, Paul D. Siney1 and Patricia A. Fleming1
(1)
The John Charnley Research Institute Wrightington Hospital, Wigan, Lancashire, UK
Detailed documentation forms an integral part of pre-operative assessment. Unfortunately this aspect is not often brought up as part of the more general teaching or practical management of a patient’s problem, unless it presents an unusual appearance or a diagnostic riddle. Any method of assessment or documentation must not be so detailed as to be time consuming, or so vague as to be of little value.
Radiographic assessment needs to be made in two parts: The underlying hip pathology and the radiographic appearance of the arthritic hip. The first will give some indication of the underlying general problems, the second the radiographic appearances as this may have a bearing on the technique of hip replacement. The classification originally proposed by Charnley serves well and requires minimum of time yet offers essential basic information (Fig. 6.1).
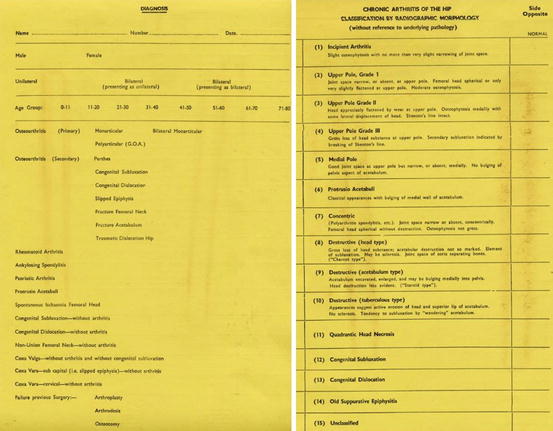
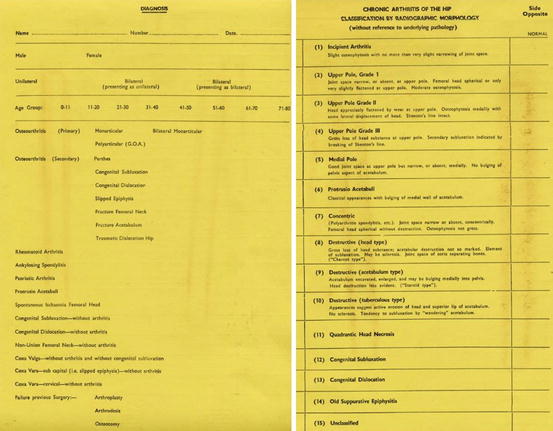
Fig. 6.1
Yellow radiographic assessment chart noting the underlying hip pathology and the radiographic appearance of the arthritic hip
Osteoarthritis: | |
Primary | Mono and bi-articular |
Poly-articular (GOA) [generalised osteoarthritis] | |
Secondary | Congenital dysplasia/subluxation/dislocation |
Perthe’s disease | |
Slipped upper femoral epiphysis | |
Trauma | |
Fractured femoral neck | |
Sepsis – acute | |
Sepsis – chronic | |
Quadrantic head necrosis (cause if known or suspected) | |
Rheumatoid arthritis | |
Ankylosing spondylitis | |
Paget’s disease | |
Protrusio acetabuli | |
Unclassified | |
Radiographic Morphology of the Arthritic Hip [1]
Uniformity of terminology and agreement on definitions are an essential part of scientific communication. It allows meaningful comparisons, avoids anecdotal presentations or emotional overtones and contributes to the advancement of our knowledge. In the arthritic hip, where radiographic appearances usually change with time, a statement: “severe arthritis” or “end stage arthritis” – has no meaning; it probably reflects the surgeon’s or the patient’s emotions more accurately.
Drawing lines or diagrams on hard-copy radiographs is best avoided, unless they can be easily removed without damaging the radiograph. Although they may serve a purpose, temporarily, they only attract the attention of the viewer; maybe to the exclusion of more important pathology. Eventually the reason for the lines is forgotten. The possibility of making errors when too much reliance is placed “on the lines drawn on radiographs …and used as a basis for calculation” has been pointed out [2]. With the computer technology used today the problem is no longer relevant.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








