Proximal Tibia Fractures: Locked Plating
James P. Stannard
Indications/Contraindications
The indications for surgical treatment of proximal tibia fractures are somewhat variable and must be individualized for each fracture and patient. The decision for surgery involves an evaluation of the patient, the fracture, and the surgeon. Patient factors include age, activity level, type of employment, associated injuries, and medical co-morbidities. Issues to consider regarding the fracture include pattern, degree of comminution, bone quality, displacement, articular impaction, mechanism of injury, condition of soft tissue around the fracture, and stability of the knee. Surgeon factors that must be considered when deciding whether to treat a fracture surgically include surgeon experience, surgical team experience, and available equipment.
There are three absolute indications for surgical treatment of proximal tibia fractures: open injuries, compartment syndromes, and fractures associated with vascular injuries. Although these are absolute indications for surgery, they are not absolute indications for open reduction and internal fixation (ORIF). In many fractures associated with these three absolute indications for surgery, temporary, spanning, external fixation is the initial treatment of choice (Fig. 27.1). Relative indications for surgical treatment of proximal tibia fractures include most displaced bicondylar and medial condyle tibial-plateau fractures; lateral tibial-plateau fractures that result in knee instability; condylar widening that exceeds 5 mm; fracture dislocations of the knee; nonarticular, proximal, tibia fractures that are displaced or unstable; and any fracture associated with patient or injury factors that will prevent early mobilization of the knee joint if treated nonoperatively (1–5).
After the decision has been made to treat a proximal tibia fracture surgically, the surgeon must decide between conventional osteosynthesis and locked plating. Specific indications for locked plating include bicondylar tibial-plateau fractures, marked comminution, osteopenia or poor bone quality, and a bone gap secondary to loss of bone along one or both columns of the proximal tibia.
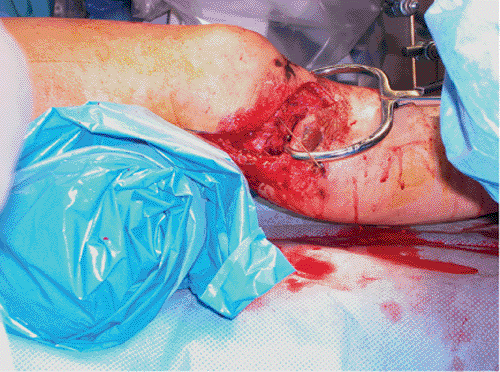
Contraindications for locking plate osteosynthesis of the proximal tibia are identical to those for conventional compression plating of the proximal tibia. The primary contraindication
is a severely damaged soft-tissue envelope (Fig. 27.2) that makes preceding with surgery a dangerous and high-risk proposal. In many cases, soft-tissue and skin damage will be a temporary contraindication for surgery. Delaying surgical treatment for a period of a few days to a few weeks, until optimal soft-tissue conditions exist, minimizes complications (3). Additional contraindications for ORIF include patients with serious medical co-morbidities that make them poor surgical candidates, and stable fractures with minimal displacement. Finally, a contraindication for locked plating is any fracture that can be treated equally well with a conventional compression plate. Plates designed with fixed-angle locking screws are expensive compared to compression plates and should be reserved for fractures that will benefit from locked plating.
is a severely damaged soft-tissue envelope (Fig. 27.2) that makes preceding with surgery a dangerous and high-risk proposal. In many cases, soft-tissue and skin damage will be a temporary contraindication for surgery. Delaying surgical treatment for a period of a few days to a few weeks, until optimal soft-tissue conditions exist, minimizes complications (3). Additional contraindications for ORIF include patients with serious medical co-morbidities that make them poor surgical candidates, and stable fractures with minimal displacement. Finally, a contraindication for locked plating is any fracture that can be treated equally well with a conventional compression plate. Plates designed with fixed-angle locking screws are expensive compared to compression plates and should be reserved for fractures that will benefit from locked plating.
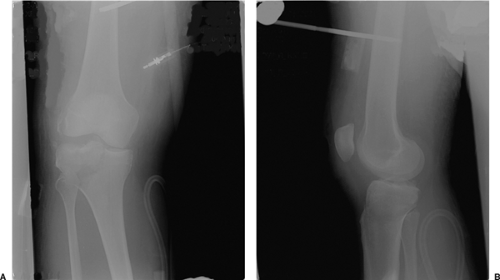 Figure 27.1. A,B. Spanning external fixator placed for temporary stabilization following a tibial plateau fracture. |
Preoperative Planning
The initial step in preoperative planning is a good history and physical examination. One of the crucial steps in developing a treatment plan is determining whether the fracture occurred as a result of high- or low-energy trauma. Locked plating will be used more frequently following high-energy trauma. In cases of proximal tibia fractures that result from high-energy trauma, great care must be taken to assess the skin and soft tissues, the compartments of the leg, the patient’s neurological status, and the vascular supply to the distal leg. Careful evaluation of the skin is important. Deep abrasions, contusions, or small open wounds are important to document and consider when determining the location of surgical incisions. I classify closed fractures according to the system proposed by Tscherne (4), highlighting the importance of the soft-tissue envelope in both closed and open fractures. Proximal tibia fractures following high-energy trauma may be associated with a knee dislocation. The surgeon should assume that the patient may have sustained a fracture dislocation and document carefully the neurological and vascular status as well as the fullness of the compartments.
The second step in preoperative planning involves obtaining appropriate imaging studies. Initial radiographs should include a good quality anteroposterior (AP) and lateral view of the knee and proximal tibia. If the fracture demonstrates substantial distal extension, the same views of the tibia should be obtained. Oblique radiographs may also be helpful. Finally, traction views are helpful to determine the quality of reduction that can be obtained using indirect reduction and ligamentotaxis. I frequently obtain these preoperatively using the fluoroscope prior to beginning the surgical procedure. Computed tomography (CT) scanning is frequently used to allow a detailed analysis of the fracture, including the exact location of any impacted articular segments. Advantages of CT include its relatively low cost and availability at most hospitals and medical centers. A major disadvantage is that CT does not provide information regarding the ligaments, menisci, and other structures of the knee.
Magnetic resonance imaging (MRI) is an additional study that provides valuable information regarding both the skeletal and soft-tissue (ligaments, menisci) injuries around the knee. Numerous studies have been published in the last decade or so that establish the role of MRI with tibial plateau fractures. Yacoubian et al (6) found that obtaining MRI in addition to plain radiographs and CT scanning in 52 patients led to a change in the fracture classification in 21% and in the treatment plan in 23% of cases. Holt et al (7) reported that MRI led to a change in fracture classification in 48% and in the treatment plan in 19% of their patients. They also reported a 48% incidence of previously unrecognized injuries in the knee, including two spontaneously reduced knee dislocations.
The protocol over the past 3 years at my institution include MRI rather than CT for tibial plateau fractures that occur as a result of a high-energy mechanism of injury (Fig. 27.3). We have evaluated 103 patients using MRI following tibial-plateau fractures at our institution. Numerous soft-tissue injuries of the knee have been detected, including 25 medial meniscus tears, 35 lateral meniscus tears, 45 anterior cruciate-ligament tears, 41 posterior cruciate-ligament tears, 16 posteromedial corner or medial collateral-ligament tears, and 46 posterolateral corner (PLC) tears. Seventy-one percent of our patients studied had at least one torn ligament associated with their tibial plateau fracture. Fifty-five percent of our patients had two or more ligaments torn, and 26% had injuries to both the anterior and posterior cruciate ligaments (Fig. 27.4) or a fracture dislocation of the knee. Published data demonstrate that between 48% and 90% of patients with tibial plateau fractures have significant associated soft-tissue injuries of the knee. Our data on 103 patients are similar with an incidence of 71% soft-tissue injuries involving the knee following tibial plateau fracture. As noted, MRI scans frequently lead to a change in the treatment plan for patients following tibial plateau fractures (6–11); therefore, because of the difficulty in accurately diagnosing knee injuries associated with tibial plateau fractures, consideration should be given to obtaining an MRI scan for fractures that result from high-energy trauma.
The final step in preoperative planning is the development of the surgical plan. Complex proximal tibia and tibial plateau fractures can be very challenging. Depending on the experience of the surgeon, it may be wise to write a formal surgical plan. Key factors to consider include the location of surgical incisions as determined by fracture displacement and
the condition of the skin, additional instruments (such as the femoral distractor) needed to assist with reduction, the type of implant to treat the fracture, and whether bone graft or a synthetic substitute will be needed.
the condition of the skin, additional instruments (such as the femoral distractor) needed to assist with reduction, the type of implant to treat the fracture, and whether bone graft or a synthetic substitute will be needed.
Surgery
There are two major types of locked plating systems, each with a unique surgical technique. Each system has its benefits and liabilities, and the surgeon must understand the differences and employ the locked plate that is most suited for the individual fracture.
Standard Locked Plating with an Open Surgical Approach
Numerous orthopedic implant manufacturers have developed locking plates that combine holes allowing standard screws with holes that accept locking screws. The patient should be placed on a radiolucent operating table in the supine position. A roll of sheets is placed under the knee, flexing it approximately 25 degrees (Fig. 27.5). The most
commonly employed surgical approach is a midline or an extended, lateral, parapatellar approach. The length of the incision will be dictated by the distal extent of the fracture. Great care should be taken in handling the soft tissues to minimize trauma inflicted by the surgeon.
commonly employed surgical approach is a midline or an extended, lateral, parapatellar approach. The length of the incision will be dictated by the distal extent of the fracture. Great care should be taken in handling the soft tissues to minimize trauma inflicted by the surgeon.
 Figure 27.5. Reduction is improved by placing a roll under the distal femur and thus flexing the knee 20 to 30 degrees. |
Following exposure of the fracture, the first step is reduction of the articular surface. The techniques used are identical to those used with conventional ORIF. Impacted fragments must be manually disimpacted, reduced, and stabilized with Kirschner (K) wires initially and screws definitively. It is critical to evaluate the fracture for widening of the articular condyles. If the widening is present, then great care must be taken to reduce them in addition to reducing the articular surface. The use of a large tenaculum or articular clamps can be very helpful in reducing the condyles (Fig. 27.6). We usually use multiple, long, 3.5-mm screws in a subchondral position to stabilize the articular reduction via the rafting technique. Bone grafting using autograft, allograft, or synthetics may be necessary after any impacted fragments have been elevated.
Following successful reduction and stabilization of the articular portion of the fracture, the locking plate is applied to the tibia. Most of these plates are designed to be applied to the lateral side of the tibia. If the fracture pattern requires a medial-based plate, a plate designed for lateral application on the left tibia will often fit surprisingly well on the medial side of the right tibia. The plate is pinned or clamped to the bone and then affixed to the proximal segment. Both conventional nonlocking screws and locking screws can be used.
Some basic rules for application of these plates are listed in Table 27.1. The surgeon should be familiar with these rules prior to attempting osteosynthesis with a locked plating system. Conventional screws can be used to reduce the proximal fragment to the plate as well as to lag fragments together (such as a butterfly does) proximally. After initial




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree