the brainstem, is crucial for maintaining balance in space and executing coordinated movements. A critical function of the cerebellum for speech and swallow is the integration of sensory input from other regions of the brain, allowing it to coordinate muscle groups. Through modifications of muscle tone, speed, and range of motion, the cerebellum allows movements to be executed smoothly and helps to make sequenced motor skills automatic. It does not initiate motor activity, but instead controls and performs online correction of planned movement.
| Lobe | Location | Function | Impairment |
|---|---|---|---|
| Frontal | Most anterior part of the brain | Language production Planning and initiation Judgment and reasoning Concentration Emotional range Inhibition Adaption to change Insight | Poor pragmatics Loss of flexible thinking Perseverations Poor focus or attention Emotional lability Inability to express language (Broca’s aphasia) Difficulty in problem solving |
| Temporal | Laterally in cerebral hemispheres | Auditory sensation and perception Auditory comprehension Memory acquisition Visual perception Categorization of objects | Difficulty comprehending language (Wernicke’s aphasia) Prosopagnosia Disturbance with selective attention to what is seen and heard Memory loss |
| Parietal | Between occipital lobe and central sulcus | Sensory integration—touch, pressure, pain, temperature, taste | Poor divided attention Anomia Alexia Agraphia Dyscalculia Poor kinesthetic awareness Unilateral neglect |
| Occipital | Most posterior part of the brain | Visual processing Visual discrimination Visual association | Visual field cuts Difficulty locating objects in environment Difficulty reading or writing |
The brainstem, which consists of the medulla oblongata, the pons, and the midbrain, connects the brain to the spinal cord and regulates primary life functions such as respiration, swallowing, blood pressure, eye movements, and heart rate. It also mediates functions such as coughing, gagging, hearing, balance, and body temperature. The medulla oblongata is important for speech and motor control, as it contains nerve fibers that control phonation, articulation, velopharyngeal closure, and swallowing. It is also crucial for overall arousal, and important for sleep. The pons bridges the brainstem to the cerebellum, helps control breathing and sleep, and is also important for alertness and arousal. The midbrain contains structures important for vision and hearing. The subcortical structures (thalamus, hypothalamus, hippocampus, amygdala, and basal ganglia) are located above the midbrain (Table 38–2); each of these structures plays a role in supporting speech, language, and swallowing.
| Structure | Location | Function | Impairment |
|---|---|---|---|
| Thalamus | Center of forebrain | Relay of sensorimotor input to other areas of the brain Contributes to cortically mediated speech and language functions | Lower pain threshold Impaired contralateral somatic sensation |
| Hypothalamus | Ventral to thalamus | Regulation of endocrine functions Hormonal system regulation Temperature regulation Blood volume Food and water intake Reproduction Circadian rhythm Wakefulness, activity level, metabolism Emotional expression | Difficulty with feeding and drinking Impaired control of body temperature regulation Impaired sleep–wake cycles Altered salt metabolism Difficulty expressing emotions Poor drive and initiation |
| Hippocampus | Between thalamus and cerebral cortex | Important for recent working memory Inhibition of a habitually unsuccessful action Spatial navigation | Inability to form new memories (anterograde amnesia) Failure to remember spatial layouts or landmarks Topographic disorientation |
| Amygdala | Located deep within medial temporal lobes of the brain | Involved in forming and storing memories associated with emotional events Regulation of emotions and motivation | Reduced safety awareness Poor recognition of risks Inability to attribute values to actions |
| Basal ganglia | Includes caudate nucleus, putamen, and globus pallidus | Motor control and integration Regulation of muscle tone Regulation of drives, action execution, and cognitive function | Akinesia, akathisia Tardive dyskinesia Tremors, chorea, and ticks Disinhibition |
In the peripheral nervous system, sensory (afferent) and motor (efferent) nerves are connected to the spinal cord (spinal nerves) and to the brainstem (cranial nerves). The spinal nerves extend to the organs, muscles, joints, blood vessels, and skin surface. The cranial nerves originate from the brainstem and innervate the muscles of the head, neck, face, larynx, tongue, pharynx, and glands. The cranial nerves are essential for speech, resonance, and phonation. In addition, these nerves transmit signals that serve the special senses: vision, audition, smell, and taste. Their motor and sensory functions are summarized in Table 38–3.
| Cranial Nerve | Major Motor Function | Major Sensory Function |
|---|---|---|
| CN I: Olfactory | Smell | |
| CN II: Optic | Vision | |
| CN III: Occulomotor | Eye movement Pupil constriction | |
| CN IV: Trochlear | Eye movement | |
| CN V: Trigeminal | Mastication | Sensation—face, oral structures |
| CN VI: Abducens | Eye movement | |
| CN VII: Facial | Facial expressions Secretions of saliva and tears | Taste (anterior two thirds of tongue) |
| CN VIII: Vestibulocochlear | Equilibrium Hearing | |
| CN IX: Glossopharyngeal | Swallowing | Taste (posterior one thirds of tongue) Visceral sensation from oral pharynx |
| CN X: Vagus | Phonation Swallowing | Sensation—thoracic and abdominal organs |
| CN XI: Accessory | Head movement Shoulder elevation | |
| CN XII: Hypoglossal | Tongue movement |
The two major systems of the peripheral nervous system are the autonomic nervous system and the somatic nervous system. The somatic nerve fibers mediate the skeletal muscle reflexes. Through its sympathetic and parasympathetic divisions, the autonomic nervous system regulates the activity of organs, such as the salivary glands, heart, lung, blood vessels, stomach, intestines, kidneys, and bladder. Regulation and monitoring of these functions are essential to survival.
The brain’s functions are regulated by a set of general organizational principles. An understanding of these principles allows further appreciation of how impaired neurologic function can impede communication and swallowing (Table 38–4).
| Principle | Organization | Implications |
|---|---|---|
| Interconnectivity of the brain | All functions (sensory and motor) in the cerebral cortex are connected through association and commissural fibers, which allow for constant interaction within each hemisphere and between the two hemispheres. | Helps to explain how messages from multiple sources are rapidly integrated for an appropriate response to given stimuli. |
| Centrality of the central nervous system (CNS) | The CNS integrates all incoming and outgoing information in order to generate appropriate responses to the information received. The response can be volitive or reflexive. | Allows for the ability to analyze and synthesize multiple sources of information and to generate distinct responses. |
| Laterality of brain organization | Bilateral anatomic symmetry | The two cerebral hemispheres are essentially similar in structure. |
| Unilateral functional differences—each hemisphere acquires an advantage over the other for different specialized functions | Left hemisphere has language dominance. Right hemisphere dominates emotions, musical skills, metaphors, humor, and stress. | |
| Contralateral sensorimotor control—all sensory and motor fibers decussate at the body’s midline | Left motor cortex controls movements in the right half of the body. Sensory information from the left half of the body projects to the right sensory cortex, and vice versa. | |
| Functionally specialized networking | Neuronal systems are functionally specialized; sensory and motor systems consist of various pathways that transmit differentiated information to different limbs. | A specialized pathway controls speech muscles in the face and neck through cranial nerves in the brainstem. |
| Topographic organization in cortical pathways | The spatial organization of neurons, tracts, and terminals reflects the spatial relationships of the body’s surface and functionally related muscle groups | Topographic maps of functions helps physicians precisely locate lesions in the CNS. |
| Brain plasticity | The brain is able to recognize and modify tissue functions and adapt to internal and external changes. This permits regeneration of nerves and reorganization of cellular functions. | Can permit new learning and adaptability following a neurologic insult. |
Familiarity with lesion localization and causes of neurologic impairment is required to conduct a thorough evaluation of speech and language abilities and interpret the results. Speech and language disorders commonly result from cerebrovascular accidents (stroke), brain tumors, or traumatic brain injuries.
Initial examination can identify spared versus disrupted functions. Any abnormal sign in a patient presumably reflects a breakdown in neural circuitry and a specific pathway. Lesion localization can assist in providing differential diagnoses and can also provide a rationale for specific probing during an evaluation. For example, a patient with a left cortical lesion and right hemiplegia warrants testing for aphasia or cognitive communication disorders.
Initial assessment of receptive and expressive language abilities and differential diagnoses occurs in the acute care setting. Upon admittance to the acute rehabilitative setting, the patient is reevaluated to determine a level of functional communication, provide a prognosis, establish a baseline for measuring progress, and create and implement a treatment plan. Ongoing assessment of recovery and efficacy of treatment is provided throughout the rehabilitation process.
Formal diagnostic testing as well as informal observational findings are used to evaluate speech and language. Receptive and expressive communication skills are probed when assessing for aphasia, an impairment in language ability that may result from a head injury or stroke. Several areas of communication are evaluated (Table 38–5).
| Language Area | Description |
|---|---|
| Auditory comprehension | The ability to listen to and process information presented verbally. Includes the understanding of interrogatives (yes–no, “wh-”), literal and figurative language, words, phrases, sentences, paragraphs, stories, and conversation. Also includes the ability to follow commands that increase in both length and complexity. |
| Verbal repetition | The ability to repeat what one hears. |
| Automatic speech | The verbalization of commonly used sequences of language and rote phrases that occur without much conscious effort of the individual (eg, the days of the week or counting to 10). |
| Word recall | The ability to name objects and pictures during structured confrontation naming, as well as at the conversational level. |
| Fluency | The ability to produce an uninterrupted phrase-length utterance, typically more than 4 words in length. Involves the smoothness or flow with which the sounds, syllables, words, and phrases are joined together. |
| Discourse ability | The ability to converse, discuss topics, retell a story or a joke, comment, ask and answer questions, etc. |
| Grammatical use | The ability to organize words and sentences into a logical structure based on the rules of syntax for that particular language. |
| Written expression | Includes copying, writing to dictation, self-generated writing, written spelling, and drawing. |
| Reading comprehension | Includes word- and sentence-level comprehension, oral reading, and oral spelling. |
| Pragmatics (social communication) | Includes initiating conversation, taking turns during a discussion, using appropriate language in social situations, etc. |
| Nonverbal communication | Gestures, facial expressions, pointing, eye contact, etc. |
Cognitive impairment and language impairment are unique entities that influence one another. Although the person with aphasia has a primary disorder in the area of language, cognitive functions must also be evaluated as the ability to compensate for language deficits reflects cognitive functioning. Evaluation and treatment of cognitive deficits is discussed later in the chapter.
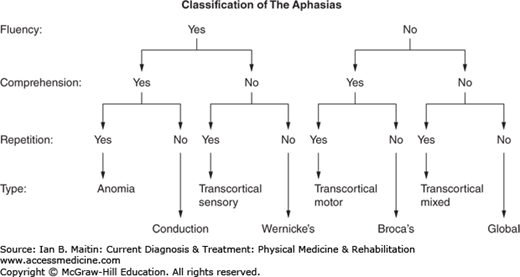
Features that confirm the presence of aphasia include difficulty with language formulation and comprehension. Virtually all patients with aphasia have some degree of anomia (ie, difficulty recalling names or words), and varying abilities in comprehension, repetition, conversation, reading, and writing. Specific types of aphasia can be determined through examination of a patient’s language presentation and lesion localization. Figure 38–1 provides a visual representation of a screening tool to classify the major aphasias.
Aphasic speech often contains recognizable errors that can assist in differential diagnosis. Agrammatism occurs in individuals with nonfluent aphasia and is characterized by the absence of functor words (ie, words that perform a function), thereby creating sentences that include primarily nouns and verbs. The speech is telegraphic and there are omissions of grammatical morphemes (small units of grammar). Paragrammatism occurs in fluent aphasias and is characterized by inaccurate application of syntactic rules. Paraphasias are errors in word recall. Phonemic paraphasias are characterized by a single phoneme substitution or similar word substitution and reflect a disruption at the phonologic level (eg, saying “ocoput” for “octopus”). Semantic paraphasias reflect a disruption at the lexical level; errors may be related to the target word (eg, saying “jellyfish” for “octopus”) or unrelated (saying “chicken” for “octopus”). A neologism is not a real word (eg, saying “ertup133” for “octopus”). Perseveration is the inappropriate repetition of a previous response that continues after the task requirements have changed and the response is no longer needed. A patient can perseverate on single words, concepts and ideas, or specific behaviors. Individuals may or may not be aware of their errors.
Each of the aphasic syndromes has both shared and unique characteristics; however, in reality, very few of them are pure, and people with aphasia have overlapping features. The subtypes of aphasia and their clinical characteristics are outlined in Table 38–6.
| Type | Lesion Localization | Major Clinical Characteristics |
|---|---|---|
| Broca’s | Lateral frontal, suprasylvian area | Nonfluent, halted, effortful speech Agrammatism Imprecise articulation Phonemic paraphasias |
| Wernicke’s | Posterior third of superior temporal gyrus | Fluent, jargon speech with normal prosody Press-of-speech (speaking rapidly without pausing, interrupting others) Poor auditory comprehension and repetition |
| Conduction | Supramarginal gyrus, left insula, auditory cortex | Fluent output with average phrase length Word-finding pauses, phonemic paraphasias Poor repetition |
| Anomic | Angular gyrus, second temporal gyrus | Word-finding problems Verbal output—use of circumlocutions and nonspecific terms |
| Transcortical motor | Anterior frontal paramedian, anterior–superior to Broca’s area | Impaired initiation of verbal output Short phrase length |
| Transcortical sensory | Posterior parietotemporal area, sparing Wernicke’s area | Significant anomia and poor auditory comprehension but good repetition skills Semantic paraphasias in verbal output and empty quality to discourse |
| Global | Large perisylvian area | Profound anomia with virtually no speech output Very poor auditory comprehension Stereotypic utterances |
| Subcortical | Internal capsule (white matter pathways), basal ganglia, thalamus | Thalamic aphasia—impaired auditory comprehension and confrontation naming Nonthalamic aphasia—impaired speech fluency, grammatical and phonologic errors Repetition is preserved |
Aphasia rehabilitation is better understood as the process of achieving a closer connection between an individual’s language deficit and his or her ability to communicate functional needs and desires. The SLP must consider both what the patient and caregivers want to do, and what the patient can do in terms of communication ability. Many factors affect communicative needs and wants, such as living environment, independence level, social interactions, and employment. The goals of treatment in therapy should always meet the following criteria, as outlined by Klein and Mancinelli:
Promote function.
Promote an effective communicative environment.
Provide compensatory strategies to communicate.
Provide education and counseling for adjustment of patient and family.
Reduce interfering behaviors.
Provide a relevant home program for patient and family.
Direct therapy for aphasia often involves targeting the deficit directly. For example, the tasks relating to lexical retrieval and sentence production therapy aim to improve functional communication by facilitating word retrieval and then producing the most grammatically correct utterance possible. Therapy exercises may include object identification, convergent and divergent naming, picture description, or conversational exchanges. Cueing hierarchies are used to elicit a response from the patient with the least amount of help from the clinician. As therapy continues, cues become less necessary. The patient is ultimately trained to use self-cuing and internal strategies for expressive language.
Among the evidence-based treatment programs available to clinicians are melodic intonation therapy and compensatory communication strategies, such as visual action therapy.
Melodic intonation therapy is a popular approach that involves musical and rhythmic intonations of phrases and sentences as the tool of language rehabilitation. The rationale for using melodic intonation is that the right hemisphere mediates musical stimuli and intonation. It is speculated that an intact right hemisphere may have the ability to improve the language functions of the left hemisphere when that hemisphere has sustained damage. The goal of this therapy is to stimulate the recovery of speech skills in severely nonfluent aphasic patients by using phrases that are intoned and paced syllable by syllable based on a melodic pattern, rhythm, and points of stress. The patient repeats melodic utterances of increasing length amid fading cues from the clinician. For example, the clinician may begin by saying the word “Hello” in a particular melody while simultaneously separating the syllables (“Hel-lo”). The clinician then encourages the patient to join him or her in producing the target word together with the same melody. Once the patient achieves this step in the process with the maximum number of cues, the clinician begins to fade cues, for instance by producing the first sound of the target word and humming the rest, then humming only the tune of the target word, and eventually guiding the patient to independently produce the target word or phrase.
Patients with severe aphasia may require compensatory communication strategies that can provide alternative ways to communicate wants and needs. An example of such a strategy is the functional communication board, which allows patients with poor verbal output to identify pictures, symbols, or written stimuli as a means of communicating more effectively with others. Patients can be taught to use an alternative communication device, such as speech-generating computer programs that build graphic symbols and pictures into phrases and sentences that are spoken aloud by a computer-generated voice. Gestures can also be taught, through visual action therapy, as a nonspeech method for the purpose of functional communication.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree