Preoperative Planning for Revision Total Hip Arthroplasty
Mohamed E. Moussa
Hany S. Bedair
Case
A 75-year-old female presented 15 years following a left primary total hip replacement that had been functioning well until 6 weeks ago, when she noted progressively worsening thigh pain and greatly limited mobility. She denied fever, chills, and her incision was pristine. A radiograph (Fig. 99.1) showed significant loosening of a cemented femoral component and marked varus alignment. In this chapter, an overview of preoperative planning for revision hip arthroplasty will be discussed and the solution to this case will be presented at the conclusion of the chapter.
 Figure 99.1. Prerevision radiograph showing loosening of a cemented femoral component in a 75-year-old woman, 15 years following primary total hip replacement. |
Indications for Revision
Although total hip arthroplasty is a highly successful procedure, it is inevitable that failures arise resulting in the need for revision surgery. These can include infection, periprosthetic fracture, recurrent dislocation, wear, osteolysis, and aseptic loosening. Once an indication for revision has been identified, the importance of preoperative planning cannot be understated in achieving a successful reconstructive outcome. An operation to revise a failed total hip arthroplasty undertaken without a sound preoperative plan will almost certainly lead to failure.
Careful evaluation of a patient’s history, physical examination, laboratory results, imaging, prior operative procedures, and existing implants are necessary to elucidate the mode of failure. Once recognized, a strong foundation in knowledge of techniques of component and cement removal as well as the wide variety of revision implants available to address each clinical situation is necessary. Furthermore, a consideration of additional factors such as bone deficiencies, soft tissue quality, and leg-length discrepancy cannot be overlooked. Often, these patients have other confounding medical comorbidities that need optimization prior to surgery such as their nutritional status or glycemic control. An understanding of the patient’s baseline functional status prior to surgery is necessary to have a clear discussion with the patient regarding postrevision goals and expectations.
Critical Information in the History and Physical Examination
History
A history of previous procedures on the hip, current components in place, as well as any postoperative complications and associated subsequent interventions need to be well documented. Confirming the components that the patient has in place is critical to a successful outcome. The first step is a review of the patient’s prior operative note or notes to confirm the prior operative approach and to determine the manufacturer, model and sizes of the implanted components. Unfortunately this information is oftentimes
poorly documented in the operative note (1) and additional measures will be required. If this information is not available in the operative note, the next step will be to try and obtain the implant stickers from the hospital where the procedure was performed (Fig. 99.2). If these are not available, oftentimes a careful review of the radiographs will give clues to the implant type and reviewing these films with partners or colleagues, industry representatives, and finally an atlas of hip implants is available (2) that can be used to try and confirm the implant type.
poorly documented in the operative note (1) and additional measures will be required. If this information is not available in the operative note, the next step will be to try and obtain the implant stickers from the hospital where the procedure was performed (Fig. 99.2). If these are not available, oftentimes a careful review of the radiographs will give clues to the implant type and reviewing these films with partners or colleagues, industry representatives, and finally an atlas of hip implants is available (2) that can be used to try and confirm the implant type.
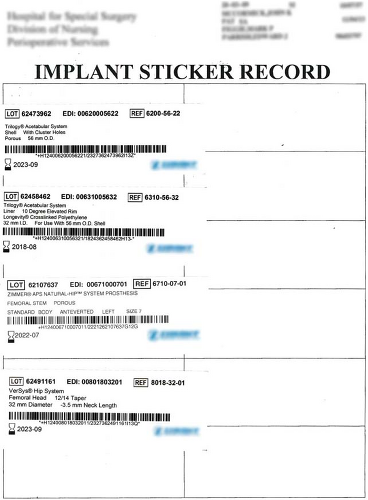 Figure 99.2. Implant stickers from the primary arthroplasty confirm the identity of the implanted components. |
The importance of accurate preoperative implant identification cannot be overstated. Oftentimes, in aseptic revisions, one of the components may be retained and thus appropriate trial heads or liners and implants will be required. Further, some implants may require special extraction techniques or tools. Finally, the track record of a particular implant may push the surgeon toward revision as opposed to retention or the availability of certain head or liner sizes may likewise push the surgeon toward removal as opposed to retention. Given that instability is the most common complication after revision THA, planning preoperatively to maximize stability is critical.
Although a complete discussion of evaluation of the painful THA is beyond the scope of this chapter, needless to say an accurate preoperative diagnosis is critical to a successful revision procedure. Revisions for pain alone or explorations of the joint are discouraged. Finally, the history should be scrutinized for aspects that suggest periprosthetic joint infection such as the use of an extended term of antibiotics in the early postoperative period, returns to the OR early after surgery or a history of pain since the time of surgery that is different than the original pain experienced. These critical aspects of the history should be asked by the surgeon as they are oftentimes not volunteered by patients who do not understand their significance.
Physical Examination
In addition to history, physical examination findings are also equally important. A general assessment of the patient’s overall condition as well as complete examination of the spine, hip and lower extremity is essential. An examination of the contralateral hip is useful for comparison, and an examination of the spine and knee can rule out confounding variables in the examination. Existing scars on the hip should be assessed for healing. In patients with multiple scars, any additional incisions should not further compromise the vascular supply to the skin flaps unless absolutely necessary.
Gait is important to assess and a Trendelenburg gait results from abductor weakness or pain. This could be due to trochanteric nonunion, failed abductor repair, poor muscle strength, damage to the superior gluteal nerve, or inadequate tension in the abductors owing to reduced offset or leg length. As above, dislocation is the most common complication of revision THA and given the importance of abductor function to hip stability, it must be carefully assessed preoperatively. If the abductor mechanism is felt to be incompetent, planning should include the possibility of a constrained liner or dual mobility construct as large heads alone may not be adequate to impart stability to the hip if the abductors are truly deficient (3).
Peroneal and sciatic nerve function should also be evaluated. Branches of the lateral cutaneous femoral nerve may be divided in extensile approaches, and this results in loss of sensation in the area of innervation on the anterolateral aspect of the thigh. Motor and sensory neurologic examinations are done to identify any deficits. The peripheral pulses are assessed. Trophic changes in the foot may indicate poor circulation. Any focus of infection in the extremity has to be treated and should be completely resolved before surgery. A spine examination to rule out spine pathology causing hip pain is carried out, and the ipsilateral knee is examined for range of motion and any laxity or deformity.
Leg-length discrepancy has to be carefully evaluated as it is a common postoperative patient concern and an assessment of where the patient is starting is critical. True leg length is measured clinically with the pelvis square and both lower limbs in identical positions. The distance between the anterosuperior iliac spine and the medial malleolus is recorded. Apparent leg-length discrepancy is an indicator of pelvic tilt leading to abduction or adduction deformity and is measured from the umbilicus to the tip of medial malleolus. Another method of assessing leg-length inequality is to use incremental foot blocks under the shorter leg to get the iliac spines level when the patient is standing. Scanograms are recommended where clinical measurement may be difficult or misleading due to severe hip deformity, scoliosis, flexion contractures, obesity, or when there is an apparent leg-length discrepancy greater than 2 cm. Patients must once again understand the importance of stability in revision THA and that the surgeon may need to lengthen their leg to obtain adequate stability.
The range of motion of the hip joint is next assessed. The Thomas test is useful for detecting any flexion contractures of the hip. In the supine patient, the unaffected hip and knee are flexed to the chest to correct any compensatory lumbar lordosis, and an inability to fully extend the affected hip indicates a flexion deformity. The range of flexion, extension, internal and external rotation, abduction, and adduction are recorded for both the affected and the contralateral hip.
Evaluating Laboratory Studies and Radiographs
Laboratory Studies
In addition to the standard preoperative laboratory tests, an erythrocyte sedimentation rate (ESR) and a C-reactive protein (CRP) level are done routinely to check for infection. In a study of 202 revision hip procedures (4), an elevated ESR over 30 mm/hr was found to have a sensitivity of 0.82 and a specificity of 0.85, and a CRP level over 10 mg/L had a sensitivity of 0.96 and a specificity of 0.92 for diagnosis of infection. Also, all patients with infection had an elevation of at least one of these two markers. The recent AAOS guidelines suggest obtaining an ESR and CRP on all patients being evaluated for periprosthetic joint infection, and a selective approach for hip aspiration based on probability of infection. When both ESR and CRP are elevated, an aspiration is strongly recommended (5).
Preoperative aspiration is generally done when there is a suspicion of infection based on clinical presentation, radiologic signs, and laboratory parameters and is not mandatory prior to all revision surgery. The synovial fluid aspirate should be analyzed for synovial white blood cell count and differential, microorganisms and crystals. The utility of preoperative aspiration in detecting infection is based on the preaspiration likelihood of infection. Preoperative aspiration cultures have a sensitivity of 92% and a specificity of 97% for detecting infection in the hip (6), and have the
advantage of identifying the organism and determining sensitivity to antibiotics. Barrack and Harris (7) reported a 13% false-positive rate in 270 consecutive aspiration procedures before revision hip arthroplasty but this number improved significantly when only those hips that were felt to be potentially infected were aspirated (8). Antibiotics should be stopped at least 2 weeks before aspiration to reduce the risk of false-negative aspirate (5). A negative aspirate does not rule out infection, and the final diagnosis is based on the combination of all preoperative tests and intraoperative tests including frozen-section analysis and periprosthetic tissue cultures (9). Preoperative antibiotics should be withheld until the intraoperative tissue samples are obtained at the time of revision surgery. A synovial white blood cell (WBC) of greater than 3,000 WBCs/mL has been shown to be predictive of periprosthetic joint infection when combined with an elevated ESR and CRP in patients undergoing revision hip arthroplasty (9). More recently, leukocyte esterase colorimetric strip testing of synovial fluid has been shown to have high sensitivity and specificity in the diagnosis of periprosthetic joint infection (10,11).
advantage of identifying the organism and determining sensitivity to antibiotics. Barrack and Harris (7) reported a 13% false-positive rate in 270 consecutive aspiration procedures before revision hip arthroplasty but this number improved significantly when only those hips that were felt to be potentially infected were aspirated (8). Antibiotics should be stopped at least 2 weeks before aspiration to reduce the risk of false-negative aspirate (5). A negative aspirate does not rule out infection, and the final diagnosis is based on the combination of all preoperative tests and intraoperative tests including frozen-section analysis and periprosthetic tissue cultures (9). Preoperative antibiotics should be withheld until the intraoperative tissue samples are obtained at the time of revision surgery. A synovial white blood cell (WBC) of greater than 3,000 WBCs/mL has been shown to be predictive of periprosthetic joint infection when combined with an elevated ESR and CRP in patients undergoing revision hip arthroplasty (9). More recently, leukocyte esterase colorimetric strip testing of synovial fluid has been shown to have high sensitivity and specificity in the diagnosis of periprosthetic joint infection (10,11).
The serum WBC count has traditionally been measured for infection but has poor sensitivity and specificity for detecting hip infections. Many studies have shown it to be elevated in only 15% to 26% of infected hip arthroplasties and is therefore not a useful test (4,6,12). Preoperative nutritional status can be assessed by serum protein levels, lymphocyte count, transferrin levels, and malnutrition corrected prior to revision surgery.
In cases of MoM total hip arthroplasty, obtaining metal ion levels of cobalt and chromium may be useful to evaluate a poorly functioning hip, but a broadly applicable metal ion cut-off level has not been determined to indicate revision surgery (13). Furthermore, there is currently no definitive evidence to suggest these ion levels correlate with soft tissue damage observed at the time of revision surgery (14,15).
Radiographs and Further Imaging
The standard radiographic evaluation for preoperative planning includes four views: a low anteroposterior (AP) view of the pelvis (centered on the pubis), an AP view of the affected hip, a frog-leg lateral view, and a shoot-through lateral view (16) of the affected hip (Fig. 99.3). AP and lateral views of the entire femur are often necessary to determine the entire extent of the existing prosthesis and remaining femoral bone for revision surgery. In cases with cemented femoral stems, the entire cement column should be visible on the radiographs to anticipate any possible difficulty in cement removal. For positioning the AP view, the center of the beam is directed perpendicular to the table at the level of the tip of greater trochanter and 2 in medial to the anterosuperior iliac spine. The natural tendency of the lower limbs to externally rotate in the supine position, along with the normal anteversion of the hip, leads to an apparent reduction in offset and increase in the neck shaft angle measured on the AP view. To avoid this error, it is recommended that the lower limbs be internally rotated by 15 to 20 degrees for measurement of the true offset and neck shaft angle.
The lateral radiograph should show the full extent of the prosthesis and the entire cement column if applicable. Areas of osteolysis, loosening, and cortical thinning should be noted. Assessment of the bow of the femur shaft in the lateral view is required if a long-stem (over 15 cm) prosthesis is planned.
The shoot-through lateral view, also known as the Danelius-Miller modification of Lorenz method, is done with the patient supine and the affected hip extended (Fig. 99.4). The contralateral hip and knee are flexed, and the leg is supported at an elevated position so as not to interfere with the x-ray beam. The beam is directed parallel to the table at 45 degrees to the axis of the body or perpendicular to the axis of the femoral neck and is centered on the femoral head. This is the best projection for estimating the version of the acetabular component on plain radiograph and also yields information on the integrity of the posterior column. In patients with extensive pelvic and acetabular defects or a history of pelvic trauma, Judet views are helpful for assessing the integrity of the anterior and posterior columns and the extent of pelvic bone loss.
Full-length views, AP and lateral, of the femur are required when revision is being planned for long-stem prosthesis, for general deformity of the bone due to systemic disease, following a distal femoral osteotomy, or for revision in the presence of a metastatic lesion in the distal femur. The presence of knee replacement prosthesis with an ipsilateral stemmed femoral component may limit the size and type of femoral component usable in the hip arthroplasty. It may also lead to a stress riser in the intervening bone segment not supported by implants above and below.
The radiographs provide information regarding the position, alignment, and type of components in the existing arthroplasty. An assessment of the loosening of the implants, degree of osteolysis, quality of the cement column, stress shielding, remodeling, heterotopic ossification, trochanteric union, bone quality, offset, canal size, leg lengths, and any deformities is done. It is oftentimes helpful to compare present radiographs with previous films to note changes in stem position and radiolucent areas. Any implants for prior fracture fixation around the hip should be noted, as these may need to be removed at the time of revision surgery; as noted above in some cases specific implant identification is critical as special screw drivers may be required (i.e., locking plates).
Loosening of cemented femoral components has been divided into three types based on radiologic appearance (17). Definite loosening is defined as migration of the stem, new appearance of a continuous radiolucent line at the stem–cement junction, fracture of the stem, or fracture in the cement mantle (Fig. 99.5). Probable loosening is defined as a continuous radiolucent line at the implant–cement interface on either the AP view or the lateral view. Possible loosening is defined as a radiolucent line extending between 50% and 100% of the cement–bone interface on either the AP view or the lateral view, or both. Debonding between the metal and the cement seen at the proximal and the distal end of the prosthesis is often one of the earliest signs of loosening of a cemented femoral component (18,19). In collarless polished tapered stems, some subsidence of the stem is expected, and this situation does not necessarily indicate a loose femoral component.
In cementless femoral stems, the absence of reactive lines adjacent to porous-coated areas of the implant and the
presence of spot welds indicate osseointegration (20). The presence of a new bone bridging the gap between the porous surface of the implant and the endosteal surface of femur is also a feature of osseointegration.
presence of spot welds indicate osseointegration (20). The presence of a new bone bridging the gap between the porous surface of the implant and the endosteal surface of femur is also a feature of osseointegration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








