Proximal Humeral Fractures: Open Reduction Internal Fixation
Andrew H. Schmidt
Indications/Contraindications
Proximal humeral fractures represent up to 5% of all fractures and occur most often as the result of a simple fall in an older patient with osteoporosis. The proximal humerus may also be fractured in younger patients as the result of high-energy trauma, and evaluation and management of associated injuries to the head, spine, chest, or other vital areas may take precedence over the shoulder fracture.
Even among experts, controversy exists regarding the indications for surgical versus nonoperative management of many proximal humeral fractures. Furthermore, differences of opinion abound regarding whether internal fixation or arthroplasty provide better outcomes in selected fracture patterns. With the introduction of peri-articular locked plates in the past decade, the treatment of proximal humeral fractures has undergone a profound change.
The overriding goal in the treatment of proximal humeral fractures is the institution of early range of motion. Shoulder function depends on the complex interaction of the glenohumeral and scapulothoracic motion, as well as the interplay of 7 or more muscle-tendon units. Soft-tissue scarring or loss of the gliding surfaces can leave the shoulder stiff and painful and results in poor outcomes. If a fracture of the proximal humerus is either unacceptably displaced or too unstable to allow early motion, then operative intervention should be considered to restore anatomy and useful shoulder function. Whether surgery is done by open reduction and fixation of the fracture or by prosthetic replacement depends on the patient’s needs and expectations, fracture pattern, bone quality, available implants, and the experience of the surgeon.
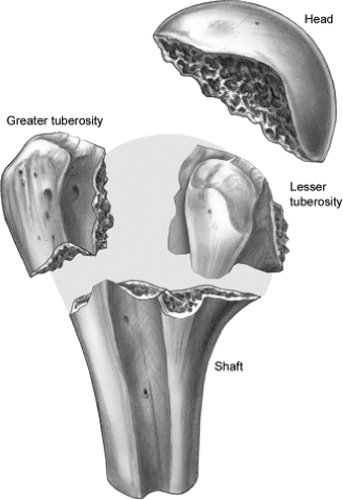
The complex anatomy of the shoulder girdle must be understood to treat proximal humeral fractures successfully. Fractures of the proximal humerus occur in typical patterns that are influenced by muscular insertions that cause predictable displacement of the fracture fragments (Fig. 3.1). Although the Neer classification is often used for surgical decision making, multiple authors have shown that interobserver and intraobserver interpretations of plain radiographs vary widely. Fractures of the proximal humerus can involve the surgical neck and/or the tuberosities. Also, fracture displacement affects the biomechanical function of the
shoulder and the vascularity of the fracture fragments. The inherent stability of the fracture is another factor affecting decision making. A fracture is considered stable if displacement is minimal and the patient will tolerate early functional motion. These fractures are usually treated nonoperatively. Surgery is indicated when fracture instability prevents early motion or when fracture displacement is sufficiently great that functional impairment is likely.
shoulder and the vascularity of the fracture fragments. The inherent stability of the fracture is another factor affecting decision making. A fracture is considered stable if displacement is minimal and the patient will tolerate early functional motion. These fractures are usually treated nonoperatively. Surgery is indicated when fracture instability prevents early motion or when fracture displacement is sufficiently great that functional impairment is likely.
Isolated greater-tuberosity fractures are often associated with anterior shoulder dislocation, and displaced tuberosity fragments should be reduced and fixed. Tension-band techniques with heavy suture or wire can be utilized, or screw fixation may be considered when comminution is minimal and bone quality is good. Isolated lesser-tuberosity fractures are uncommon and may occur with posterior shoulder dislocations. Large lesser-tuberosity fragments may require open reduction and fixation if they are significantly displaced.
Fractures through the surgical neck of the humerus can be nondisplaced or displaced, simple or comminuted. Displaced surgical-neck fractures in physiologically young patients should be treated by reduction and fixation. A number of fixation techniques have been employed, including T-plate fixation, percutaneous pinning, tension-band wiring, and intramedullary nailing. With the advent of peri-articular locking plates, these methods of treatment have been rendered obsolete (Fig. 3.2). Locked plates dramatically increase angular stability, minimize screw toggle, and allow early range of motion in the shoulder. Therefore, locking plates are indicated for nearly every fracture of the proximal humerus for which surgical treatment is necessary.
Many fractures of the proximal humerus consist of various combinations of elementary fracture patterns. Three-part fractures generally represent the combination of surgical neck and greater-tuberosity fractures (Fig. 3.3). For these injuries, treatment should be based on the radiographic or computed tomography (CT) interpretation of the fracture, such as tuberosity or humeral-head displacement. Locking plates are ideal implants for these
fractures because they provide stable fixation of the humeral head and a means to repair the greater or lesser tuberosities.
fractures because they provide stable fixation of the humeral head and a means to repair the greater or lesser tuberosities.
Several surgeons have reported successful results with open reduction and internal fixation for four-part fractures, and this treatment should be considered in relatively active, young patients. It is interesting that complications after operative repair of valgus-impacted four-part fractures seem to be less frequent than in other types of four-part fractures, and therefore, these valgus-impacted injuries may be a good indication for internal fixation. When a valgus-impacted fracture is identified, one must carefully look for evidence of lateral displacement of the humeral-head fragment (Fig. 3.4). If lateral displacement is found, the medial periosteal vessels that perfuse the articular segment may be ruptured, and avascular necrosis is more likely to result. In the absence of lateral displacement of the humeral-head fragment, the humeral head is likely to remain viable.
Preoperative Planning
Appropriate management of proximal humeral fractures begins with a thorough assessment of the functional needs and abilities of the patient, the presence of cognitive or physical impairments, the fracture pattern, bone density, the patient’s expectations, and the ability of the patient to comply with a rehabilitation program. The goal of treatment is to
obtain fracture union and maintain adequate function of the shoulder while avoiding complications. The skills of the surgeon and the resources available must also be considered.
obtain fracture union and maintain adequate function of the shoulder while avoiding complications. The skills of the surgeon and the resources available must also be considered.
In patients who require surgery, a thorough understanding of the fracture geometry and morphology is essential. Precise anteroposterior (AP) and axillary lateral radiographs of the shoulder should be scrutinized. Occasionally, oblique, Y views or arch views of the scapula can be helpful. If any doubt exists, a CT or magnetic resonance imaging (MRI) scan should be obtained in noncritically ill patients. In young patients with wide tuberosity displacement, an MRI scan often provides useful information about the rotator cuff. The fracture displacement should be carefully analyzed, so that reduction maneuvers can be planned. For example, in a valgus-impacted fracture, the greater tuberosity is displaced and the humeral head falls into the resultant void. In addition, an intact, medial, soft-tissue attachment
is often found between the humeral head and shaft. Therefore, a valgus-impacted fracture is reduced by applying a medial force to the superior-lateral aspect of the humeral head and using the medial soft tissues as a hinge (Fig. 3.5). Once the humeral head is reduced, the greater tuberosity may be reduced into its bed, after which it serves to maintain reduction of the humeral head. In contrast, a humeral head that is displaced in varus will require the opposite maneuver to reduce the articular segment.
is often found between the humeral head and shaft. Therefore, a valgus-impacted fracture is reduced by applying a medial force to the superior-lateral aspect of the humeral head and using the medial soft tissues as a hinge (Fig. 3.5). Once the humeral head is reduced, the greater tuberosity may be reduced into its bed, after which it serves to maintain reduction of the humeral head. In contrast, a humeral head that is displaced in varus will require the opposite maneuver to reduce the articular segment.
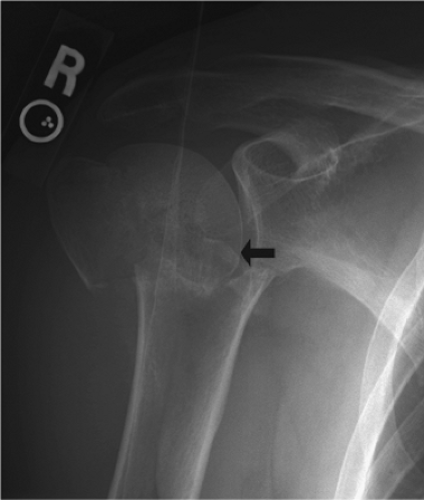 Figure 3.4. A valgus-impacted fracture with more than 5 mm of lateral displacement of the humeral head. This may signify disruption of all soft-tissue attachments to the articular segment. |
Open-reduction internal fixation of the proximal humerus is usually done through a classic deltopectoral approach. Although a deltoid-splitting approach is normally used for isolated greater-tuberosity fractures, the classic and splitting techniques may be combined if the greater tuberosity is displaced posteriorly such that reduction and fixation is difficult via the deltopectoral approach alone. This two-incision approach may also be helpful in patients with a large muscle envelope or significant soft-tissue swelling.
Surgery
General Considerations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree