(1)
Department of Orthopedic Surgery Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands
Abstract
Recurrent dislocation of the peroneal tendons is a disabling condition, due to persistent symptoms of pain and instability. Dislocations or subluxations of the tendons are in most cases related to sports injuries. In this chapter, we describe an endoscopic groove-deepening procedure by means of a three-portal technique. This technique is the standard two-portal hindfoot approach in the prone position with the addition of one more superior posterolateral portal.
Endoscopic groove deepening is a good treatment for recurrent peroneal tendon dislocation.
24.1 Introduction
Monteggia was the first to describe peroneal tendon instability in a ballet dancer in 1803 (Kollias and Ferkel 1997; Mason and Henderson 1996; Safran et al. 1999). Thereafter, many authors followed describing the anatomy, mechanism of injury, radiographic findings, and their operative procedures for the treatment of peroneal tendon instability (Kollias and Ferkel 1997; Kumai and Benjamin 2003; Mason and Henderson 1996; Nicholas and Hershman 1986; Marti 1977; Kelly 1920; Jones 1932). Peroneal tendon dislocation or subluxation is reported to be between 83 and 95 % of cases related to sports injuries (Kollias and Ferkel 1997; Kumai and Benjamin 2003; Tourne et al. 1995; Mason and Henderson 1996; Safran et al. 1999). Skiers are at particular risk, but these injuries can also occur in soccer, American football, running, gymnastics, tennis, ballet, basketball, and skating (Kollias and Ferkel 1997; Tourne et al. 1995; Safran et al. 1999). In general, the peroneal dislocation is the result of a single traumatic event that occurs while the foot is dorsiflexed, abducted, and everted (Kollias and Ferkel 1997; Mason and Henderson 1996; Orthner et al. 1989) (Fig. 24.1).
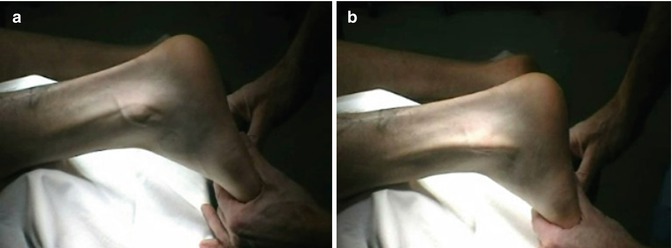
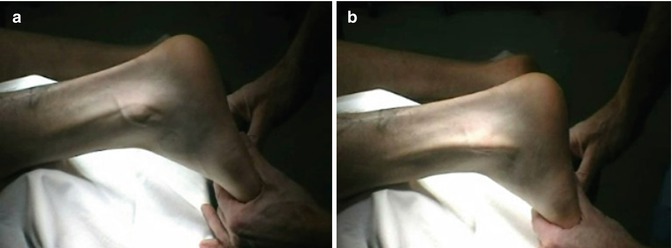
Fig. 24.1
A patient with recurrent peroneal tendon dislocation left ankle. (a) The tendons are located behind the lateral malleolus. (b) In dorsiflexion and eversion the tendons dislocate over the fibula
24.2 Anatomy and Injury Mechanism
The tendons of peroneus longus and brevis pass the ankle on the posterior side wrapping around the lateral malleolus and lie in a malleolar groove (MG) (Kumai and Benjamin 2003). This MG is formed by a periosteal cushion of fibrocartilage that covers the bony groove (Kumai and Benjamin 2003). The tendons are held in their position within the MG by the superior peroneal retinaculum (SPR) (Kumai and Benjamin 2003) (Fig. 24.2). The features of the posterior surface of the fibula have been well documented by Edwards, Pöll, Mabit, and Kumai. In 1928, Edwards examined 178 dry fibulas and found in 82 % of the cases that it was concave; the remaining 18 % was either flat (11 %) or convex (7 %) (Edwards 1928). In 1984, Poll examined 25 distal fibulas and found 28 % to be either flat or convex (Mabit et al. 1999). Kumai found that the distal posterior part of the malleolus was convex and that the groove was primarily formed by a thick, fibrocartilaginous periosteum (Kumai and Benjamin 2003). This periosteum helps the tendons mould their shape to MG and therefore reduce the risk of tendon displacement (Kumai and Benjamin 2003). More proximal, the bone itself is grooved and the periosteum is thinner and purely fibrous (Kumai and Benjamin 2003). After a CT scan study, Mabit also found three types of morphological variations in the MG. In 70 % of cases the groove was shaped concave and the rest was either flat or convex (Mabit et al. 1999). The average width of the groove was 9 mm (Mabit et al. 1999). They compared their results on patients with peroneal tendon dislocations and found an osseous dysplasia concerning the groove depth and/or a torsional insufficiency (Mabit et al. 1999). Orthner also found the depth of the MG as a predisposing factor for peroneal tendon dislocation (Orthner et al. 1989).
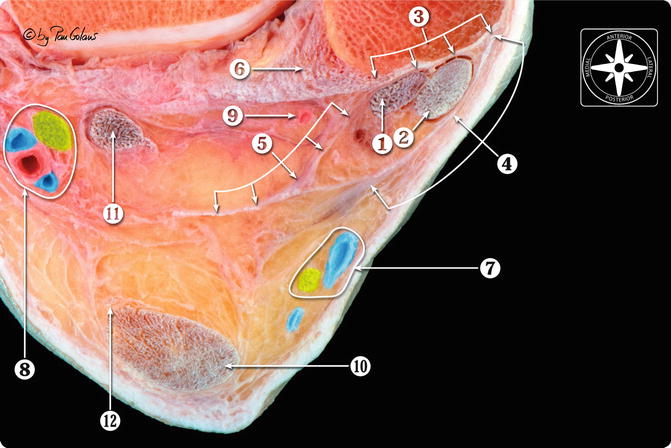
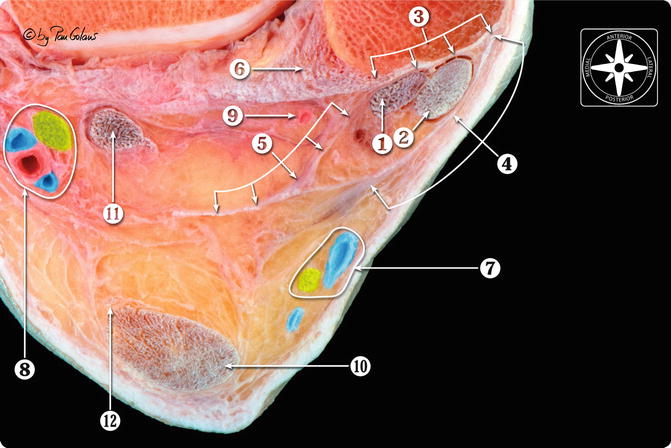
Fig. 24.2
Transversal section at the level of malleolar groove. 1 Peroneus brevis tendon, 2 peroneus longus tendon, 3 malleolar groove, 4 superior peroneal retinaculum, 5 floor of the fibrous peroneal tendon sheath, 6 posterior tibiofibular ligament, 7 sural nerve and small saphenous nerve, 8 posterior neurovascular bundle (tibial nerve and posterior tibial artery and veins), 9 posterior peroneal artery, 10 calcaneal or Achilles tendon, 11 flexor hallucis longus tendon, 12 plantaris tendon (With kind permission of © Pau Golanó 2013)
Purnell performed a sequential sectioning of the retinaculas to evaluate their function in peroneal stability (Purnell et al. 1983). They concluded that the superior retinaculum is the important restraining force in holding the peroneal tendons in their normal anatomic positions (Purnell et al. 1983). After a series of 73 surgical explorations of acute peroneal tendon dislocations, Eckert concluded that it is not the superior retinaculum that is torn but the retinaculum with the periosteum being stripped off from the fibula (Eckert and Davis 1976). Eckert graded three types of pathoanatomical situations and grade I was found in more than 50 % of cases (Eckert and Davis 1976) (Table 24.1).
Grade I | The retinaculum with the periosteum is stripped off the lateral malleolus with the tendons lying between the periosteum and bare bone (51 %) |
Grade II | The distal 1–2 cm of the dense fibrous lip is elevated along with the retinaculum and periosteum (33 %) |
Grade III | A thin cortical rim of bone is avulsed along the fibrous lip, retinaculum, and the periosteum (16 %) |
A peroneal tendon dislocation is the result of a single traumatic event that occurs while the foot is dorsiflexed, abducted, and everted, and the peroneal muscles strongly contracted, but other positions have been reported (Kumai and Benjamin 2003; Mason and Henderson 1996; Safran et al. 1999; Orthner et al. 1989).
Because of the three-dimensional movements of the foot at the subtalar and ankle joints, the highest risk of subluxation is at the distal end of the MG (Kumai and Benjamin 2003). Proximally, the relationship between the tendons and the MG is more stable, because the tendons are further away from the ankle and subtalar joints and the bony MG is deeper (Kumai and Benjamin 2003).
The greatest risk of dislocation is when the foot is on the ground and the peroneal muscles work with a fixed insertion and a movable origin (Kumai and Benjamin 2003). Other authors report that regardless of the position of the ankle, the causative movement in acute peroneal tendon subluxation is a forceful contraction of the peroneal muscles, and this is sufficient to elevate the posterior periosteal attachment of the superior peroneal retinaculum of the fibula (Mason and Henderson 1996).
24.3 Treatment Options
For the patient with an acute peroneal tendon injury, it is difficult to make a definite statement regarding the outcome of nonoperative treatment options (Mason and Henderson 1996). Results of cast and soft compression dressings, position of the ankle, the duration of immobilization, and weight bearing influence the outcome (Mason and Henderson 1996; Eckert 1976). The results of the studies show that nonoperative treatment options are unpredictable and have high incidences of redislocations (Mason and Henderson 1996; Eckert 1976). Operative treatments on the other hand have excellent results, and therefore, this treatment is the treatment of choice (Table 24.2).
Table 24.2
Literature overview of treatment for recurrent peroneal tendon dislocation
Author | Date | Pat | A | C | Technique | Results |
|---|---|---|---|---|---|---|
Tourne | 1995 | 35 pat | 12 | 24 | Meary → 25 | 92 % satisfactory result |
Exner Suture→ 8 | ||||||
Mason | 1996 | 10 pat | 11 | SPR repair + fibular rotation osteotomy | 9 out of 11 excellent | |
One reoperation for resubluxation | ||||||
Karlson | 1996 | 15 pat | 15 | SPR repair + MG deepening | 87 % (13/15) results satisfactory, with full range of motion and no pain | |
Hutchinson | 1994 | 20 pat | 20 | MG deepening | ||
Steinbock | 1994 | 12 pat | 10 | 3 | Transposition of peroneal tendons under calcaneofibular ligament | 11 of 13 had excellent results |
Micheli | 1989 | 12 pat | 12 | Sliding fibular graft | 11 of 12 had excellent results, one reoperation | |
Slatis | 1988 | 4 pat | 4 | MG deepening but maintaining cartilaginous layer | All excellent | |
Behfar | 1987 | 13 pat | 13 | Viernstein | 12 of 13 resumed sports and no redislocations | |
Martens | 1986 | 9 pat | Transposition of peroneal tendons under calcaneofibular ligament | All 11 ankles, excellent or good results | ||
Two cases of sural nerve paresthesia
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





