Proximal Humeral Fractures: Arthroplasty
Louis U. Bigliani
Sean F. Bak
Steven S. Goldberg
Indications/Contraindications
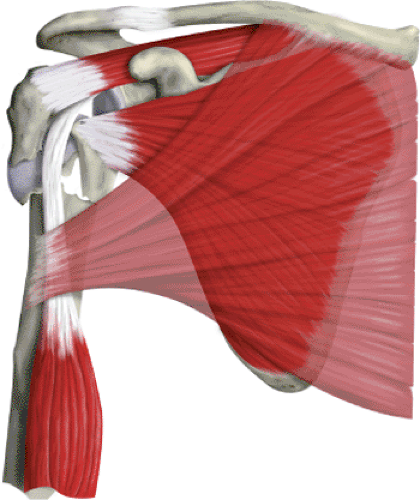
Proximal humeral replacement is a useful surgical technique for acute displaced fractures of the proximal humerus (Fig. 4.1). The indications for placement of a prosthesis are (a) 4-part fractures and fracture dislocations, (b) head-splitting fractures, (c) impression fractures involving more than 40% of the articular surface, and (d) selected 3-part fractures in older patients with osteoporotic bone. The majority of severely displaced, proximal, humeral fractures occur in the older population, with predominance in women. Other methods of treatment, including closed reduction, open reduction-internal fixation, head excision, and fusion, have been reported to have a high percentage of unsatisfactory results.
The contraindications for proximal humeral replacement are active soft-tissue infection, chronic osteomyelitis, and paralysis of the rotator-cuff muscles. Deltoid paralysis is not a contraindication: Adequate yet compromised function can be achieved in such a shoulder.
Preoperative Planning
A detailed history and physical are essential, although an adequate clinical evaluation of the injured limb may be difficult because of pain and swelling. It is important to establish whether the patient has lost consciousness or has had a seizure. Neurovascular status should be assessed with a high index of suspicion for injuries to the axillary nerve and artery. Injuries to the axillary artery are limb threatening and should be evaluated with emergency arteriography and a vascular surgery consultation. Injuries to the brachial plexus or peripheral nerves are often overlooked initially. The vast majority of these are treated conservatively. Electromyographic analysis should be planned 3 to 4 weeks after injury to help clarify the extent of the injury. A neurologic deficiency should not delay definitive management of the fracture. Most injuries are neurapraxias and will resolve over time sufficiently to allow adequate function. If the neurologic status does not improve, any needed procedure to the axillary nerve can be done within 3 months of injury without compromise.
To determine whether a humeral head replacement is the best treatment option for a displaced, proximal, humeral fracture, the fracture pattern must be clearly delineated. In the majority of cases, this can be achieved with a trauma series (Fig. 4.2). This includes a true anteroposterior (AP) view of the scapula (taken 30 to 40 degrees oblique to the coronal plane of the body), a transscapular lateral or Y view, and an axillary view. The axillary view is taken by abducting the arm 20 to 30 degrees and placing the tube in the axilla with the radiographic plate above the shoulder; there is no need to abduct the arm fully. Often the surgeon must position the arm because of pain. Alternately, a Velpeau axillary view can be obtained, with the patient remaining in the sling and leaning back over the plate and the tube directed downward. If displacement cannot be determined, or if the articular surfaces of the humeral head or glenoid are not clearly visualized, then a computed tomography (CT) scan also may be used to clarify the situation. Use of a preoperative scanogram of both the involved and the uninvolved arm often helps establish the proper length of the prosthesis relative to the remaining humeral shaft.
Surgery
Patient Positioning
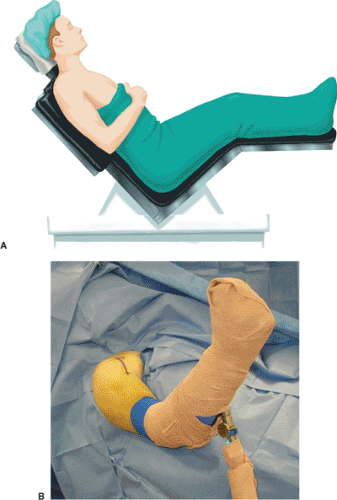
Proper patient positioning is the first step to a successful procedure, and its importance cannot be overemphasized. The goal is to have global access to the shoulder. This is achieved by having the involved shoulder elevated from the table and properly supported. We prefer a table with a cutaway section at the shoulder that allows greater access posteriorly and has an attached pneumatic arm positioner (Spider, Tenet Medical, Calgary,
Alberta, Canada) (Fig. 4.3). Our anesthetic of choice is an interscalene regional block because it provides excellent muscle relaxation, which facilitates exposure. Two small towels are placed under the medial border of the scapula to negate any retraction. The head is secured in a positioner in neutral rotation and flexion with respect to the cervical spine. The operating table should then be placed in a modified beach-chair position. The patient is first flexed fully at the hips, and the foot of the table is lowered to slightly flex the knees. The back of the operating table is then elevated so that the patient sits up at an angle of approximately 45 to 50 degrees. Surgical drapes are used to isolate the operative field superiorly to the midclavicle and inferiorly below the axilla so that the arm can be draped free and is able to be moved throughout the surgery.
Alberta, Canada) (Fig. 4.3). Our anesthetic of choice is an interscalene regional block because it provides excellent muscle relaxation, which facilitates exposure. Two small towels are placed under the medial border of the scapula to negate any retraction. The head is secured in a positioner in neutral rotation and flexion with respect to the cervical spine. The operating table should then be placed in a modified beach-chair position. The patient is first flexed fully at the hips, and the foot of the table is lowered to slightly flex the knees. The back of the operating table is then elevated so that the patient sits up at an angle of approximately 45 to 50 degrees. Surgical drapes are used to isolate the operative field superiorly to the midclavicle and inferiorly below the axilla so that the arm can be draped free and is able to be moved throughout the surgery.
Technique
Approach
A long deltopectoral approach is performed, starting just below the clavicle and extending over the lateral aspect of the coracoid to the deltoid insertion on the humeral shaft (Fig. 4.4). Large Gelpi retractors can be placed in the skin to provide exposure. The cephalic vein is identified in the deltopectoral interval and is usually retracted laterally. There are fewer tributary veins on the medial side than on the lateral side, so retracting the vein laterally decreases bleeding. Often, however, there is a large crossover vein superiorly, which should be cauterized so that superior exposure is not compromised. It is important to preserve the deltoid origin
on the clavicle and acromion. Rarely is the deltoid origin removed. If more exposure is needed, the deltoid insertion may be partially elevated; however, the proximal third of the pectoralis insertion is usually detached from its humeral attachment (Fig. 4.5). This should be tagged with a suture and reattached during closure. At this stage, the coracoid and coracoid muscles should be identified. The coracoid is the lighthouse to the shoulder, and dissection should not be medial to this structure (Fig. 4.6). A
broad retractor is placed beneath the lateral borders of the coracoid muscles. The coracoid muscles should not be cut nor the coracoid process osteotomized because they provide a barrier to protect the neurovascular bundle. The anterior portion of the leading edge of the coracoacromial ligament can be resected to facilitate exposure. The bulk of this ligament should remain intact to avoid any compromise in superior stability. Another retractor is placed underneath the deltoid and the muscle is retracted laterally. The long head of the biceps should be identified distally and followed proximally, as this is an important structure that will lead to the center of the shoulder at its glenoid insertion (Fig. 4.7).
on the clavicle and acromion. Rarely is the deltoid origin removed. If more exposure is needed, the deltoid insertion may be partially elevated; however, the proximal third of the pectoralis insertion is usually detached from its humeral attachment (Fig. 4.5). This should be tagged with a suture and reattached during closure. At this stage, the coracoid and coracoid muscles should be identified. The coracoid is the lighthouse to the shoulder, and dissection should not be medial to this structure (Fig. 4.6). A
broad retractor is placed beneath the lateral borders of the coracoid muscles. The coracoid muscles should not be cut nor the coracoid process osteotomized because they provide a barrier to protect the neurovascular bundle. The anterior portion of the leading edge of the coracoacromial ligament can be resected to facilitate exposure. The bulk of this ligament should remain intact to avoid any compromise in superior stability. Another retractor is placed underneath the deltoid and the muscle is retracted laterally. The long head of the biceps should be identified distally and followed proximally, as this is an important structure that will lead to the center of the shoulder at its glenoid insertion (Fig. 4.7).
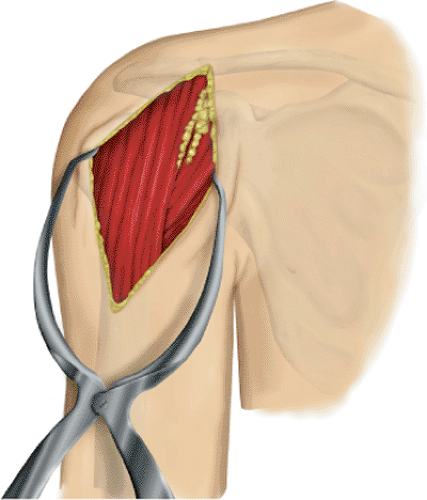 Figure 4.4. A long deltopectoral approach starts just below the clavicle and extends over the lateral aspect of the coracoid to the deltoid insertion on the humeral shaft. |
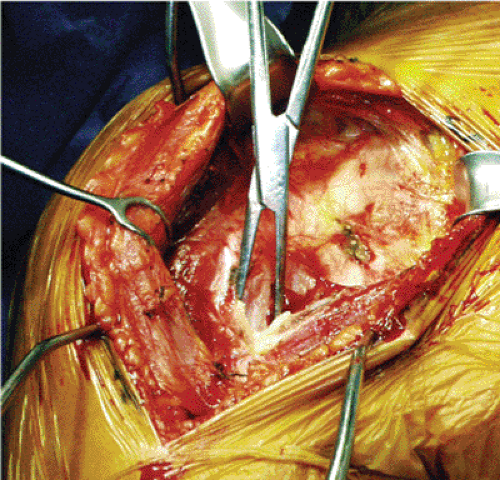 Figure 4.5. The superior insertion of the pectoralis major is usually detached and tagged to allow improved exposure. |
Exposure of the Fracture
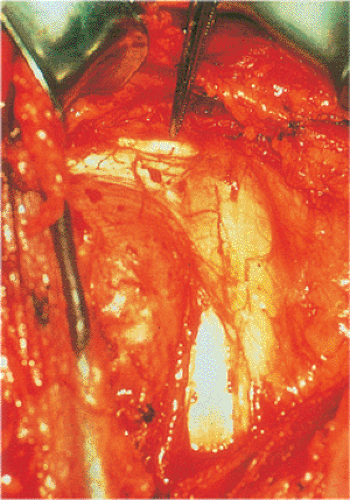
Once the retractors have been placed in the appropriate position, hemorrhagic bursa and fracture hematoma can be identified and gently removed.
It is important not to remove large pieces of bone that may be used later to support the prosthesis on the deficient proximal shaft. The key to recognizing the various components of the fracture is the long head of the biceps. As the biceps is followed proximally, the lesser tuberosity is on the medial side, and the greater tuberosity is usually on the lateral side (see Fig. 4.1).
It is important not to remove large pieces of bone that may be used later to support the prosthesis on the deficient proximal shaft. The key to recognizing the various components of the fracture is the long head of the biceps. As the biceps is followed proximally, the lesser tuberosity is on the medial side, and the greater tuberosity is usually on the lateral side (see Fig. 4.1).
As a rule, the rotator interval can be split in the area of the bicipital groove, as this is often fractured. This split can be carried proximally to help identify and mobilize the supraspinatus and subscapularis because they attach to the greater and lesser tuberosities, respectively. The interval is repaired later. The head usually lies between the tuberosities and is removed and used for sizing of the prosthetic head (Fig. 4.8).
If the head has been dislocated laterally, the greater and lesser tuberosities act almost as a hood and can be elevated intact. In this situation, the head can be extracted and the prosthesis can be placed without disturbing the rotator interval, greater-tuberosity, or lesser-tuberosity fragments. Generally, however, the interval must be opened in the area of the bicipital groove. Once again, it is important to preserve any loose fragments and pieces of bone to be used later in the procedure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree