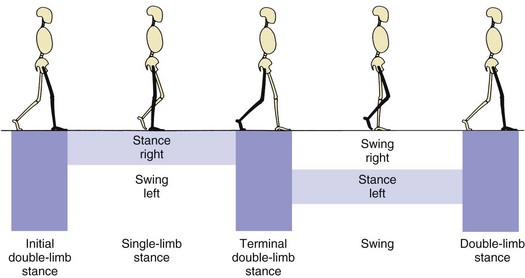
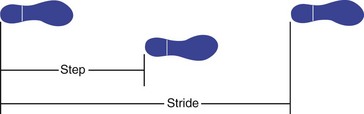
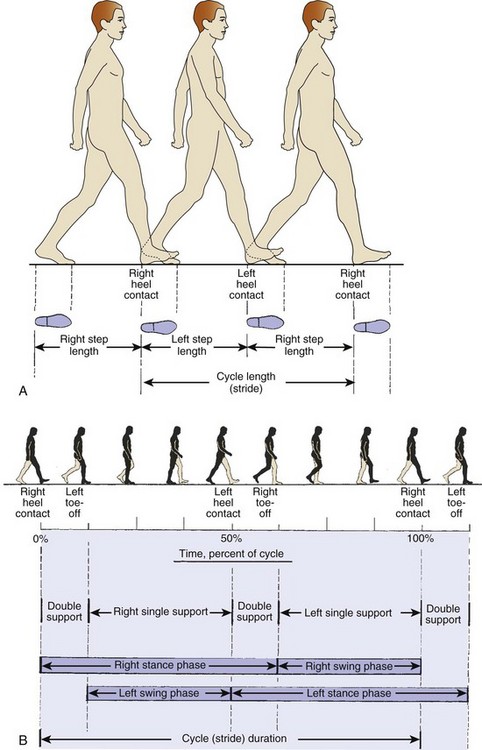
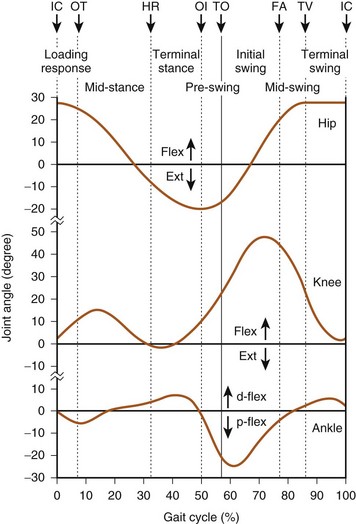
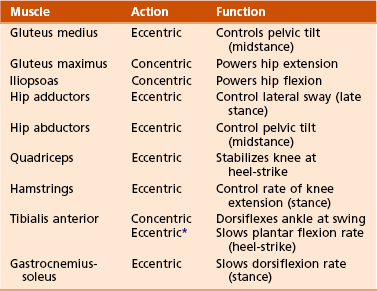
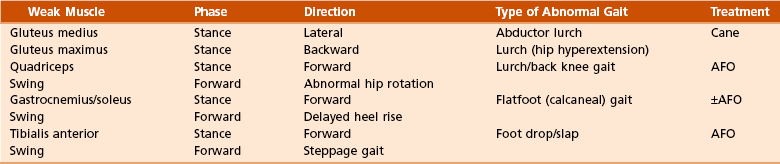
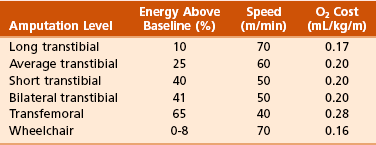
Chapter 10 1. Walking is the repetitive process of sequential lower limb motion to move the body from one location to another while maintaining upright stability. 2. Walking is a cyclic, energy-efficient activity: one foot must be in contact with the ground at all times (single-limb support), with a period when both limbs are in contact with the ground (double-limb support) (Figure 10-1). 3. The step is the distance between initial swing and initial contact of the same limb. 4. Stride is the period from initial contact to initial contact of the same limb (i.e., each stride comprises two steps) (Figure 10-2). 5. Velocity is a function of cadence (steps per unit of time) and stride length. 6. Running involves a period when neither limb is in contact with the ground. B Phases: Prerequisites for normal gait include stance-phase stability, swing-phase ground clearance, the correct position of the foot before initial contact, and energy-efficient step length and speed. 1. The stance phase occupies 60% of the cycle. 2. The swing phase is 40% of the cycle. 3. Important characteristics of gait cycle: A The combined phases of gait contribute to an energy-efficient process by lessening excursion of the center of body mass. B The head, neck, trunk, and arms account for 70% of body weight. C The trunk center of gravity of body mass is located just anterior to T10, which is 33 cm above the hip joints in an individual of average height (184 cm). D The body’s line of gravity is anterior to S2 and provides a reference for the moment arm to the center of the joint under consideration. The resulting gait pattern resembles a sinusoidal curve. III DETERMINANTS OF GAIT (MOTION PATTERNS) In mechanical terms, there are six independent degrees of freedom (Figure 10-4): A Pelvic rotation: The pelvis rotates horizontally about a vertical axis, alternately to the left and right of the line of progression, lessening the center-of-mass deviation in the horizontal plane and reducing the impact at initial floor contact. B Pelvic list: The non–weight-bearing, contralateral side drops 5 degrees, reducing superior deviation. C Knee flexion at loading: The stance-phase limb is flexed 15 degrees to dampen the impact of initial loading. D Foot and ankle motion: Through the subtalar joint, damping of the loading response occurs, leading to stability during midstance and efficiency of propulsion at push-off. E Knee motion: The knee works together with the foot and ankle to decrease necessary limb motion. The knee flexes at initial contact and extends at midstance. F Lateral pelvic displacement: This relates to the transfer of body weight onto the limb. The length of motion is 5 cm over the weight-bearing limb, narrowing the base of support and increasing stance-phase stability. A Agonist and antagonist muscle groups work in concert during the gait cycle to effectively advance the limb through space. B The hip flexors advance the limb forward during the swing phase and are opposed during terminal swing, before initial contact by the decelerating action of the hip extensors. C Most muscle activity is eccentric, which is muscle lengthening while it contracts, and allows an antagonist muscle to dampen the activity of an agonist and act as a “shock absorber” (Figure 10-5). D Isocentric contraction is muscle length’s remaining constant during contraction (Table 10-1). E Some muscle activity can be concentric, in which the muscle shortens to move a joint through space. Abnormal gait patterns are caused by the following factors: A Muscle weakness or paralysis: decreases the ability to normally move a joint through space. A walking pattern develops on the basis of the specific muscle or muscle group involved and the ability of the individual to acquire a substitution pattern to replace that muscle’s action (Table 10-2). B Neurologic conditions: may alter gait by producing muscle weakness, loss of balance, reduced coordination between agonist and antagonist muscle groups (i.e., spasticity), and joint contracture. 1. Hip scissoring is associated with overactive adductors, and knee flexion contracture may be caused by hamstring spasticity. 2. Equinus deformity of the foot and ankle may result in a steppage gait and backwards setting of the knee. C Pain in a limb: creates an antalgic gait pattern, in which the individual shortens the stance phase to lessen the time that the painful limb is loaded. The contralateral swing phase is more rapid. D Joint abnormalities: alter gait by changing the range of motion of that joint or producing pain 1. A hip and knee with arthritis may have joint contractures and reduced range of motion. 2. An anterior cruciate–deficient knee has quadriceps-avoidance gait, which is a net quadriceps moment during midstance that is lower than normal. E Hemiplegia: characterized by prolongation of stance and double-limb support 1. Gait impairment may be excessive plantar flexion, weakness, and balance problems. 2. Associated problems are ankle equinus, limitation of knee flexion, and increased hip flexion. 3. Equinus deformity is surgically corrected 1 year after onset. F Crutches and canes: devices that ameliorate instability and pain, respectively 1. Crutches increase stability by providing two additional loading points. 2. A cane helps shift the center of gravity to the affected side when the cane is used in the opposite hand. This decreases the joint reaction forces of the lower limb and reduces pain. G Arthritis: Forces across the knee may be four to seven times those of body weight; 70% of the load across the knee occurs through the medial compartment. H Water walking: There is a significant decrease in joint and total joint contact forces as a result of the effect of buoyancy. A All or part of a limb may be amputated to treat peripheral vascular disease, trauma, tumor, infection, or a congenital anomaly. B It is often an alternative to limb salvage and should be considered a reconstructive procedure. C Because of the psychologic implications and the alteration of body self-image, a multidisciplinary-team approach should be instituted to help the patient. II METABOLIC COST OF AMPUTEE GAIT A The metabolic cost of walking is increased with proximal-level amputations and is inversely proportional to the length of the residual limb and the number of functional joints preserved. B With a proximal amputation, patients have a decreased self-selected, maximum walking speed. C The higher the level of amputation (or the shorter the stump), the higher the oxygen consumption; thus, the transfemoral amputee with peripheral vascular disease uses close to maximum energy expenditure during normal walking at self-selected velocity (Table 10-3). D Of note is that the required increase in energy expenditure for ambulation in bilateral transtibial amputation (41%) is less than that of unilateral transfemoral amputation (65%). A The soft tissue envelope acts as an interface between the bone of the residual limb and the prosthetic socket. 1. Ideally, it is composed of a mobile, securely attached muscle mass covering the bone end and full-thickness skin that tolerates the direct pressures and “pistoning” (mobility) within the prosthetic socket. 2. It is rare for the prosthetic socket to achieve a perfect, intimate fit. A nonadherent soft tissue envelope allows some degree of mobility of the skin and muscle, thus eliminating the shear forces that produce tissue breakdown and ulceration. B Load transfer (i.e., weight bearing) occurs either directly or indirectly. 1. Direct load transfer (i.e., terminal weight bearing) occurs in knee or ankle disarticulation (Syme amputation). For direct load transfer, intimacy of the prosthetic socket is necessary only for suspension. 2. When the amputation is performed through a long bone (i.e., transfemoral or transtibial), the end of the stump does not take all the weight, and the load is transferred indirectly by the total contact method. A Nutrition and immune status: 1. Patients with malnutrition or immune deficiency have a high rate of wound failure or infection. A serum albumin level of less than 3.5 g/dL indicates that a patient is malnourished. An absolute lymphocyte count of less than 1500/mm3 is a sign of immune deficiency. 2. If possible, amputation surgery should be delayed in patients with stable gangrene until these values can be improved by nutritional support, usually in the form of oral hyperalimentation. 3. In severely affected patients, nasogastric or percutaneous gastric feeding tubes are sometimes essential. 4. When infection or severe ischemic pain necessitates urgent surgery, open amputation at the most distal, viable level, followed by open-wound management, can be accomplished until wound healing can be optimized. B Vascular supply: Oxygenated blood is a prerequisite for wound healing, and a hemoglobin concentration of more than 10 g/dL is necessary. Amputation wounds generally heal by collateral flow; thus, arteriography is rarely useful for predicting the success of wound healing. 1. Standard Doppler ultrasonography helps measure arterial pressure and has been used as the measure of vascular inflow to predict the success of wound healing in the ischemic limb. 2. Transcutaneous partial pressure of oxygen is the current “gold standard” for measurement of vascular inflow. It reflects the oxygen-delivering capacity of the vascular system to the level of contemplated surgery. A Pediatric amputations are usually undertaken because of congenital limb deficiencies, trauma, or tumors. B Congenital amputations are the result of failure of formation. C The current classification system is based on the original work of the 1975 Conference of the International Society for Prosthetics and Orthotics (ISPO) and the subsequent standard developed by the International Organization for Standardization (ISO). D Deficiencies are either longitudinal or transverse, with the potential for intercalary deficits. E Amputation is rarely indicated in congenital upper limb deficiency; even rudimentary appendages can be functionally useful. In the lower limb, amputation of an unstable segment may allow direct load transfer and enhanced walking (e.g., Syme amputation for fibular hemimelia). F In a growing child, disarticulations should be performed only when it is possible to maintain maximum residual limb length and prevent terminal bony overgrowth. 1. The absolute indication for amputation after trauma is an ischemic limb with a vascular injury that cannot be repaired. 2. The guidelines for immediate or early amputation of mangled upper limbs differ from those for mangled lower limbs. 3. Early amputation in appropriate scenarios may prevent emotional, marital, financial, and addiction problems. 4. Most grades IIIB and IIIC tibia fractures occur in young men who are laborers and may be more likely to return to gainful employment after amputation and prosthetic fitting. 5. Sensation is not as crucial in the lower limb as in the upper limb, and current prostheses more closely approximate normal function. 6. Disadvantages of limb salvage: 1. In order for patients to learn to walk with a prosthesis and care for their stumps and prostheses, they must possess certain cognitive capacities: memory, attention, concentration, and organization. 1. A majority of patients who undergo amputation are diabetic, with inherent immune deficiency. 2. The most important risk factors in amputation in diabetic patients are the presence of peripheral neuropathy and development of deformity and infection. 1. Most of the other patients who undergo amputation are malnourished patients with peripheral vascular disease of sufficient magnitude to necessitate amputation, and their coronary and cerebral arteries are diseased. 2. Appropriate consultation with physical therapy, social work, and psychology departments is important to determine rehabilitation potential. 3. Medical consultation helps determine cardiopulmonary reserve. The vascular surgeon should determine whether vascular reconstruction is feasible or appropriate. 4. The biologic amputation level is the most distal functional amputation level with a high probability of supporting wound healing. 5. Morbidity and mortality rates have remained unchanged for several decades. Thirty percent of patients with peripheral vascular disease die in the first 3 months after amputation, and nearly 50% die within the first year. The overall rate of prosthetic use is 43%. A Goal of surgery: to remove the tumor with adequate surgical margins. B Amputation versus limb salvage: 1. Advances in chemotherapy and allograft or prosthetic reconstruction have made limb salvage a viable option in extremity sarcomas. 2. If adequate margins can be achieved with limb salvage, the decision can then be based on expected functional outcome. 3. The advantage of limb salvage over amputation—with regard to energy expenditure to ambulate, quality-of-life measures, and function with activities of daily living—is controversial in the literature. 4. Expected functional outcome should include the psychosocial and body-image values associated with limb salvage. A Skin flaps should be of full thickness, and dissection between tissue planes should be avoided. B Periosteal stripping should be sufficient to allow for bone transection; this minimizes regenerative bone overgrowth. C Wounds should not be sutured under tension. Muscles are best secured directly to bone at resting tension (myodesis) rather than to antagonist muscle (myoplasty). D Stable residual limb muscle mass can improve function by reducing atrophy and providing a stable soft tissue envelope over the end of the bone. E All transected nerves form neuromata. The nerve end should come to lie deep in a soft tissue envelope, away from potential pressure areas. Crushing the nerve may contribute to postoperative phantom or limb pain. F Rigid dressings (postoperative) help reduce swelling, decrease pain, and protect the stump from trauma. G Early prosthetic fitting is done within 5 to 21 days after surgery in selected patients. 1. Phantom limb sensation—the feeling that all or part of the amputated limb is present—occurs in almost all adults who have undergone amputation. It usually decreases with time. 2. Phantom pain is a burning, painful sensation in the part having undergone amputation. It is diminished by prosthetic use, physical therapy, compression, and transcutaneous nerve stimulation. 3. A common cause of residual pain is complex regional pain syndrome (reflex sympathetic dystrophy) or causalgia. Amputation should not be performed for this condition. 4. Localized stump pain is often related to bony or soft tissue problems. 5. Pain referred to the limb occurs in a frequent number of cases. 1. Postoperative edema occurs after amputation. It may impede wound healing and place significant tension on the tissues. 2. Rigid dressings and soft compression help reduce the problem. 3. Swelling occurring after stump maturation is usually caused by poor socket fit, medical problems, or trauma. 4. Persistence of chronic swelling may lead to verrucous hyperplasia, a wartlike overgrowth of skin with pigmentation and serous discharge.
Rehabilitation
Gait, Amputations, Prostheses, Orthoses, and Neurologic Injury
section 1 Gait
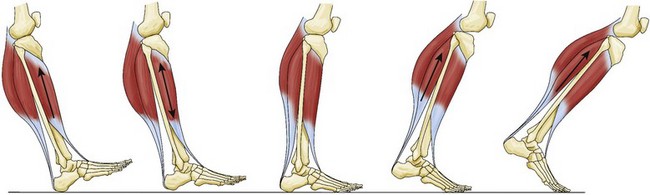
 Starts at initial swing (toe-off) and proceeds with limb acceleration to midswing, when the limb decelerates at terminal swing before the next cycle (Figure 10-3)
Starts at initial swing (toe-off) and proceeds with limb acceleration to midswing, when the limb decelerates at terminal swing before the next cycle (Figure 10-3)
 During initial swing, the hip and knee flex, and the ankle begins to dorsiflex.
During initial swing, the hip and knee flex, and the ankle begins to dorsiflex.
section 2 Amputations
 An absolute Doppler pressure of 70 mm Hg was originally described as the minimum inflow pressure to support wound healing.
An absolute Doppler pressure of 70 mm Hg was originally described as the minimum inflow pressure to support wound healing.
 The ischemic index is the ratio of the Doppler pressure at the level being tested to the brachial systolic pressure. It is generally accepted that patients require an ischemic index of 0.5 or greater at the surgical level to support wound healing. The ischemic index at the ankle (i.e., the ankle-brachial index) is the most accepted method for assessing adequate inflow to the ischemic limb.
The ischemic index is the ratio of the Doppler pressure at the level being tested to the brachial systolic pressure. It is generally accepted that patients require an ischemic index of 0.5 or greater at the surgical level to support wound healing. The ischemic index at the ankle (i.e., the ankle-brachial index) is the most accepted method for assessing adequate inflow to the ischemic limb.
 In the normal limb, the area under the Doppler waveform tracing is a measure of flow. In at least 15% of patients with diabetes and peripheral vascular disease, those values are falsely elevated and not predictive because of the incompressibility and loss of compliance of calcified peripheral arteries. The ischemic index for toe pressure is more accurate in such patients and, if greater than 0.45, is usually predictive of adequate blood flow.
In the normal limb, the area under the Doppler waveform tracing is a measure of flow. In at least 15% of patients with diabetes and peripheral vascular disease, those values are falsely elevated and not predictive because of the incompressibility and loss of compliance of calcified peripheral arteries. The ischemic index for toe pressure is more accurate in such patients and, if greater than 0.45, is usually predictive of adequate blood flow.
 Such overgrowth usually occurs in the humerus, fibula, tibia, and femur, in that order; it is typical in diaphyseal amputations.
Such overgrowth usually occurs in the humerus, fibula, tibia, and femur, in that order; it is typical in diaphyseal amputations.
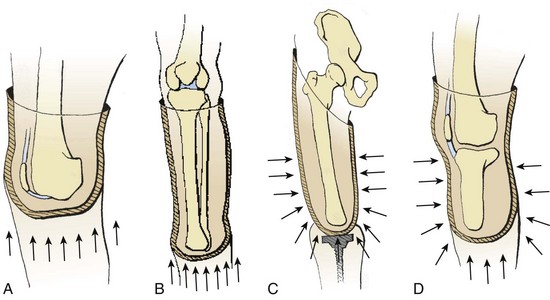
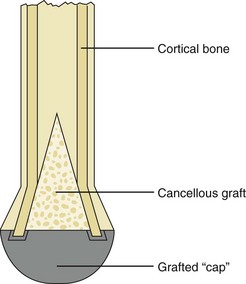
 Numerous surgical procedures have been described to resolve this problem, but the best method is surgical revision of the residual limb with adequate resection of bone or autogenous osteochondral stump capping (Figure 10-7).
Numerous surgical procedures have been described to resolve this problem, but the best method is surgical revision of the residual limb with adequate resection of bone or autogenous osteochondral stump capping (Figure 10-7).
 Severe open tibia fractures that are managed by limb salvage rather than amputation are often associated with high rates of mortality and morbidity as a result of infection, increased energy expenditure for ambulation, and decreased potential to return to work.
Severe open tibia fractures that are managed by limb salvage rather than amputation are often associated with high rates of mortality and morbidity as a result of infection, increased energy expenditure for ambulation, and decreased potential to return to work.
 Limb salvage for Gustillo-Anderson grades IIIB and IIIC open fractures of the tibia and fibula generally has poor functional outcomes and multiple complications, and multiple surgical procedures may be needed.
Limb salvage for Gustillo-Anderson grades IIIB and IIIC open fractures of the tibia and fibula generally has poor functional outcomes and multiple complications, and multiple surgical procedures may be needed.
 The salvaged lower extremity with an insensate plantar weight-bearing surface (loss of posterior tibial nerve), with associated major functional muscle and bone loss, is unlikely to provide a durable limb for stable walking and is a potential source of early or late sepsis.
The salvaged lower extremity with an insensate plantar weight-bearing surface (loss of posterior tibial nerve), with associated major functional muscle and bone loss, is unlikely to provide a durable limb for stable walking and is a potential source of early or late sepsis.
 This level is determined by the presence of adequate, viable local tissue to construct a residual limb capable of supporting weight bearing; an adequate vascular inflow; and serum albumin level and a total lymphocyte count sufficient to aid surgical wound healing.
This level is determined by the presence of adequate, viable local tissue to construct a residual limb capable of supporting weight bearing; an adequate vascular inflow; and serum albumin level and a total lymphocyte count sufficient to aid surgical wound healing.
 The selection of an appropriate amputation level is determined by combining the biologic amputation level with the rehabilitation potential in order to choose the level that maximizes ultimate functional independence.
The selection of an appropriate amputation level is determined by combining the biologic amputation level with the rehabilitation potential in order to choose the level that maximizes ultimate functional independence.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Rehabilitation: Gait, Amputations, Prostheses, Orthoses, and Neurologic Injury