Proximal Femoral Replacement
Rajit Chakravarty
Mohammad R. Rasouli
Javad Parvizi
CASE
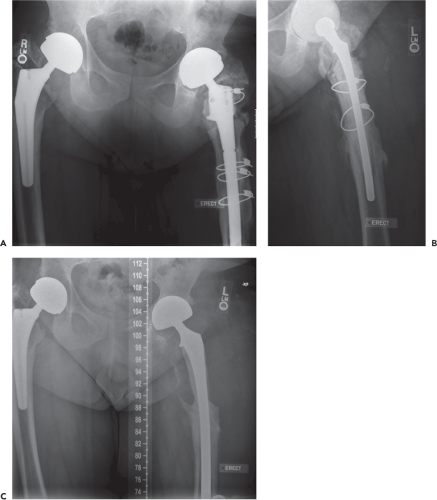
A 46-year-old male with body mass index of 38.3 kg/m2 and past medical history of Perthes disease requiring bilateral total hip arthroplasty (THA) at the age of 29 years. He has undergone multiple prior revisions and presented with a chronically infected THA with cultures positive for Enterobacter and extensive proximal bone loss (Fig. 123.1A). The patient underwent a resection arthroplasty and insertion of a cement spacer as the first stage of a proposed two-stage exchange (Fig. 123.1B). Two months following the resection arthroplasty, his ESR and CRP levels were elevated (42 mm/hr and 69.5 mg/dL, respectively) and the spacer was exchanged and additional debridement was performed (Fig. 123.1C). At that time operative cultures showed growth of Candida species and antifungal medication was added to his antibiotic regimen.
Introduction
Total hip arthroplasty (THA) is considered one of the most successful and reliable surgical procedures within orthopedics. As the number of patients undergoing THAs continues to rise, so too does the need for revision total hip replacement (1). Revision THA with femoral bone loss adds complexity to the procedure and poses a technical challenge to the surgeon (2,3,4,5). The operating physician must not only accurately assess the extent of proximal femoral bone loss, but also choose the appropriate prosthesis. Factors contributing to loss of femoral bone stock include stress shielding with adaptive remodeling, osteolysis secondary to particulate debris, prior infection, periprosthetic fractures, natural aging process, and diminished bone mass secondary to multiple previous reconstructive hip procedures (2,6,7,8,9,10,11).
While technically difficult to treat, there are several reconstructive options available for addressing severe femoral bone loss in revision THA. These choices include long cemented or press-fit stems, impaction allografting, resection arthroplasty, allograft prosthetic replacement and modular proximal femur replacement (3,4,12,13,14,15,16).
Historically, proximal femoral replacement with megaprosthesis was initially employed for reconstruction following tumor resection (5). The first-generation monolithic megaprosthesis included variable segmental stems which were cemented into the femoral diaphysis (Fig. 123.2). Newer generation of megaprosthesis allows for various resection lengths through its modular design and promote bony ingrowth via porous coating and extracortical bone bridging (Fig. 123.3). In addition, the second-generation modular prosthetic components with proximal holes afford better soft tissue reattachment and the ability to reapproximate the retained host bone to the femoral component.
Indications
After initial success of the megaprosthesis in treating patients with neoplastic conditions, it soon became part of the armamentarium of the reconstructive hip surgeon in addressing extensive proximal femoral bone loss. Proximal femur replacement arthroplasty is currently reserved for the elderly and sedentary patient with massive proximal femoral bone loss following multiple prior revisions, periprosthetic joint infection, periprosthetic fracture, fracture nonunion, and hip salvage after failed resection arthroplasty (2,3,4,5,17). One paramount prerequisite for the use of proximal femoral replacement is the presence of sufficient distal femoral length to secure the femoral stem distally.
Contraindication
While indicated for reasons mentioned previously, there are instances which would preclude the use of proximal femoral replacement. The presence of superficial or deep infection around the hip is considered an absolute contraindication. In addition, patients with significant medical comorbidities, severe vascular insufficiency that place wound healing at risk or inadequate distal femoral bone stock for the insertion of the femoral component also serve as contraindications (2).
Preoperative Planning
Proximal femoral replacement is technically demanding and requires meticulous attention to detail to achieve success. Thus the importance of preoperative planning cannot be
overstated. Standing radiographic studies along with serologic tests need to be obtained prior to any revision THA. Hip aspirations may be performed if a high index of suspicion of deep infection exists or if serologic markers are elevated.
overstated. Standing radiographic studies along with serologic tests need to be obtained prior to any revision THA. Hip aspirations may be performed if a high index of suspicion of deep infection exists or if serologic markers are elevated.
Determining proximal femoral arthroplasty as the indicated implant is based on a thorough assessment of the preoperative x-rays. Proximal femur reconstruction is performed for metaphyseal–diaphyseal lesions that extend below the lesser trochanter, cause extensive cortical destruction, and yet spare at least 3 cm of distal femoral diaphysis for secure fixation of the femoral stem (18). Some advocate using the Paprosky femoral deficiency classification and algorithmic approach to reconstruction in revision THA. Della Valle and Paprosky (12) recommended the use of proximal femoral replacement in the setting of a type IV femur in the elderly with extensive metaphyseal and diaphyseal damage in conjunction with widened femoral canal. Proximal femoral replacement also has a role in addressing Vancouver type B3 periprosthetic fracture with its association of loose stem and poor proximal bone stock in the less active patients (3,17,19). In addition, proximal femoral
replacement arthroplasty has shown to be a viable form of hip salvage in patients with severe lack of proximal femoral bony structure due to failed THA or infection that preclude the use of long stem or calcar supporting type of implant in revision THA (2,3,5).
replacement arthroplasty has shown to be a viable form of hip salvage in patients with severe lack of proximal femoral bony structure due to failed THA or infection that preclude the use of long stem or calcar supporting type of implant in revision THA (2,3,5).
 Figure 123.2. Example of first-generation monolithic proximal femoral replacement prosthesis in various sizes. (Reprinted with permission from Sim FH, Chao EYS. Hip salvage by proximal femoral replacement. J Bone Joint Surg Am. 1981;63:1228–1239.) |