12 Regional injuries
Cases relevant to this chapter
Essential facts
1. Non-operative treatment is used for most clavicle, humeral, distal radial, metacarpal and phalangeal fractures.
2. Gleno-humeral dislocation is the most common major joint dislocation and is associated with an 80% recurrence in younger patients and rotator cuff tears in older patients.
3. Displaced supra-condylar humeral fractures in children are associated with a significant risk of vascular and neurological injury.
4. Distal radius fractures in adults are very common; 30% are unstable in a cast.
5. Scaphoid fractures may not be obvious on initial radiographs and are associated with a risk of avascular necrosis.
6. Intra-capsular hip fractures interfere with femoral head blood supply and are frequently complicated by non-union and avascular necrosis.
7. Extra-capsular hip fractures generally heal after internal fixation.
Upper limb injuries
Fractures of the clavicle and shoulder girdle
Clavicular fractures
These are common injuries in adults and children (Fig. 12.1). The majority of cases follow a fall on the shoulder. Most fractures involve the middle third of the bone. Clinical diagnosis is not difficult in most cases – there is tenderness with visible and palpable deformity at the site of the fracture. A small proportion of these patients have high-energy trauma and in these cases there is an association with brachial plexus injuries and vascular injury. Clinical assessment should include an assessment of the neurovascular status of the upper limb.
Shoulder injuries
Acromio-clavicular dislocations
• Grade I – the acromio-clavicular ligaments are damaged, but there is no superior displacement of the clavicle. Patients are tender on palpation of the joint, but there is no deformity.
• Grade II – the ligaments are damaged sufficiently to allow subluxation, but not complete dislocation of the joint.
• Grade III – there is complete dislocation with superior displacement of the joint. The coraco-clavicular and acromio-clavicular ligaments are torn. This injury is not usually seen in the younger child, but may be seen in adolescents.
Treatment of grade I and II injuries is non-operative with a sling for comfort until early mobilization is commenced 1–2 weeks after injury. Most grade III injuries can also be treated non-operatively. However, occasionally the clavicle is widely displaced and comes to lie in a subcutaneous position. These injuries are best treated surgically. The clavicle can be repositioned using a coraco-clavicular screw.
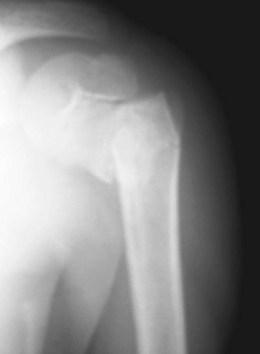
Proximal humeral fractures
Most of these fractures are not markedly displaced and unite reliably with non-operative treatment in a sling in a few weeks. Wide displacement of the fragments or the presence of displaced tuberosity fragments warrants consideration of internal fixation or humeral head replacement (Fig. 12.2). Non-operative treatment is associated with a high rate of mal-union and shoulder stiffness, but operative treatment in osteoporotic bone seldom produces superior functional results, except in the most displaced fracture patterns.
In children the injury may involve the physeal plate (see section on physeal injuries) or the proximal metaphysis (Fig. 12.3). Most injuries can be treated non-operatively and, even if there is noticeable angulation at the fracture site, the proximal humerus has excellent potential for remodelling in the child.
Humeral shaft fractures
Not all humeral shaft fractures can be treated non-operatively. Indications for surgery include:
• Fractures with a brachial plexus palsy
• Fractures associated with a vascular injury
• Humeral fractures associated with an ipsilateral forearm fracture
• Patients with multiple trauma
• Pathological humeral fractures
• Displaced transverse fractures – high risk of non-union with closed treatment.
If surgery is required, plating is the preferred fixation option for most fractures. Intra-medullary nailing is possible, but has been associated with a high rate of non-union and other surgical complications. In children, rigid nails and any fixation device that crosses a physis are not used. Flexible intra-medullary nails or plate fixation are appropriate.
Fractures around the elbow
Distal humeral fractures
Fractures of the distal humerus and metaphysis in children are usually managed non-operatively.
Supra-condylar fractures of the humerus are the commonest elbow injury in children aged 5–7 years and result from a fall on to the outstretched hand. The force is transmitted up the forearm and the humerus fails in the metaphysis, the area of least structural strength. Some 95% of supra-condylar fractures are extension types and the remainder have a flexion pattern. The degree of displacement of the distal fragment may range from being undisplaced to some displacement, but with posterior cortical continuity or complete displacement (Fig. 12.4). Completely displaced fractures may be associated with loss of circulation to the forearm and hand as the brachial artery is trapped in the fracture site. Neurological damage may also occur as peripheral nerves at the elbow are contused or stretched by the injury; the anterior interosseous nerve is affected most commonly (see Chapter 2). Loss of circulation to the hand is a surgical emergency and urgent reduction of the fracture under general anaesthesia is required. Displaced fractures are generally pinned after reduction. Neurological injury is usually managed conservatively and generally carries a good outlook. Healing of the fracture is rapid and the child can begin mobilizing the elbow after 3 weeks. Mal-union of the fracture may occur and cubitus varus (a medial deviation of the forearm) may be seen (Fig. 12.5). This is a cosmetic deformity that does not affect function, but most children and parents eventually find the appearance unacceptable and it can be corrected by supra-condylar osteotomy.
Fracture of the lateral condyle in children (Fig. 12.6) is the second commonest injury at the elbow in children aged 5–7 years. The injury passes through the elbow joint and across the growth plate, and if there is any displacement the fracture is fixed to ensure anatomical reduction of the joint surface and growth plate. If a displaced lateral condyle is not fixed and a non-union ensues, there is a likelihood of the child developing a progressive lateral drift of the forearm and tardy ulnar nerve palsy as an adult. The palsy is due to the ulnar nerve being stretched at the elbow and results in muscle weakness in the hand and difficulty in performing fine hand movements (See Chapter 1 for anatomy review).
Olecranon fractures
The olecranon process is commonly fractured in falls on the elbow. The triceps inserts on to the olecranon and this commonly results in distraction of the fracture. Non-operative treatment is, therefore, seldom feasible. Internal fixation using a tension-band wire system is the most common method of operative treatment (Fig. 12.7). Postoperatively a short period of immobilization is usual for 10–14 days, after which cautious mobilization of the elbow out of a cast may begin. The main complication is failure of fixation with delayed or non-union of the fracture. In children the injury can be treated conservatively if the articular surface has not been disrupted, or surgically if there is loss of continuity of the joint surface.
Radial head and neck injuries
Fractures of the radial head and neck are quite frequent and result as a consequence of a fall on the outstretched hand. Force transmitted up the radial shaft results in a compressive axial force on the radius with a fracture of the head itself, or the neck. Radial neck fractures are often minimally displaced and if the angle subtended by the radial articular surface is less than 30° no specific treatment is needed. Fractures with tilt of the head in excess of 30° usually need to be manipulated or have open reduction and fixation. Complete dislocation of the radial head may require radial head replacement. In children, an angulation of up to 20° can be accepted, but a greater tilt is an indication for closed reduction, which can be achieved by manipulation or by using a percutaneous wire to reduce the fracture (Fig. 12.8).
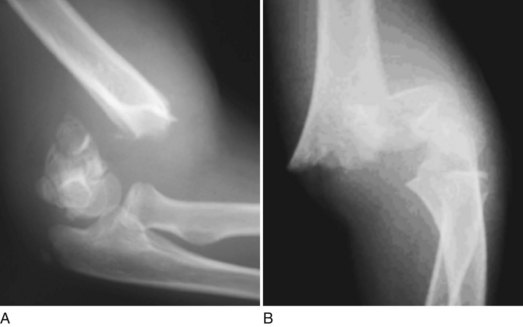
Elbow dislocations and fracture dislocations
The elbow may dislocate as a result of a fall on the outstretched hand with the elbow extended. The olecranon and radial head dislocate in a postero-lateral direction. Neuropraxia of the nerves round the elbow is an occasional complication. Closed reduction can be achieved in the majority of cases by application of manual traction with the elbow slightly flexed. Sedation is necessary, but general anaesthesia is not generally required. The elbow is usually stable after reduction. After 10–14 days of immobilization in a back-slab plaster, the elbow is mobilized. Some high-energy dislocations are associated with more extensive degrees of soft-tissue disruption and the joint may be unstable. In the majority of these adult cases, exploration of the elbow with ligament repair is necessary. The same principles apply to children (Fig. 12.9), except that operative repair of disrupted ligaments is not usually indicated. The injury may also be associated with an avulsion of the medial epicondyle, which can then be incarcerated in the joint as a result of either the injury or the subsequent reduction. If this occurs, the elbow should be opened, the fragment retrieved and pinned back in place (Fig. 12.10).
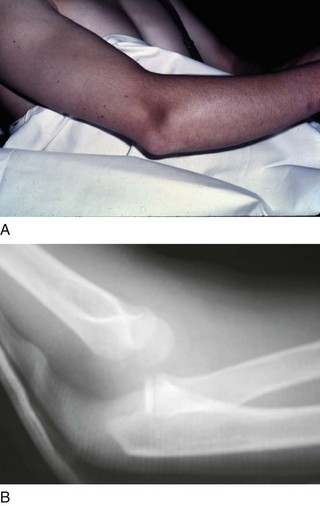
FIGURE 12.9 (A) Elbow dislocation showing visible deformity. (B) Plain radiograph showing posterior dislocation
Fractures of the forearm
Fractures of the forearm are very common injuries in children, but much less common in adults. The peak age of fractures in children is between the age of 5 and 12 years, and fractures in this age group account for 50% of children’s fractures. These injuries vary from plastic deformation (Fig. 12.11), to greenstick fractures, to complete fractures, and many can be treated by closed manipulation and an above-elbow cast. Cast treatment is generally continued for 3–5 weeks depending on the age of the child. At that stage, healing is sufficiently advanced to allow cast removal and mobilization. Complications are uncommon, but mal-union occasionally occurs. Rotational mal-union is poorly tolerated in the forearm particularly and results in loss of forearm rotation. To avoid this complication children should be reviewed and radiographs taken 1 and 2 weeks following reduction. Open reduction and fixation with flexible nails or plates is indicated if a satisfactory alignment cannot be achieved or if the child is approaching skeletal maturity.

FIGURE 12.11 Antero-posterior (left) and lateral (right) radiographs of forearm in a child showing plastic deformity
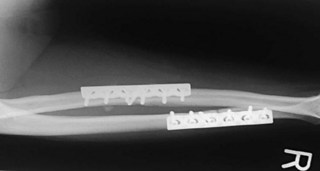
Forearm fractures in adults are more often a consequence of high-energy trauma. Compartment syndrome is a well recognized complication. Most mid-shaft forearm fractures are completely displaced and are not readily amenable to non-operative treatment. Internal fixation with plates is the treatment of choice (Fig. 12.12). Failure to achieve anatomical reduction is associated with loss of the range of pronation and supination. Non-union and infection can complicate surgical treatment, but rates are usually less than 5%. Cross-union between the forearm bones after fracture complicates 2% of injuries and is more common in proximal third fractures, particularly in patients who have delayed fixation, head injury or those who develop infection.
Two patterns of forearm fracture dislocation occur and are eponymously known as the Monteggia fracture dislocation and the Galeazzi fracture dislocation. The Monteggia is the more common pattern and is characterized by an ulnar shaft fracture and a radial head dislocation. The Galeazzi pattern is a radial shaft fracture and a dislocation of the distal radio-ulnar joint. Good-quality radiographs including elbow and wrist joints are necessary in all forearm injuries to avoid missing associated dislocations at these joints. These patterns are also seen in children (Fig. 12.13) and, although internal fixation is indicated in all forearm fracture dislocations in adults, it is possible to manage these fracture patterns in children conservatively, provided that a reduction of the radial head in the Monteggia fracture and the radio-ulnar joint in the Galeazzi fracture can be obtained and maintained. If this is not possible, surgical management is required. Closed reduction of radial head dislocations may be possible, but open reduction and soft-tissue repair is indicated if a stable closed reduction cannot be achieved. For distal radio-ulnar dislocations, additional fixation of the joint may be required. Typically the ulna has dislocated dorsally with respect to the radius. Kirschner wire fixation of the ulna to the radius should be used in patients who have an unstable joint following reduction. These wires require removal at 6 weeks to allow the patient to restore forearm rotation.
Fractures at the wrist
In children the equivalent injuries are fractures through the distal metaphysis and physeal injuries, the commonest of which is the Salter–Harris II pattern. All the typical fracture patterns are seen in this region (see Chapter 11 on children’s injuries). Median nerve symptoms may be seen in the bayonet fracture pattern (Fig. 12.14), where there is an overlap of the fragments.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree