Chapter 7.11 Prolotherapy Prolotherapy is an injection therapy used to treat chronic ligament, joint, capsule, fascial, and tendinous injuries. The goal of this treatment is to stimulate proliferation of collagen at the fibro-osseous junctions to promote nonsurgical soft tissue repair and to relieve pain (see Fig 7.11.1) (Klein & Eck 1997). Originally defined by Hackett as “the rehabilitation of an incompetent structure (ligament or tendon) by the generation of new cellular tissue”, it has received a variety of names (Dagenais et al. 2005; Alderman 2007). Growth factors are powerful polypeptides that induce wide-ranging effects including cell migration, proliferation, and protein synthesis. These proteins may be produced by the affected cells or in other cells. These growth factors must avoid the binding proteins which could cause their inactivation, find their way to the area needing growth, and hook onto an appropriate receptor protein (Reeves 2000). Prolotherapy has been used extensively in the USA since the 1930s (over 450 000 people have undergone prolotherapy treatment) and in other countries around the world. Yet it has not become a mainstream therapy (Mooney 2003). The abundance of case series studies and anecdotal evidence has not been supported by a large body of randomized controlled trials (Yelland et al. 2003; Dagenais et al. 2007). Hippocrates (trans by Francis Adams 1946) (460–370 BCE) was the first to describe the intentional provocation of scar tissue formation by searing the shoulder capsules in the unstable shoulders of javelin throwers in Sparta. Two millennia later, in 1837, Robert Valpeau of Paris described the use of scar formation for the repair of hernias. One hundred years later, Yeomans (1939) extensively reviewed the genealogy of herniology and a variety of vein sclerosis techniques. Gedney (1937) applied these injection techniques to joints, the first being the sacroiliac joint. He maintained the term sclerotherapy, which remained in use until the 1950s. In that same year, Schultz (1937) described, in the Journal of the American Medical Association, a treatment for subluxation of the temporomandibular joint. In the mid 1950s, George Hackett published a number of articles based on his more than 20 years’ experience, culminating in his book Ligament and Tendon Relaxation Treated by Prolotherapy (Hackett 1956), where he claimed an 82% cure rate in a population of 1600 people with back pain(Hackett & Huang 1961). In 1983, Liu confirmed experimentally increases in ligament junction strength and diameter of collagen fibrils. In 1995, prolotherapy was renamed by some as RIT (regenerative injection therapy), or “the injection of growth factor production stimulants to promote regeneration of normal cells and tissue” (Linetsky & Manchikanti 2005; Reeves et al. 2008). An idea of tissue healing and repair is necessary to understand better the effects of prolotherapy. Wound healing and repair of injured tissues follows three stages (inflammation, matrix deposition, and remodeling) in healthy individuals (Hildebrand et al. 2005). Wound healing generally leads to repair, and in many cases allows return to at least partial function of the injured tissue, but not to tissue regeneration. The repair process leads to a loss of function as a result of scar tissue formation. This is an important factor when dealing with connective tissue that functions in a mechanically active environment. The repair of connective tissue by scar formation – ultimately healing by second intention – may restore connective tissue to its pre-injury length, but will not provide adequate (pre-injury) tensile strength in ligaments and tendons (Reeves 2000; Linetsky & Manchikanti 2005). 1. The tissue deposited attempts to bridge the injured area, regardless of the tissue structure it attempts to gap or repair. 2. The changes in the matrix deposited early in the process lead to the organization of deposited matrix that is different from normal tissue. In mechanically active tissues this will result in a severe compromise of the tensile strength of the new tissue formed: scar tissue is not as strong as the original ligamentous tissue. In addition to matrix deposition in the early stage of healing, there is an increase in cellularity and in vascularity (Bray et al. 1996) due to the release of angiogenic factors in the early postinjury stages. Increased vascularity generates the influx of new micro-vessels. Those connective tissues with endogenous microvasculature will heal well, whereas those that are poorly vascularized (e.g., menisci) do not heal well. In the early stages of scar tissue formation there are almost no neural elements, and therefore minimal regulation of fibroblast-like cells or microvasculature. This is a much slower process, which involves not only alterations in the remodeling of the existing matrix but also gene expression, cellularity, vascularity, and innervation (Hildebrand et al. 2005). The material deposited early is reorganized to suit the mechanical demands of the injured tissue. In the case of ligament, the organization of fibrils becomes oriented towards the axis of the ligament, whereas in other tissues such as skin, a more basket-weave arrangement takes place, which provides strength in multiple directions. This process may take months or even years, and the composition of the repaired tissue changes with time, as does the gene expression phenotype. The application of growth factors to stimulate cell proliferation and extracellular matrix synthesis in tendinopathy has been described by Wang and colleagues (2006) and can represent a new look at the mechanism of action of prolotherapy solutions. The transplantation of mesenchymal stem cells into injured tendons has been shown to promote tendon healing in laboratory animal models (Smith & Webbon 2005). The injection of growth factors should produce structural changes in the tissues injected, and these changes result in improved mechanical quality and function. These changes have not been conclusively proven to date, but the possible role of growth factors represents an exciting development pathway. Further systematical study of the topic is required before definite statements can be made. Two types of substance are used in prolotherapy. The first is injection of growth factor-containing substances. Examples of this include injection of blood, and injection of mass-produced recombinant growth factors, PRP and mesenchymal stem cells. The second method is stimulation of growth factor production, in which the injected solution initiates production of growth factors (dextrose, inflammatory agents that initiate an inflammatory cascade to produce growth factors), and plasmid DNA (Reeves 2000). In the classical understanding of the inflammatory reaction theory, there are four types of solutions, grouped according to the suspected mechanism of action (Banks 1991): 1. Osmotic (e.g., hypertonic dextrose) solutions are thought to provoke cell dehydration, with subsequent cell lysis, release of cellular fragments, which in turn attract granulocytes and macrophages. In addition dextrose could cause glycosylation of cellular proteins. 2. Irritants (e.g., phenol) have a phenolic hydroxyl group that is believed to alkylate surface proteins; these either become antigenic or are damaged, and in turn attract granulocytes and macrophages. 3. Chemotactics (e.g., sodium morrhuate) are chemically related to inflammatory mediators such as leukotrienes and prostaglandins, and possibly undergo conversion to these substances to mediate the inflammatory response. 4. Particulate irritants (e.g., pumice flour) are believed to attract macrophages, leading to phagocytosis. Injections of inflammatory proliferant solutions in connective tissues have demonstrated ligament thickening, hypertrophy of the bone–tendon unit and the strengthening of tendon and ligament in animal studies (Hackett 1956; Liu et al. 1983; Ongley et al. 1988). The injection of hyper- or hypo-osmolar dextrose induces cells to proliferate and produce a number of growth factors. RIT was coined to reflect currently prevailing anatomic and pathophysiological trends in nomenclature. It stimulates chemomodulation of collagen by repetitive induction of inflammatory and proliferative stages leading to tissue regeneration and repair, thus increasing tensile strength, elasticity, mass and load-bearing capacity of collagenous connective tissues. This makes RIT a viable treatment for painful chronic enthesopathies, tendinosis, ligament degeneration, and laxity (Linetsky & Manchikanti 2005). In retrospect, we can say that the original concept of prolotherapy solutions triggering the inflammatory cascade was overly simplistic. The mechanism of action is now considered to be multifaceted, and includes any or all of the following components (Klein et al. 1989; Reeves 2000; Yelland et al. 2004; Linetsky & Manchikanti 2005): 1. Cellular and extracellular matrix damage induced by mechanical needle injury stimulates the inflammatory cascade, which in turn governs the release of growth factors. 2. Compression of cells by a relatively large volume of external fluid, as well as cell expansion or constriction due to osmotic properties of the solution injected that stimulates the release of intracellular growth factors. 3. Chemomodulation of collagen through inflammatory, proliferative, regenerative/reparative responses induced by the chemical properties of the solutions injected and mediated by cytokines and multiple growth factors. 4. Chemoneuromodulation of peripheral nociceptors provides stabilization of antidromic, orthodromic, sympathetic and axon reflex transmissions. 5. Modulation of local hemodynamics with changes in intraosseous pressure leads to reduction of pain. Empirical observations suggest that a dextrose/lidocaine combination has a much more prolonged action than lidocaine alone. 6. Temporary repetitive stabilization of painful hypermobile joints, induced by inflammatory response to the solutions injected, that provides a better environment for regeneration and repair of the affected ligaments and tendons. 7. Additional possible mechanisms of action include the disruption of adhesions that have been created by the original inflammatory attempts to heal the injury by the large volume of solutions injected. The relatively large volume of chemically nonirritating solution assumes the role of a space occupying lesion in a relatively tight and slowly equilibrating extracellular compartment of the connective tissue.
Introduction
History
Wound healing, repair and regeneration
The matrix deposition phase
The remodeling phase
Mechanism of action and substances injected
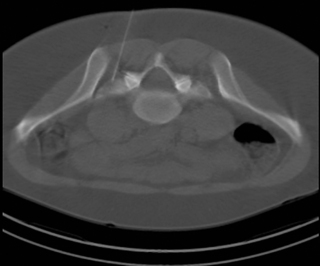
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine