6 Rationale for the use of HVLA thrust techniques
High-velocity low-amplitude (HVLA) thrust techniques are widely used in patient care with increasing evidence of their effectiveness. However, the use of HVLA thrust techniques must be considered within the context of a comprehensive patient management plan, which may include the application of other osteopathic manipulative techniques and adjunctive therapies.
Various authors have described specific indications for the use of HVLA thrust techniques (Box 6.1).
Box 6.1 Specific indications for HVLA thrust techniques as listed by various authors
Cavitation Associated With Hvla Thrust Techniques
Research involving the metacarpo-phalangeal joint indicates that the audible release is generated by a cavitation mechanism resulting from a drop in the internal joint pressure.29–32 Following cavitation, there is an increase in the size of the joint space and gas is found within that space.29–33 The gas bubble has been described as 80% carbon dioxide30 or having the density of nitrogen.14 The gas bubble remains within the joint for between 15 and 30 minutes,14,29–31,33 which is consistent with the time taken for the gas to be reabsorbed into the synovial fluid.30 An increased range of joint motion immediately following cavitation has been demonstrated.33
The audible release in the lumbar spine is believed to originate from the apophysial joints.34 Widening of lumbar zygapophysial joints post manipulation has been demonstrated by magnetic resonance imaging (MRI) following lumbar spine manipulation.35 The situation in the cervical spine is less clear as neck manipulation did not demonstrate similar post-manipulation apophysial joint space widening when assessed using computerized tomography (CT).36
A number of studies have reported that thrust techniques are associated with a temporary increase in the range of spinal motion.37–45 Longer-term effects of HVLA thrust techniques have also been reported46,47 and it is postulated that these may be due to reflex mechanisms that either directly cause muscle relaxation or inhibit pain.5 However, the sound of a ‘crack’ or ‘pop’ associated with a HVLA thrust technique does not necessarily indicate that reflex or tissue changes have occurred. Some authors have reported benefits from HVLA thrust techniques without the accompanying audible release.48,49 There continues to be speculation as to the level and side of apophysial joint cavitation when HVLA thrust techniques are applied to the spine.50–53 It is likely that the level and side of cavitation will be dependent upon a range of factors that might include spinal positioning and locking, the specific technique applied, operator skill and patient compliance and whether the patient is symptomatic or asymptomatic. The aim of HVLA thrust techniques is to achieve cavitation within the normal range of zygapophysial joint motion and not at the anatomical end range.
Repeated ‘cracking’ or ‘popping’ of the joints of the hand, associated with cavitation, has not been shown to be linked with an increased incidence of degenerative change.54,55
Evidence Summary
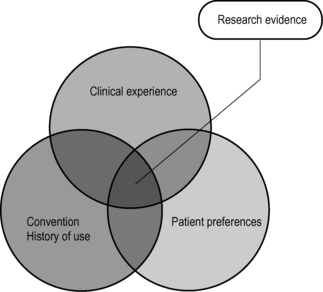
Best practice requires practitioners to embrace the principles of evidence-based medicine (EBM). Evidence-based medicine incorporates the best results from clinical and epidemiological research with individual clinical experience and expertise whilst taking account of patient preferences.56,57
In manual medicine the focus of critical review of the efficacy of treatment can often be based solely upon research evidence. However clinical experience and patient preferences should also play an important role in deciding the best treatment approach. Practice-based evidence (PBE) is evidence that individual clinicians acquire through clinical experience and practice, which should be informed by research. Best practice should also take account of convention, clinical experience, and patient preference (Fig. 6.1).
Evidence for efficacy of interventions, such as spinal manipulation, can be assessed according to a hierarchy of evidence that exists in the literature for that intervention.
Hierarchy of evidence
• Randomized controlled trials (RCTs)
• Non-randomized controlled trials
• Cohort or longitudinal studies
• Cross-sectional descriptions and surveys
• Case series and case reports
Syntheses
Bronfort et al58 report that since 1979 there have been in excess of 50 mostly qualitative, non-systematic reviews published relating to manipulation and mobilization treatment for back and neck pain. A number of systematic reviews and meta-analyses have also been undertaken that attempt to determine the efficacy of spinal manipulation on low back pain,59–69 back and neck pain,70,71 neck pain72–76 and chronic headache.77
Bronfort et al71 undertook an extensive search of computerized and bibliographic literature databases up to the end of 2002 relating to the efficacy of spinal manipulation and mobilization for low back and neck pain and concluded that the use of spinal manipulative therapy and / or mobilization is a viable option for the treatment of both low back pain and neck pain. This systematic review identified the paucity of high-quality trials distinguishing between acute and chronic presentations and recommended that further research should examine the value of spinal manipulation and mobilization for well-defined sub-groups of patients and determine the cost-effectiveness of different treatment approaches.
A Cochrane database systematic review on spinal manipulative therapy for low back pain concluded that there is no evidence that spinal manipulation is superior to other standard treatments for patients suffering acute or chronic low back pain.67 A systematic review of RCTs published since 1995, relating to a range of complementary therapies for non-specific back pain, concluded that spinal manipulation has real but modest benefits for acute and chronic low back pain and that the risks of lumbar manipulation are low.64 A systematic review relating to chronic low back pain concluded that both spinal manipulation and mobilization are viable treatment options and are at least as effective as other commonly used interventions with a low risk of serious adverse events.69 Waddell, on reviewing the evidence in relation to acute low back pain and disability, commented that there are numerous symptomatic treatment options other than manipulation but there is little scientific evidence that they are effective and states that the evidence supports the use of manipulation as a treatment option for symptomatic relief.78 The United Kingdom Back Pain Exercise and Manipulation (UK BEAM) randomized trial concluded that spinal manipulation over a 12-week period produced statistically significant benefits relative to best care in general practice at both 3 and 12 months79 and that spinal manipulation was also a cost-effective addition to general practice best care.80 The joint clinical practice guideline from the American College of Physicians and the American Pain Society states that practitioners should consider using spinal manipulation for acute, sub-acute or chronic low back pain in those patients who do not improve with self care options.81
A Cochrane review of manipulation and mobilization for mechanical neck pain concluded that, when combined with exercise, mobilization and / or manipulation is beneficial for persistent mechanical neck disorders with or without headache, providing strong evidence for using a multi-modal treatment approach.74 Vernon et al75 carried out a systematic analysis of group change scores in RCTs of patients treated with manual therapy suffering from chronic neck pain not due to whiplash and excluding headache or arm pain. They concluded that patients randomized to receive spinal manipulation or mobilization showed clinically important improvements at 6, 12 and up to 104 weeks after treatment. The Bone and Joint Decade 2000–2010 task force on neck pain and its associated disorders reported that the evidence favours supervised exercise sessions with or without manual therapy over usual or no care for both whiplash-associated disorders and neck disorders without trauma.76 The task force reported that manipulation and mobilization yielded comparable clinical outcomes.
A systematic review of the efficacy of spinal manipulation for chronic headache concluded that spinal manipulative therapy has an effect comparable to commonly prescribed prophylactic tension headache and migraine medications.77
In an effort to increase consistency in the management of spinal disorders the available evidence has been reviewed by expert committees to establish clinical guidelines. Clinical guidelines for the management of low back pain have been developed in at least 12 different countries. Since the available evidence is international there would be an expectation that all the guidelines regarding diagnosis and treatment would offer broadly similar recommendations.81 Willem et al66 noted that all national guidelines on the management of low back pain included the use of spinal manipulation. However, the data upon which national recommendations are based has been interpreted differently, leading to conflicting guidelines between countries for the use of spinal manipulation in the management of both acute and chronic back pain.
Manual therapy approaches, including HVLA thrust techniques, have been negatively impacted by poorly designed and implemented research studies. Practitioners of manipulative therapy are not a homogeneous group and have differing levels of training and skill in the application of manipulative techniques. Patients with spinal pain are also not a homogeneous group, which makes comparison of like with like extremely difficult. However, practitioners have demonstrated an ability, using signs and symptoms, to identify sub-groups of patients with low back pain and then match them to specific treatment approaches. Those patients matched by the practitioner to specific interventions showed statistically significant improvement compared with non-matched controls.82 Several classification systems for spinal and pelvic girdle pain have been proposed in an attempt to address this problem and identify the sub-groups of patients who are likely to respond positively to specific interventions.83–90
Research into the predictive value of specific clinical findings to identify patients with spinal pain who are likely to benefit from spinal manipulation has led to the development of clinical prediction rules. Clinical prediction rules consist of combinations of variables obtained from self-report measures, patient history and examination that assist in identifying those patients with spinal pain most likely to respond to spinal manipulation.25–28
Clinical Decision Making
Clinical decision making is the ability to collate and synthesize information, make decisions and appropriately implement these decisions in the clinical environment. At our present state of knowledge, what should guide our clinical decision making to incorporate HVLA thrust techniques within a treatment regimen? All healthcare practitioners utilize a clinical decision-making process prior to the application of a therapeutic intervention, such as HVLA thrust technique (Box 6.2).
Box 6.2 Clinical decision making
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree