CHAPTER 7 Pressure ulcers: impact, etiology, and classification
1. Describe the incidence and prevalence of pressure ulcers in various clinical settings and vulnerable patient populations.
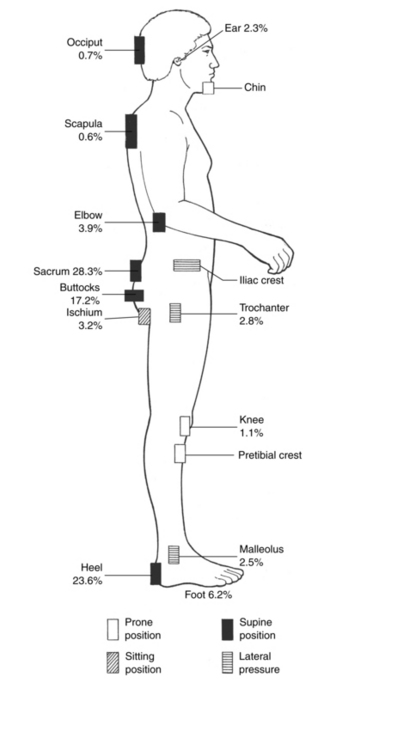
3. Identify the three most common locations at which pressure ulcers develop.
4. Describe the role of subcutaneous tissue and muscle in preventing pressure ulcers.
5. Describe the role of the causative factors for pressure ulcer formation.
6. Differentiate between capillary pressure and capillary closing pressure.
7. Describe the phenomena of reactive hyperemia, blanching erythema, and nonblanching erythema.
8. Describe the pathophysiologic consequences of pressure damage, including the changes that occur at the cellular level and the cone-shaped pressure gradient.
9. List five variables that influence the extent of tissue damage as a consequence of pressure.
Pressure ulcers present a significant health care threat to patients with restricted mobility or chronic disease and to older patients. Because of this threat, more documents about pressure ulcers are being published, such as the International Pressure Ulcer Guidelines for Prevention and Treatment (NPUAP and EPUAP, 2009), the Wound, Ostomy and Continence Nurses (WOCN) Society Guideline for Prevention and Management of Pressure Ulcers (WOCN Society, 2003, 2010), the Registered Nurses Association of Ontario (RNAO) Risk Assessment and Prevention of Pressure Ulcers Guideline (RNAO, 2005), “Guidelines for the prevention of pressure ulcers” by the Wound Healing Society (Stechmiller et al, 2008), the Canadian Association of Wound Care “Best practice recommendations for the prevention and treatment of pressure ulcers: update 2006” (Keast et al, 2007), and Healthy People 2010 (U.S. Department of Health and Human Services, 2000). The Institute for Healthcare Improvement identified pressure ulcers as one of its primary goals in the “Save 5 Million Lives” campaign (Padula et al, 2008). The Cochrane Wounds Group also covers the prevention and treatment of pressure ulcers (Bell-Syer et al, 2007).
Scope of the problem
The scope of the pressure ulcer problem in the United States is examined in terms of the patient’s age and diagnosis and the setting. Statistics about pressure ulcers vary because of how data were collected, variations in terminology about prevalence and incidence, concern about litigation, and political and social events that changed American health care. The concepts of prevalence and incidence and methods for calculation are discussed in Chapter 1.
Prevalence
The WOCN Society (2004) defines pressure ulcer prevalence as the number of patients with at least one pressure ulcer who exist in a given patient population at a given point in time. In the United States, the 6-year sequential analysis of pressure ulcer prevalence ranges from 14% to 17% (Whittington and Briones, 2004). The prevalence of pressure ulcers in long-term care has been reported as 27.3%, with 8.5% being nosocomial (VanGilder et al, 2008; Whitney et al, 2008). The prevalence of pressure ulcers in home care ranges from 3% to 10% (Bolton et al, 2008). The 2003 National Pediatric Pressure Ulcer and Skin Breakdown Prevalence Survey found a pressure ulcer prevalence of 4%; 92% of pressure ulcers were partial-thickness ulcers and 66% were facility acquired (McLane et al, 2004). The discrepancies in prevalence can be attributed to the fact that some studies include intact pressure-damaged skin (suspected deep tissue injury, or Stage I), whereas other studies exclude such lesions. Prevalence is lower when intact pressure-damaged skin is excluded from the sample. Pressure ulcers in dark-skinned persons may also be difficult to detect (Black et al, 2007). Some skin conditions, such as candidiasis and herpetic lesions, may be misclassified as pressure ulcers. In infants and children, the diagnosis of a pressure ulcer is carefully considered because the most common types of skin breakdown in this group include diaper dermatitis, skin tears, and intravenous extravasation (McLane et al, 2004). Data collectors must accurately distinguish between pressure ulcers and other causes of erythema and skin ulcerations.
Incidence
The WOCN Society (2004) defines incidence as the number of patients who initially were ulcer-free who develop a pressure ulcer within a particular time period in a defined population. Incidence measures new conditions (e.g., pressure ulcers) and therefore is considered more reflective of the quality of care within that setting. It is a measure used to evaluate the effects of preventive and therapeutic interventions. Determining the incidence of pressure ulcers is inherently difficult because such studies require longitudinal observations. As with prevalence, incidence will vary by setting. The incidence of pressure ulcers in acute care ranges from 7% to 9% (Whittington and Briones, 2004). The incidence in long-term care ranges from 3% to 31% (Shukla et al, 2008) and in home care ranges from 0% to 17% (NPUAP, 2001).
Considerable methodologic issues surround the calculation of incidence. For example, defining who is at risk (the number used in the denominator of the incidence formula) can have a significant influence on the resulting value, which actually may overestimate or underestimate the true frequency of the condition. Consequently, variation in reports of incidence may reflect a real difference in the frequency of the condition or simply different data collection techniques, definitions, and methods. Although differences in methodology make comparisons difficult, incidence remains an important measure. Consistency in data collection technique within the health care setting is essential to generate data that can be compared over time. National standards for the definition of terms and the process for conducting prevalence and incidence studies will also increase the comparability of these kind of data (WOCN Society, 2004). The National Database of Nursing Quality Indicators (NDNQI) includes pressure ulcer prevention and hospital-acquired pressure ulcer reports from more than 1,100 facilities in the United States designed for comparisons between hospitals of similar sizes and practice levels (Montalvo, 2007).
Economic effects
In fiscal year 2007, a preventable pressure ulcer was listed as a secondary diagnosis for 257,412 Medicare patients. The average payment for admission in which a pressure ulcer was present was $43,180 (Armstrong et al, 2008). In 2008, the Centers for Medicare and Medicaid Services (CMS) ceased payment for hospital complications considered reasonably preventable, including Stage III or IV pressure ulcers (see Chapter 8). CMS with the Centers for Disease Control and Prevention (CDC) released new codes for pressure ulcers capturing wound severity (Krapfl, 2008).
Literature reports a range of costs for pressure ulcer management. Approximately, 2.5 million patients are treated each year in U.S. acute care facilities for pressure ulcers, and the cost of treating pressure ulcers is estimated at $11 to $17.2 billion annually (Ayello and Lyder, 2008; Bolton et al, 2008). Pressure ulcers lead to loss of function, infection, and extended hospital stays, all of which can increase cost. Hospital length of stay for a principal pressure ulcer diagnosis was 14.1 days compared to 12.7 days for a secondary pressure ulcer diagnosis. The average cost per hospital day for a principal pressure ulcer diagnosis was $1,200 compared to $1,600 for a secondary pressure ulcer diagnosis. Three of four hospitalizations with a pressure ulcer diagnosis were billed to Medicare; Medicaid patients accounted for additional 12.5% of hospitalizations with a principal pressure ulcer. More than half of patients with pressure ulcer stays were discharged to long-term care, which is more than three times the rate of hospitalizations for all other causes (Russo et al, 2008).
Impact on quality and duration of life
Pressure ulcers may affect psychosocial needs and quality of life in terms of occurrence, recurrence, ulcer characteristics, and ulcer demands. Pressure ulcers may cause social isolation and add burden and frustration for the patient, the family, and care providers. Aspects of quality of life include change in body image, pain, odor and drainage, and financial impact (Langemo, 2005). Quality-of-life research studies about persons with pressure ulcers tend to have small sample sizes, so additional research is needed. Important factors to assess are the patient’s social networks, the patient’s living space and environment, and the patient’s mental status, learning needs, and personal goals. Pain is an ever-present problem with pressure ulcers and must be assessed (Pieper et al, 2009). Pain assessment and management is discussed in detail in Chapters 25 and 26.
Pressure ulcers have been examined in terms of their effects on mortality rates. In 2006, hospital mortality among persons with a secondary diagnosis of a pressure ulcer was 11.6% and was 4.2% among those with a pressure ulcer as a principal diagnosis (Russo et al, 2008). Approximately 60,000 patients die each year from pressure ulcer complications (Ayello and Lyder, 2008). Pressure ulcers were reported as a cause of death among 114,380 persons (1990–2001), and the age-adjusted mortality rate was 3.79 per 100,000 population. Pressure ulcers deaths occurred mostly in persons at least 75 years old, and septicemia was reported in 39.7%. Mortality rates were higher in African Americans than in persons of other racial/ethnic groups (Redelings et al, 2005). In a home care project in Italy, residents with a pressure ulcer had a relative risk of dying of 1.92 after adjusting for age, gender, and all significant variables between the two groups of patients (Landi et al, 2007).
Vulnerable patient populations
Historically, older adults admitted to acute and long-term care facilities have been a vulnerable population. Nearly 3 (72%) of 4 older adult patients hospitalized with a secondary pressure ulcer diagnosis and 56.5% of adults with a principal diagnosis of a pressure ulcer were 65 years of age or older (Russo et al, 2008). Among persons admitted to long-term care, 10.3% to 18.4% had one or more pressure ulcers on admission (Baumgarten et al, 2003; Siem et al, 2003). The presence of an existing pressure ulcer at the time of admission to acute care was 26.2% among persons admitted from a nursing home and 4.8% among those admitted from another living situation (Keelaghan et al, 2008). For older adults with a pressure ulcer, coexisting conditions were fluid and electrolyte disorders, nutritional disorders, diabetes mellitus without complications, and dementia (Russo et al, 2008).
Pressure ulcer prevalence for persons with spinal cord injuries ranges from 20% to 66% (Schubart et al, 2008). Paralysis and spinal cord injury were common coexisting conditions among younger adults hospitalized principally for pressure ulcers (Russo et al, 2008). Those with the greatest level of disability and mobility impairment have the highest pressure ulcer risk. Other risk factors are history of pressure ulcers, coexisting medical conditions, rehospitalizations, nursing home stays, less than high school education, older adult, male, African American, and single (Schubart et al, 2008).
In a study involving 37 facilities, the incidence of pressure ulcers related to the surgical event was 3.5% (Aronovitch, 2007). Associated factors were at least one comorbidity, managed with a warming device, receipt of three or more anesthetic agents, and median operative time of 4.48 hours (Aronovitch, 2007). Tissue damage may become apparent within hours or may be delayed for up to 3 days. Initial manifestations may be skin discoloration (e.g., bruising) that evolves into blister formation or necrosis. Because this process transpires over several days (i.e., 2–6 days), isolating the time of the original injury is complicated (Price et al, 2005). Because the length of surgery and other variables for the surgical patient cannot be changed, the surgical team must aim to decrease pressure and shear not only during the procedure but also when transferring the patient into position before and after the procedure (Schoonhoven et al, 2002).
Both the obese and the underweight patient populations are vulnerable to pressure ulcer development. The morbidly obese are at risk for pressure ulcers due to their inability to turn themselves, underlying diseases, improper equipment, lack of adequate pressure redistribution, inadequate staff numbers, or staff not trained in how to turn and move such patients (Knudsen and Gallagher, 2003; Mathison, 2003). In a study of elderly patients admitted to acute care, the odds of developing a pressure ulcer in patients who were obese and those who were severely obese were very low (odds ratio 0.7 and 0.1, respectively). In contrast, the odds of the underweight patient developing a pressure ulcer was almost doubled (odds ratio 1.8) (Compher et al, 2007).
Two additional vulnerable patient populations are children and patients at end of life. Pressure ulcer prevalence, incidence and risk factors for these two patient populations are presented in Chapters 36 and 37 respectively.
Terminology
Over the years, several terms have been used to describe pressure ulcers: bedsore, decubitus ulcer, decubiti, and pressure sore. Pressure ulcer is the accepted term because it is more accurate and descriptive. The origin of the term bedsore is not known, but it predates the term decubitus. Decubitus, a Latin word referring to the reclining position (Fox and Bradley, 1803), dates from 1747 when the French used it to mean bedsore. However, this term is inaccurate because it does not convey the tissue destruction associated with these lesions and because these lesions result from positions other than the lying position (such as sitting) (Arnold, 1983).
A pressure ulcer is defined as localized injury to the skin and/or underlying tissue usually over a bony prominence as a result of pressure or of pressure in combination with shear and/or friction. A number of contributing or confounding factors are associated with pressure ulcers, but the significance of these factors has not yet been elucidated (NPUAP, 2007).
Pressure ulcers occur most commonly over a bony prominence, such as the sacrum, ischial tuberosity, trochanter, and calcaneus; however, they may develop anywhere on the body (e.g., underneath a cast, splint, or cervical collar). Figure 7-1 shows common sites for pressure ulcers and frequency of ulceration per site. The majority of pressure ulcers occur in the pelvis, but other more common locations are the sacrum and the heels (VanGilder et al, 2008).
Causative factors
Pressure is the major causative factor in pressure ulcer formation. However, several factors play a role in determining whether pressure is sufficient to create tissue ischemia proceeding to tissue death. The pathologic effect of excessive pressure on soft tissue can be attributed to (1) intensity of pressure, (2) duration of pressure, and (3) tissue tolerance (ability of skin and its supporting structures to endure pressure without adverse sequelae). Braden and Bergstrom (1987) presented a model of the factors that contribute to the intensity and duration of pressure ulcers (Figure 7-2), in combination with intrinsic and extrinsic factors that affect tissue tolerance.
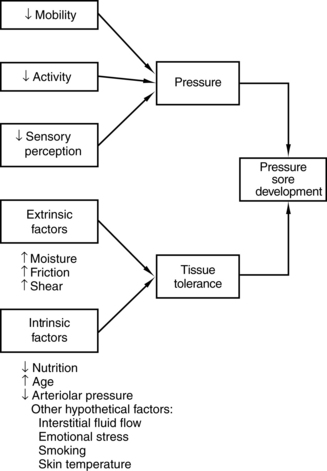
FIGURE 7-2 Factors contributing to the development of pressure ulcers.
(From Braden B, Bergstrom N: A conceptual schema for the study of the etiology of pressure sores, Rehabil Nurs 12(1):9, 1987.)
Intensity of pressure
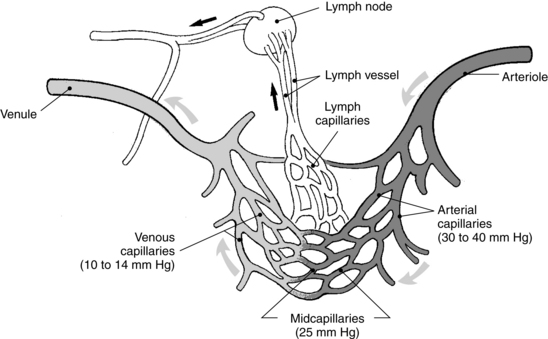
To understand the importance of intensity of pressure, it is important to review the terms capillary pressure and capillary closing pressure. Capillary pressure tends to move fluid outward through the capillary membrane. Exact capillary pressure is not known because of the difficulty of obtaining the measurement. Various methods have been used to estimate capillary pressure. A normal hydrostatic pressure is approximately 32 mm Hg at the arterial end of a capillary bed and 12 mm Hg at the venous end (Figure 7-3) (Kumar et al, 2005a). The mean colloidal osmotic pressure in tissue is approximately 25 mm Hg.
The term capillary closing pressure, or critical closing pressure, describes the minimal amount of pressure required to collapse a capillary (Burton and Yamada, 1951). Tissue anoxia develops when externally applied pressure causes vessels to collapse. It is believed that the amount of pressure required to collapse capillaries must exceed capillary pressure, which is considered to be 12 to 32 mm Hg, the numerical “standard” for capillary closing pressure.
To quantify the intensity of pressure being applied externally to the skin, interface pressures are measured. Numerous studies measuring interface pressures have been conducted (Kosiak, 1961; Kosiak et al, 1958; Lindan, 1961). These studies showed that interface pressures attained while a person is in the sitting or supine position commonly exceed capillary pressures (Bennett et al, 1984). In 1961, Lindan used an experimental “bed” to calculate the pressure distribution over the skin of a healthy adult male in the supine, prone, side-lying, and sitting positions. Interface pressures ranged from 10 to 100 mm Hg. Interface readings as high as 300 mm Hg have been obtained over the ischial tuberosity of healthy, able-bodied male subjects when sitting in an unpadded chair (Kosiak, 1961).
Because head of bed elevation is important for mechanically ventilated patients in critical care and head of bed elevation greater than 30 degrees exposes the patient to increased shear injury and unrelieved pressure, Peterson et al. (2008) examined sacral interface pressures at elevations of 0, 10, 20, 30, 45, 60, and 75 degrees in 15 healthy subjects. The elevations 30 degrees or greater had peak interface pressures significantly higher than supine. In addition, elevations 45 degrees or higher had bed interface pressures greater than 32 mm Hg (Peterson et al, 2008).
Duration of pressure
Duration of pressure is an important factor that influences the detrimental effects of pressure and must be considered in tandem with intensity of pressure. An inverse relationship exists between duration and intensity of pressure in creating tissue ischemia. Specifically, low-intensity pressures over a long period can create tissue damage just as high-intensity pressure can over a short period (Figure 7-4). Husain (1953) underscored the significance of the relationship between duration and intensity of pressure. Husain found that a pressure of 100 mm Hg applied to rat muscle for 2 hours was sufficient to produce only microscopic changes in the muscle. However, the same pressure applied for 6 hours was sufficient to produce complete muscle degeneration.
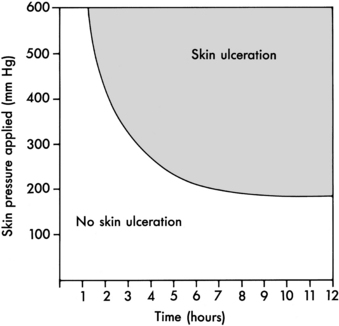
FIGURE 7-4 Graph demonstrating relationship between intensity and duration of pressure.
(From Kosiak M: Etiology of decubitus ulcers, Arch Phys Med Rehabil 42:191, 1961.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree