Surgical Reconstruction of the Diabetic Charcot Foot
Internal, External or Combined Fixation?
Keywords
• Charcot foot • Diabetes mellitus • Internal fixation • External fixation • Surgery • Reconstruction
Treatment goals for the diabetic Charcot foot
The ultimate goal of deformity correction in diabetic CN patients is to provide a functional lower extremity that is resistant to ulceration or infection. Diabetic limb salvage in CN patients should lead to improvement of a patient’s daily activities of living, provide an ambulatory status with or without bracing, and improve the patient’s overall quality of life.1–5
In addition, maintenance of a stable plantigrade foot may be achieved with prolonged postoperative bracing and accommodative shoe gear to avoid catastrophic postoperative complications that can lead to recurrence of deformity, skin and osseous breakdown, and eventual lower extremity amputation.6–8
Clinical decision making for diabetic Charcot foot fixation
Internal Fixation
Medial plating techniques may be beneficial to address certain CN midfoot deformities with severe abduction or to provide stability to multiple transverse joints of the midfoot. Plate fixation in this manner is placed on the tension side of the deformity. In addition, plate fixation along the medial column allows the placement of screws to cross multiple cortices of the metatarsal and tarsal bones, improving the screw purchase and overall construct stability. Locking plates create a fixed-angle construct by attaching the screw to the plate. These devices were developed to improve fixation in osteoporotic bone, and careful consideration is needed to determine if adequate bone purchase is achieved, since the screw is rigidly attached to the plate. Other plating systems have combined locking and nonlocking abilities for certain osseous pathologies and anatomic placements.3,4
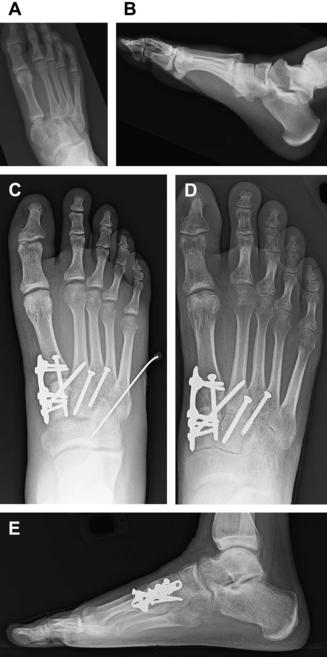
Plate fixation to stabilize the rearfoot or ankle can be used if the soft tissue envelope permits and the CN deformity if free of any ulceration or infection. Various plates and plating techniques have been described. Blade plate fixation is a fixed angle construct providing superior stability to stabilize rearfoot and ankle arthrodesis. Numerous anatomic rearfoot and ankle plating systems have been developed allowing for compression and the use of locking screws. The use of various nonanatomic plates such as the femoral and humeral plates has also been described. These plates are typically selected because of their rigidity and strength while providing multiple screw options to gain purchase into the calcaneus. Plate placement for ankle and rearfoot arthrodesis is dependent on the plane of deformity, previous surgical reconstruction, soft tissue envelope, and presence of ulceration. Lateral, anterior, and posterior approaches have all been performed. Incision placement must be carefully planned, especially if bone resections and shortening of the lower extremity are being performed, as these can result in significant tension on the surgical incisions. These clinical case scenarios need to be considered in detail before fixation constructs are placed to prevent poor soft tissue closure and postoperative complications (Fig. 1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree