Indications
Contraindications
Older age
Younger age
Anterior knee pain and patellofemoral symptoms
Short, thin patients
Radiographic patellofemoral changes and loss of patellofemoral articular cartilage observed intraoperatively
Well-preserved patellar articular cartilage intraoperatively
Inflammatory arthropathy
Congruent patella tracking well intraoperatively
Obesity
Thin patella incapable of resurfacing
Intraoperative patellar mal-tracking
History of patellar subluxation or dislocation
There are some absolute indications for patellar resurfacing, and these include inflammatory arthritis as well as surgical procedures performed primarily for patellofemoral disease [39].
14.5 Implant Designs
The patellofemoral articulation in a TKA is subjected to considerable compression, shear and torsional loads over long periods of time and is a well-acknowledged source of failure of the entire joint necessitating revision. The Australian Orthopaedic Association National Joint Replacement Registry data indicates higher revision rates in patients who are not resurfaced (7.4 % at 13 years) than those resurfaced (6 % at 13 years) [40]. The patella and femur together act as a unit and influence each other’s mechanics. Whilst the ideal relationship for perfect functioning and longevity remains to be defined, our past experience with asymmetric loading of the tibia as a consequence of mal-alignment suggests that a centrally tracking patellar component will be less likely to wear than a tilted or mal-tracking implant. Over the years, a myriad of patellar components have been designed. They can be broadly classified into as follows.
14.5.1 Metal-Backed Components
These were introduced and became popular during the 1980s mainly due to the perception that a metal backing improved load transfer and protected the fixation interface as well as allowed biological fixation to a porous metal backing [32, 41]. The presence of a metal layer reduced the thickness of the polyethylene, and this subjected it to more contact stresses and deformation [42–44].
14.5.2 All-Polyethylene Components
They can be further divided into:
1.
Dome Shaped
All-polyethylene dome-shaped patellar components are the most common type of patellar implant. The prosthesis is unloaded in extension but is exposed to high compressive forces with knee flexion. Improvements in femoral and trochlear component geometry have reduced this problem.
2.
Modified Dome Shaped
These implants were primarily developed to increase contact area in flexion over what occurs with dome-shaped designs. The implant typically looks like a Mexican sombrero hat. Though studies have shown decreased wear in these designs, it must be borne in mind that the patellar component is subjected to rotation, tilt and sideways moments. Thus, increasing congruity throughout the range of motion may not be the solution to increased wear [45, 46].
3.
Cylindrical
This is a less frequently used design, initially manufactured to increase congruency throughout the range of motion and improving the articulation in the coronal plane without compromising stability. The patellar component is smaller in size ranging from 25 to 30 mm. The implant has a central peg with a collar and can be cemented or un-cemented and implanted with an inlay technique. It has survival rates of over 95 % at 10 years [47].
4.
Anatomically Shaped
These implants closely resemble normal patellar anatomy with a medial and lateral facet to maximise contact area and minimise contact pressures. They were designed to replicate native patellofemoral biomechanics. However, anatomically shaped implants are prone to malpositioning, are difficult to implant and match the femoral component and are therefore seldom used [48–50].
5.
Mobile Bearing
This design system has high conformity and low contact pressure that has contributed to its survival of over 99 % at 12 years. The principle is based on the rotating platform tibial component. Its longevity has been attributed to its ability to move into an appropriate position to minimise load throughout the knee arc of motion irrespective of the surgical alignment [51].
Metal and all-polyethylene patellae may be either cemented or un-cemented.
14.6 Material Science: Ultra-high Molecular Weight Polyethylene (UHMWPE)
UHMWPE is the present material of choice for patellar implants – due to its many suitable material properties but especially its low coefficient of friction when articulating with a chrome cobalt femoral component. Though not the ideal material due to a low yield strength, it remains the best material available at present. UHMWPE is subjected to over 400 % of its yield strength on flexion exceeding 90° subjecting it to deformation [52–55]. Rotating platform designs are subjected to sub-yield strength loads, and with greater conformity comes improved wear resistance [56]. UHMWPE is subjected to plastic deformation due to its yield rather than brittle failure [57]. Anatomic and modified dome-shaped designs are subjected to less wear and creep [58, 59]. Subsurface stress continues even in conforming implants and could lead to permanent deformation [56]. The addition of cross-linked UHMWPE has been shown to reduce wear in tibial polyethylene. The use of cross-linked UHMWPE has increased from 7.1 % in 2003 to 42.9 % in 2013 in the Australian National Joint Registry [40].
14.7 Surgical Technique
14.7.1 Patellar Preparation Positioning and Alignment
Rotation of the femoral component with consequent alteration in the position of the femoral trochlea directly affects one half of the patellofemoral joint. Using an aircraft landing analogy, the trochlea represents the landing strip, and it is imperative to place it where the plane will travel. Correct positioning of the trochlea should be matched with correct positioning of the patella implant to ensure smooth tracking and even distribution of loads across both sides of the prosthesis.
The native patella is conventionally asymmetric with a prominent sagittal plane ridge that divides the articular surfaces into a smaller steeper medial facet and a larger flatter lateral facet. A domed patella implant sited on the medial edge of the native patella with a small area of the lateral facet uncovered will mimic this anatomy.
It is important to resect the patella either parallel to its anterior surface or slightly thicker on the medial side. Commonly, equal amounts of bone resected on both sides can lead to an obliquely aligned patella which is excessively thin medially when viewed from the sunrise position. The most common method of resection is with an oscillating saw – either freehand or with a jig to ensure correct resection is achieved. The authors consider this cut to be the most technically demanding bone cut of TKA and prefer to utilise a milling system with stops as described below under inlay technique. After milling, the patellar component is sited on the medial edge to replicate the native retropatellar eminence and improve tracking. Medialisation by 2 mm reduces peak lateral forces by 10–15 N and creates a medial shear force at flexion <25° which reduces the requirement for lateral release [60].
Maintenance of the joint line is an important consideration in TKA. Raising will produce patella baja which is more common than patella alta, and both adversely affect patellar function [61]. However, it is the author’s opinion that 2–3 mm of altered joint line to achieve a balanced tibiofemoral joint gives a better outcome than a perfectly matched joint line with a significant flexion deformity.
14.7.2 Patellar Thickness
The patella in arthritic patients can be broadly divided into those with a relatively well-preserved articular cartilage including minor wear and those with advanced articular wear and bone stock loss. This latter group frequently has isolated patellofemoral arthritis as a consequence of trochlear dysplasia. The primary aim in replacement of its articular surface is to produce a patella with an overall thickness of 22–24 mm [62]. Larger males may be up to 28–30 mm. A minimum of 15 mm thickness of native patella is usually necessary for resurfacing, but some surgeons use 12 mm as a cutoff [63]. It is important not to remove excessive bone from the patella to compromise the structural integrity. Many have advocated replicating native patella thickness, whilst others suggest reducing the overall thickness by 1–2 mm for efficient tracking and to commence the load-sharing effect of the quadriceps tendon in early knee flexion [64]. Increasing thickness can have catastrophic effects of overstuffing, reduced flexion and increased incidence of fracture [65].
14.7.3 Inlay Versus Onlay Milling Techniques for Patellar Preparation
Onlay milling refers to placement of the patella implant in the desired position on the retropatellar surface by drilling holes for its pegs after milling the entire surface. Of necessity, the patellar capture ring utilised for onlay milling surrounds the patella with its teeth abutting the peripatellar soft tissues. The plane and depth of the mill are determined by the position of the ring which can be difficult to control and frequently alter in position during milling resulting in an oblique surface.
The inlay technique involves placement of the patella into a milled cavity on its retropatellar surface utilising a patellar capture ring which is smaller than the onlay ring with teeth that are anchored to the bone and engineered to resist the clockwise rotation forces imparted to the patella by the reamer blade. Placing the inlay capture ring in a position to achieve the best stability of the reaming system during milling frequently sites the implant too far laterally. The author’s preference is to utilise an inlay milling technique to ensure an accurate plane and depth of cut but remove the outer bony rim with an oscillating saw and rongeurs and then position the implant on the medial patellar margin. Prior to clamping the inlay milling ring on the patella, a small lateral facetectomy is performed with an oscillating saw to deepen the mill laterally and achieve the desired plane of cut.
14.7.4 Lateral Release
The authors assess patellar tracking at the time of trial implantation. It is also a secondary check that tibial and femoral components are in proper rotation. Rarely, mal-tracking persists due to tight lateral structures usually associated with preoperative marked lateral patellar wear. Insall’s “rule of no thumb” can be used to assess if lateral release is required. In this test before closing the wound, the patella should track centrally on flexion of the knee without thumb pressure or the use of one thumb [64, 69]. We also observe that the medial patella sits in apposition with the medial trochlea at 30–40°. Whilst lateral release is routine for many surgeons to improve patellar tracking [69], the authors have found that this is rarely required.
14.7.5 Surgical Technique: Inlay Technique
Whilst the authors prefer to combine the accuracy and stability of an inlay milling technique in patellar resurfacing with the benefits of an onlay technique to correctly position the implant, we describe here how we perform the inlay milling. We resurface all patellae unless too thin.
Soft tissue around the patella is first cleared, and patella thickness is measured using a calliper. Proximal to distal patellar symmetry is evaluated by palpation and flattened where necessary with an oscillating saw which is also utilised to perform a small oblique lateral facetectomy. This deepens the position of the teeth on the lateral side of the inlay capture ring to ensure that the patellar surface is milled close to parallel to the anterior surface or slightly thicker medially. The largest size capture ring that is innately stable is positioned on the patella. Its teeth are designed to resist the clockwise forces imparted to the patella by the mill. The ring is secured to the patella with a clamp that includes variable depth stops to ensure the correct amount of bone remains, and the system may also include a depth stop responding to the amount of bone removed. This will vary depending on the native patella and the implant with the goal of restoring correct patellar thickness for the size of the patient, commonly 22–28 mm. It is important to ensure that the teeth of the capture ring sit down on the patellar surface. The position of the teeth represents the depth of the mill. The ring has a concave cross section when viewed in the sunrise view and is asymmetrical in order to mirror the cross-sectional shape of the patella. This must be borne in mind when the patella is everted medially with a lateral approach for the valgus knee.
The position of the capture ring is determined by its stability against the patella, and this is usually not the ideal position for the implant (Figs. 14.1 and 14.2). Accordingly the authors then remove the remaining rim of the bone with bone nibblers and a saw. Trials are utilised to obtain the largest implant that does not overhang, and it is sited on the medial edge. Holes for the pegs on the patellar component are then drilled, and a trial component is applied and tracking observed. The authors then utilise pulse lavage to prepare the surface and insert all implants.
Fig. 14.1
Patellar resurfacing: Inlay capture ring in black with a concave cross section and sharp teeth that resist clockwise motion and the onlay milling ring with a circular cross section and straight blunt teeth (left) and (right)
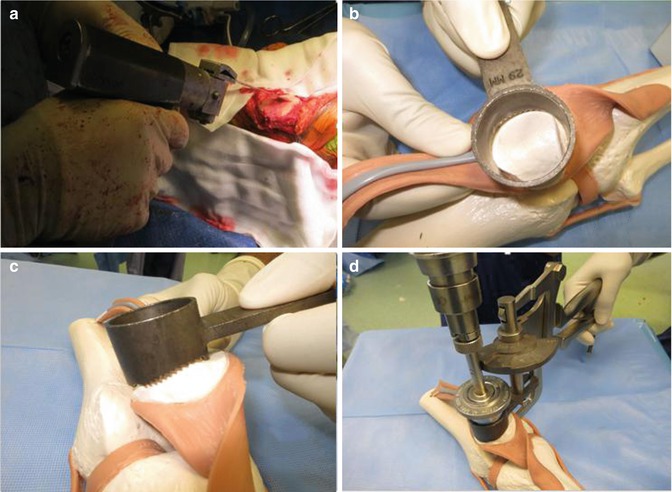
Fig. 14.2
Patellar resurfacing: Lateral facetectomy (a); placement of the milling ring such that it is stable (b); capture ring sitting uniformly over the patella and with sufficient contact (c); milling the patella at the requisite depth (d)
The all-polyethylene patella is cemented and pressurised with a clamp until cement is cured with care to check that the implant is fully seated. Tracking is again checked, and if a lateral release is required, this is accomplished with a pie-crusting technique.
14.7.6 Onlay Technique
The initial steps of measuring as well as clearing soft tissues and osteophytes around the patella are performed as described for the inlay technique. The patella is then held with the capture ring so that its teeth surround the patella completely and uniformly against the soft tissue surrounding it. The thickness to be milled is adjusted on the clamp – usually between 8 and 9 mm depending on the implant. After milling, the capture ring is removed, the remaining thickness is measured and the plane is evaluated using the thumb and index finger to determine if it is uniform. If not uniform, several passes with an oscillating saw over the under-resected area will help. An advantage of milling is that the mill does not deflect off eburnated surfaces in the same way as an oscillating saw.
A disadvantage of the onlay milling technique is the difficulty in holding the patellar capture ring stably in the desired position against the peripatellar soft tissues.
14.8 Complications of Patellar Resurfacing
14.8.1 Patellar Fractures
Fracture of the patella following TKA has an incidence of 0.5–5.2 %. Factors thought to be associated with fracture include increased strain, mal-alignment, thermal necrosis due to bone cement and decreased thickness of the native patella retained [70–73]. Other factors include compromise of patellar vascularity associated with excessive dissection, and lateral release may contribute to this. The incidence of patellar fracture in TKA where the patellar is non-resurfaced is 0.05 %.
Ortiguera and Berry have divided patellar fractures into three groups. In type I, the patellar implant is stable and the extensor mechanism is intact, and this is treated conservatively in a cylinder cast for 6 weeks. With type II, the extensor mechanism is disrupted, and the fracture is treated by tension band wiring and retinacular repair. With type III, the patellar implant is loose, but the extensor mechanism remains intact, and their recommended treatment is removal of the patellar component and reimplantation at a later stage. Type III fractures can be further subdivided into type IIIa, indicating reasonable remaining bone stock, and type IIIb, in which the bone stock is either poor, with an overall thickness of less than 10 mm, or where there is significant patellar comminution [74].
14.8.2 Patellar Loosening
Loosening of the patellar implant is seen much less commonly than the tibia or femur and has an incidence of 0.6–4.8 %. This has reduced since the receding popularity of metal-backed patellae [75, 76]. Obesity, concomitant lateral release, flexion beyond 100°, elevated joint line, small fixation pegs, poor remaining patellar bone stock, osteolysis, osteonecrosis and component mal-alignment are other identified risk factors [72, 77, 78].
14.8.3 Wear
Patellar wear is a consequence of the unfavourable mechanical environment of the patellofemoral articulation. It has reduced considerably after the change to ultra-high molecular weight polyethylene (UHMWPE). The patient’s weight and range of motion affect wear which is seen more commonly in patients with flexion greater than 100°.
14.8.4 Patellar Clunk Syndrome and Impingement
Patellar clunk syndrome is a painful click/clunk and catching sensation of varying severity when the knee is extended [79]. This occurs as a consequence of a prominent fibrous nodule forming between the distal end of the quadriceps tendon and the superior pole of the patella that becomes entrapped in the femoral notch between 30° and 45° of flexion. It is particularly seen in posterior stabilised knees with longer proximal extension of the intercondylar notch. Arthroscopic debridement is usually successful, but recurrence is described. Implant design improvements, particularly extending the trochlear groove distally, have largely eliminated this problem.
14.8.5 Patellar Instability
Patellar instability maybe manifests as patellar mal-tracking, intermittent subluxation or dislocation. Symptoms include poorly localised anterior discomfort, weakness, insecurity, lack of confidence with loading the bent knee, giving way and locking. Patellar instability remains the most common cause of secondary surgery including revision [25, 75, 80]. Factors involved in creating patellar instability include improper patient selection, problems with implant design and technical factors with surgery. Obese patients, those with marked ligamentous laxity and genu valgum, are prone to suffer patellar instability following TKA.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








