Fig. 7.1
a Previously treated thumb with inadequate padding. b Previously treated thumb with full-thickness skin necrosis of the volar pad. c Previously treated thumb in a child with skin graft and a scar contracture of the IP joint. d Irreparable nerve damage to both digital nerves of the thumb with loss of sensory function. (Courtesy of G. Rayan MD)
Any of these flaps may be employed to provide soft tissue coverage for a thumb tip with a full-thickness skin defect or to restore supple, sensate skin to a thumb that has skin coverage that lacks those qualities. Selection of the appropriate soft tissue reconstruction technique is dependent upon the character of the thumb-tip injury and the patient’s goals and expectations.
Management of extensive thumb injuries such as amputations proximal to the IP joint and degloving injuries is beyond the scope of this chapter but will be briefly discussed.
Flaps for Coverage of Thumb-Tip Injuries
Moberg Advancement Flap
The Moberg advancement flap (MAF) is a bipedicled, axial-pattern, cutaneous, advancement flap that was first proposed in 1964 by Erik Moberg. The procedure was originally described to restore sensibility to a thumb tip with intact but denervated skin [3]. It is most commonly used to provide skin coverage for amputations or partial degloving of the thumb tip and sometimes for other digits.
Anatomy
Both the radial and ulnar digital arteries of the thumb serve as vascular pedicles to the MAF. It is possible that the flap may survive on a single pedicle, but whenever possible both vascular structures should be present and elevated with the flap to ensure adequate vascular flow. Sensory function is maintained by preserving the paired digital nerves traveling with the arteries.
The dorsal skin of the fingers is supplied by the palmar digital arteries; therefore, using an MAF for fingertip injuries may compromise its circulation. In contrast to the other digits, the dorsal skin of the thumb receives its own blood supply from the dorsal digital arteries. This allows the palmar skin of the thumb to be elevated with both digital arteries as an axial flap without concern about dorsal ischemia.
Indications
The MAF is best suited for pulp tip defects distal to the IP joint and tip amputations measuring 2 cm2 or less (Fig. 7.2a–f). It is not indicated for larger defects because of potential complications [4]. Palmar, oblique loss of the pulp creates a defect particularly well suited for coverage with an MAF. The flap may also be used to replace scars at the tip or restore sensibility to an insensate digital tip as originally described.
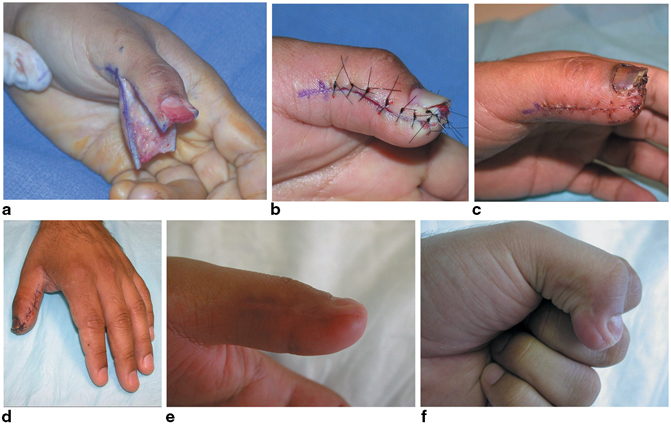
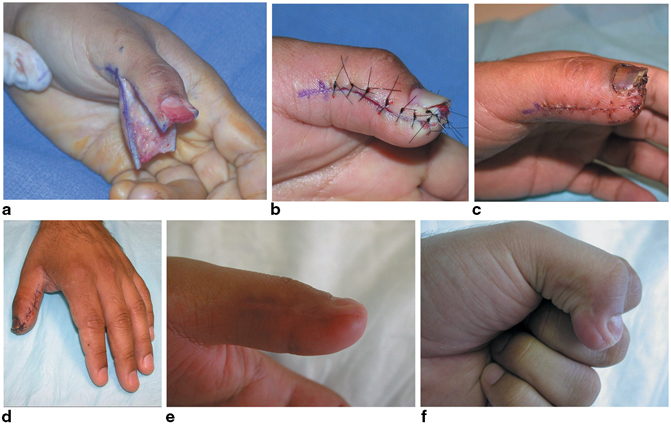
Fig. 7.2
a Intraoperative picture of thumb-tip amputation with Moberg advancement flap (MAF) elevation in progress. b Flexed thumb IP joint with MAF inset to cover thumb-tip amputation. c Thumb appearance at 3 months with early healing. d Thumb appearance at 3 weeks showing maintained first web space. e Full IP joint extension 4 months following MAF coverage. f Satisfactory IP joint flexion 4 months following MAF coverage. (From [23]. Used with permission from the American Society for Surgery of the Hand)
Relative contraindications for the MAF include: elderly patients (especially those with advanced arthritic changes), injury to one or both vascular pedicles of the thumb, soft tissue defect greater than 2 cm2, and defects proximal to the IP joint.
The use of this flap in the digits has been considered to be a relative contraindication because of the higher risk of dorsal skin necrosis. In fingertip amputations , however, part of the dorsal skin is missing, which lessens the concern about the dorsal skin vascularity. Successful use of Moberg palmar advancement flaps in the fingers, however, has been reported. When this technique is adopted for these digits, the dissection should be modified to preserve the perforating vessels that extend from the palmar to the dorsal aspect of the digit. [5–13]
Surgical Technique
The MAF is typically preformed within a few days of thumb injury, but the timing of coverage is not critical to the outcome. The procedure should be performed as soon as the patient’s condition allows. Satisfactory results can be achieved even after several days of delay, provided that the wound is tidy and free of infection at the time of flap coverage.
Prior to flap elevation, the wound should be irrigated and debrided of any foreign material or nonviable tissue. Associated fractures and nail bed injuries should also be addressed prior to flap elevation. The wound margins should be freshened while preserving all viable tissues.
Flap elevation begins with midlateral incisions on the radial and ulnar aspects of the thumb. Dissection should be dorsal to the neurovascular structures towards the flexor tendon sheath (Fig. 7.3a–d). The flap is elevated from distal to proximal. Sometimes the severed digital nerve branches may be divided sharply 5 mm proximal to the skin edge to avoid creating painful neuromas at the thumb tip. The flap is freed of all dorsal attachments and mobilized proximally to the level of the metacarpophalangeal (MP) joint in order to maximize its distal advancement. Proper elevation of the flap should allow advancement of up to 2 cm.
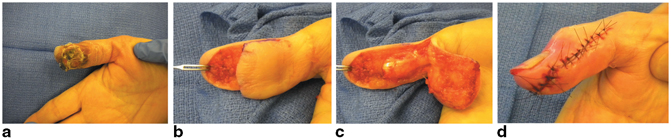
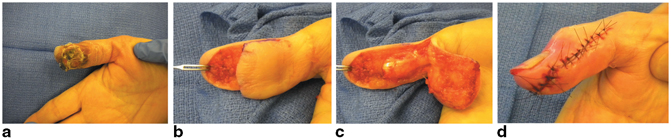
Fig. 7.3
a Complex soft tissue injury of thumb pulp. b Full-thickness soft tissue defect of thumb tip following debridement. c Completed elevation of Moberg advancement flap. d The flap after inset with interphalangeal joint flexion to increase distal advancement. (Courtesy of G Rayan MD)
The tourniquet should be deflated, hemostasis obtained, and the wound irrigated prior to flap inset. The flap is advanced distally, which may require flexion of the IP joint and, to some degree, the MP joint to allow maximum coverage of the defect and for the flap to reach the tip of the thumb. The extent of flexion usually does not exceed 30–45°. If additional flexion is necessary for adequate coverage, then one of this flap’s modifications described below may be considered.
Complete full-thickness skin coverage of the thumb tip is not essential. A small area of exposed subcutaneous tissue will re-epithelialize and should not have considerable adverse effect on the final functional or cosmetic outcome.
The flap is inset and skin closure is done with 4–0 or, preferably, 5–0 nylon. In children, chromic catgut suture is preferable. Sutures can be placed through the nail plate distally if necessary. The thumb is dressed with non-adherent gauze and immobilized in a thumb spica splint that extends beyond the tip.
Postoperative Care
Splinting is continued for up to 3 weeks depending on concerns about patient compliance or the condition of the flap. Early active range of motion (ROM) is preferred and may begin at 7–10 days postoperatively. The patient is instructed to begin scar massage techniques at 4–6 weeks postoperatively to soften and desensitize the scar. Formal hand therapy may be required if the patient has a great deal of stiffness, especially in the presence of incipient or mild arthritic changes, or scar hypersensitivity .
Technical Modifications
Using this flap requires flexion of the IP joint. This commonly results in mild loss of IP joint hyperextension or stiffness, especially in older patients. Modifications to the MAF have been proposed in order to minimize the degree of flexion necessary to extend the flap to the tip.
Flap advancement may be enhanced to some degree by placement of Burrow’s’ triangles (Fig. 7.4a–c) or z-plasties (Fig. 7.5a–c) at the proximal aspect of the lateral incisions [4, 13].
Fig. 7.4
a Burrow’s triangles excised at the base of the flap on both sides facilitate distal advancement. b The triangular defects are closed increasing the advancement of the flap toward the tip. c Final appearance of Moberg advancement flap after advancement. (From: [35]. Used with permission from the American Society for Surgery of the Hand)
Fig. 7.5
a Z-plasty flaps are raised at the base of the flap on both the radial and ulnar sides. b Transposition of the Z-plasty flaps facilitates distal advancement of the flap toward the tip. c Final appearance of Moberg advancement flap after advancement. (From: [35]. Used with permission from the American Society for Surgery of the Hand)
O’Brien [9] proposed a transverse incision of the skin flap proximally, preserving the neurovascular structures. This creates a bipedicled island flap and increases the flap reach to the tip, lessening the degree of IP joint flexion (Fig. 7.6). The secondary defect created proximally is covered with a full-thickness skin graft, or with triangular flaps from both sides of the thumb [10]. The island flap concept has been further modified by fashioning the mobilized skin island as a homodigital V flap and performing a V–Y closure at the proximal aspect, eliminating the need for a skin graft [11, 12].
Fig. 7.6
An illustration of island modification of Moberg advancement flap. (From: [35]. Used with permission from the American Society for Surgery of the Hand)
Outcome
Experience with the Moberg flap is typically rewarding (Fig. 7.7a–d). Modifications to extend the reach of the flap are rarely required, and failure of the flap is rare, although limited marginal necrosis may occur. Final ROM is usually near normal, but a small loss of IP joint hyperextension is not uncommon. Sensory function is usually equal or near that of the contralateral thumb, and most patients can return to their normal activities and work after healing is complete.
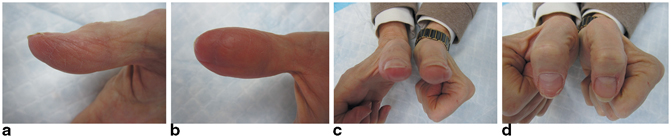
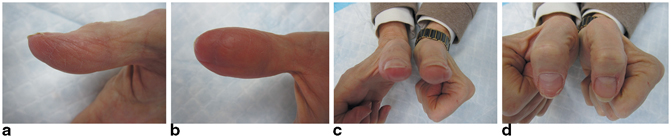
Fig. 7.7
a, b Full restoration of soft tissue coverage of thumb tip was achieved with a Moberg advancement flap with adequate soft tissue padding and near normal sensory function. c, d There is no residual flexion deformity and the patient returned to work and hobbies without limitations. (Courtesy of G Rayan MD)
Complications
Stiffness: Some loss of IP joint hyperextension can be expected, but is unlikely to be dysfunctional. Arthritic changes in the thumb may increase the risk of stiffness. Pinning of the thumb in flexion may also contribute to loss of motion and is not recommended. Although no improvement in outcome has been shown by any of the described modifications, theoretically they enhance flap advancement and decrease the IP flexion required and may improve final ROM [4]. Early ROM exercises help prevent stiffness.
Neuroma: Some risk of digital neuroma formation exists after the use of this flap due to the associated nerve injury. The reported incidence is low however at 0–10 % [4, 10]. Sharp transection of the digital nerve branches just proximal to the edge of the skin may help prevent this complication.
Cold Intolerance: This is a common side effect following management of fingertip injuries with any reconstructive procedure. This problem is not necessarily more common after this procedure and it spontaneously resolves with time in most patients In one report, over 30 % of patients had severe symptoms of cold intolerance [4]. Therapeutic modalities and topical agents may alleviate some of these symptoms if they are severe. Using thermal, well-padded gloves to keep the hand warm is the most effective treatment measure. Patients should be counseled prior to surgery about this expected consequence.
Pulp Instability: Poor adherence of the flap to the deeper structures at the tip of the thumb may cause instability of the pulp during pinch. This is an uncommon sequela and typically mild in nature, but may be of functional importance. This may be related to “bowstringing” of the flap that occurs when excessive flexion of the IP joint is required for inset. Using one of the flap modifications to decrease the amount of flexion required to achieve coverage may lessen the risk of this complication.
Nail Deformity: This is not uncommon when the original injury involves a large portion of the nail bed. Careful attention to accepted principles of treatment for fingertip amputations and nail bed injuries will minimize the incidence of this complication.
Dorsal Skin Necrosis: This complication is rarely encountered when the flap is harvested in the thumb without injury or anomaly of the dorsal blood supply. In the other digits, the dorsal skin is at risk for this problem; therefore, care must be taken to preserve the communicating branches from the digital vessels in the flap.
Neurovascular Island Flap
The NVI flap is an axial flap transferred on a pedicle consisting of a digital artery , sensory nerve, accompanying veins, and fascia. It was first described by Littler in 1960 to restore sensory function or coverage of a thumb defect [14]. The classic NVI flap is a fasciocutaneous flap transferred from the ulnar side of the long or ring finger to the thumb pulp [15–17].
Indications
The NVI flap is indicated for coverage of full-thickness thumb-tip defects of greater size or a pattern which is not amenable to Moberg flap coverage. It may also be used to resurface a severely scarred thumb pulp, and restore sensory function to an insensate thumb [15–17]. Finally, it can be used as an adjunct flap to provide sensibility after an insensate soft tissue resurfacing procedure such as a groin or other tubed flap or in osteoplastic thumb reconstruction of more extensive injuries [15, 17] (Fig. 7.8a–e).
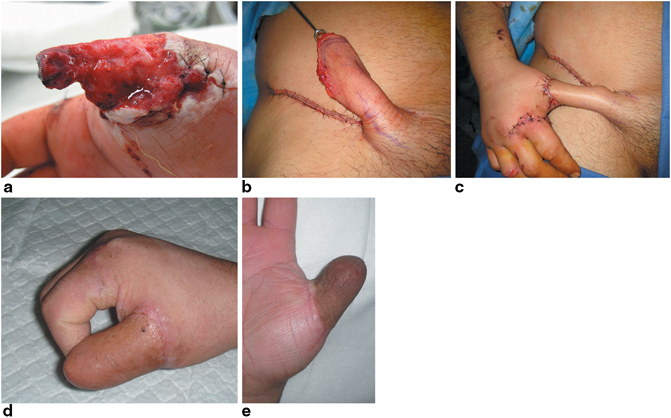
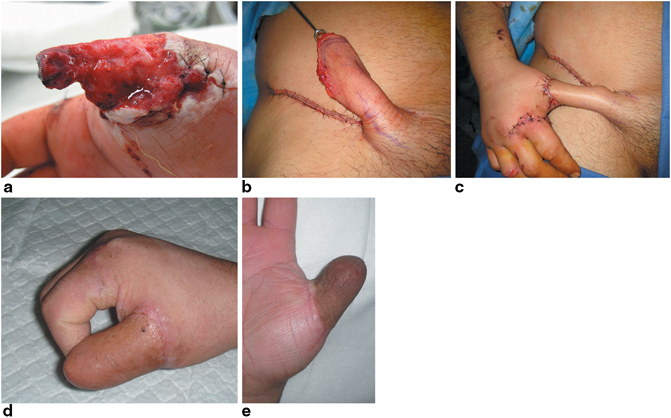
Fig. 7.8
a Extensive thumb degloving injury not suitable for Moberg advancement flap coverage. b Elevated groin flap. c inset groin flap d, e healed groin flap. Degloving injury has adequate soft tissue coverage, but absent sensibility. a, c, d, e. (From: [36]; Figs. 44.3a, b, c. Used with permission from Thieme. b Courtesy of G Rayan MD)
Relative contraindications for NVI flap reconstruction include a history of heavy smoking, atherosclerosis, diabetes, connective tissue diseases, or vasospastic disorders. Since the flap sacrifices a portion of a healthy digit, the benefits of correcting the thumb defect should outweigh the deficit created in the donor digit [15].
Surgical Technique
Selection of the donor site should be done before the patient is brought to the operating room. The donor finger must have normal innervation in an area that is less essential to hand function. Sensibility is essential on the palmar aspect of the thumb and the radial sides of the index and long fingers during opposition and fine manipulation. Sensibility on the ulnar side of the small finger is important in protection of the hand. The ulnar sides of the ring or long fingers are less essential to hand function and may be suitable donor sites for this flap [16]. Since it is supplied by the ulnar nerve, the ulnar side of the ring finger is the preferred donor in cases where there is median nerve damage [15].
The donor finger must also have a robust blood supply. The digit that shares the web space with the donor flap digit must have an intact digital artery on its unshared side. The proper digital artery to this neighbor digit shares a common digital arterial origin with the flap pedicle and will be divided during flap harvest. A digital Allen’s test or handheld Doppler is used to assess the status of the digital arteries to the donor and neighboring digits. If the history or physical examination raises concerns about arterial patency, preoperative digital arteriography may be required. However, this is rarely necessary. The final assessment of adequacy of perfusion is made during dissection of the pedicle.
In the operating room, and under tourniquet control, the soft tissue defect should be irrigated and debrided of any nonviable tissue or foreign debris; it should be clean and free of contamination or evidence of infection. If the flap is used to provide sensation to a thumb with intact skin, a primary defect must be created. Ideally, this defect is created on the ulnar thumb pulp with its most distal aspect 3 or 4 mm proximal to the thumb tip. This full-thickness skin defect is raised with a knife, keeping the volar fat pad intact underneath. The skin can be preserved as a skin graft for donor-site resurfacing if possible. Any painful neuromas can be resected and buried within the thenar or adductor muscles at this time. A zigzag incision is marked on the volar aspect of the thumb from the defect to the MP flexion crease. The volar zigzag incision flaps are raised to expose the bed for the transferred pedicle. As such, they should be free of constriction points. Alternatively, the skin proximal to the thumb defect can be left intact to tunnel the flap beneath it after it is raised.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








