Postural Assessment
Steven P. Weiniger DC*
*Private practice in Conyers, Georgia; founder, BodyZone.com.
Why Posture Is Important
Posture is how a body balances. If a body doesn’t balance, it falls down. To analyze posture it is necessary to observe how the body is balancing. Posture is more than muscles and bones. The spine, with its ligaments intact but devoid of muscles, is an extremely unstable structure. Muscles and their complex neuromuscular control are required (a) to provide stability of the trunk in a given posture and (b) to produce movement during physiologic activity (1). The motor system and the nervous system function as one entity (2). Therefore, postural analysis is an assessment of the function of the motor system (bones, muscles, and ligaments) and the nervous system’s control of the motor system.
Postural observations are organic; that is, they deal with the whole organism. Unlike most orthopaedic or neurologic tests, which focus on identifying the specific nature of an injury, illness, or other clinical problem, a postural evaluation looks at the whole person and attempts to assess the relative contributions of myriad postural observations. Posture comprises an accumulation of adaptations and compensations from injuries and habits to allow the body to balance and function effectively.
An individual’s neutral posture occurs when the brain and nervous system use information from three sources to balance the body in space when standing, sitting, or moving:
Eyes: We see what is level.
Ears: The vestibular apparatus gives the brain information about the relative position and motion of each inner ear.
Muscles and joints: Proprioceptors in the muscles, ligaments, and tendons tell the brain how hard each is being stressed.
The brain integrates the information it receives to balance the body.
Architectural Versus Adaptive Postural Changes: Body Types, Injury, and Habit
Postural compensations and adaptations can be both a cause and an effect of a clinical problem. Orthopedic problems frequently cause a postural change, which in turn worsens the orthopaedic problem. Asymptomatic postural problems can cause undue mechanical stress, predisposing an individual to either injury or chronic mechanical stress syndrome.
There is no one “normal” posture. An ideal posture is used as a reference point, but rarely does a patient have “perfect posture.” Since the posture is how the body balances, the ideal posture for an individual distributes the forces of gravity for balanced muscle function. Joints should move in their mid range so as to minimize undue stress and strain on ligaments at the joint’s end range of motion and fully distribute stress on the joint surfaces. A biomechanically efficient posture is maximally effective in that individual’s activities of daily living and avoids injury.
People come in various shapes and sizes and live unique lives, and their postures differ accordingly (Fig. 2-1). An individual learns during childhood to balance the body’s unique architecture. The child’s habits affect his or her posture. Good habits can create a strong and stable posture. Bad habits can train the body for poor posture and instability. Excessive sitting, carrying a heavy backpack, slumping, or poor sleeping position trains the body to a folded-forward posture. Habitual one-sided activities, such as carrying a heavy purse, sitting on a wallet, or facing sidewise to view a poorly placed computer monitor train the body to be asymmetrical from left to right.
Poor posture creates adaptive patterns of body motion. Poor posture and body motion stress the musculoskeletal system, resulting in premature joint wear and susceptibility to injury. Studies show that sports injuries correlate with deviations of body mechanics (3). The incidence of injury in athletes has been linked to postural distortions associated with the site of injury, and those with more than two types of injury have significantly worse postural symmetry.
The human bipedal posture is extremely effective and “the most economical of antigravity mechanisms once the upright posture is attained” (4). However, when there is an illness or injury, the body adapts and moves differently. The body must balance, so the posture adapts to changes in muscle and joint motion and resting positions. Overstressed muscles strengthen and favored muscles weaken.
Posture and body motion are like a fold in a piece of paper. Once folded, the paper will bend along the fold when it is stressed. Similarly, once posture and body motion change to compensate for poor habits or injury, the body continues to assume the same uneven resting posture and follows the same adaptive pattern of motion. Biomechanically speaking, this adaptive posture is almost always inefficient. Mother was right about molding good posture in a child by standing straight with head and shoulders back.
Clinically, a postural change begins a cascade of compensating causes and effects. Subjectively, the patient usually believes he or she is standing straight and balanced, even if a visual inspection shows otherwise. If the brain believes the body is balanced when it is not, posture adaptations cause uneven stress and predisposition to future injury. Over a lifetime, people’s history of injury, daily activities, and habits shape their unique posture.
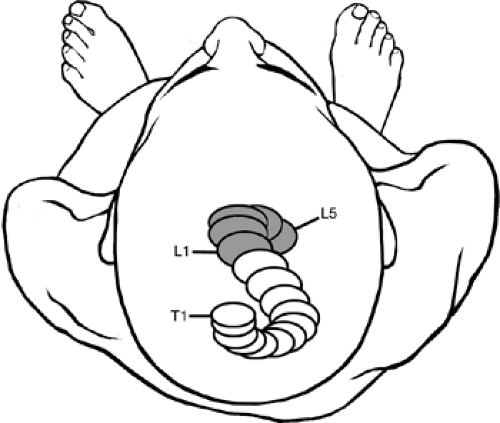
Spinal distortions occur in all directions of three-dimensional space and are more than a sum of the front, back, and side views of the spine. When viewed from above, the helical nature of spinal adaptations becomes apparent (Fig. 2-2) (1). However, according to White and Panjabi (1), present knowledge and technology do not allow effective evaluation of helical adaptations. Nonetheless, posture analysis can provide valuable clinical information that must be correlated with a patient’s history and reported symptoms.
Posture Evaluation: Methods and Observations
A suggested posture evaluation mindset is to think of the body as a stack of children’s blocks (Fig. 2-3). When the blocks are all balanced, the stack is stable. But when one is out of place, the stack wobbles. To balance a stack of blocks, you put the second block on top of the first. When you place the third block on the second, it can be only as stable as the second. Placing a forth block requires stability of the blocks below, and so on. This bottom-to-top arrangement is how human beings balance. That is why shoulder corrections tend to follow correction of lateral pelvic tilt, but the reverse does not necessarily occur.
Additionally, in posture analysis and clinical treatment, it is important to determine whether a muscle is weak or inhibited. A weak muscle is unused because it is unstressed and should therefore be strengthened with exercise. An inhibited muscle is not used because its antagonist is being adaptively overused. The neurologic reciprocal inhibition of a muscle by its antagonist results in overdevelopment of the muscles most used in posture and underdevelopment of their antagonists (2).
Clinically, the goal is to identify the most important fault in the kinetic chain. Since postural analysis can be diagnostic and possibly suggest therapeutic actions, it is imperative to differentiate between actions and reactions. Unbalanced postures have compensating reactions. When observing the posture, the examiner should note any inconsistencies or imbalances, both from left to right and from front to back. Mentally integrate the patient’s complaint and history with the mechanics of the body’s balance. Palpation can help differentiate longstanding adaptive muscle hypertrophy (unilaterally tight muscles without significant reactive pain on palpation) from acute muscle spasm (with reactive pain on palpation).
Prior to postural evaluation, the examiner should obtain all pertinent history, including a description of symptoms, fractures, injuries, congenital abnormalities, and the patient’s dominant hand. It is important to note any gross structural asymmetries, scoliosis, or other condition that creates imbalance.
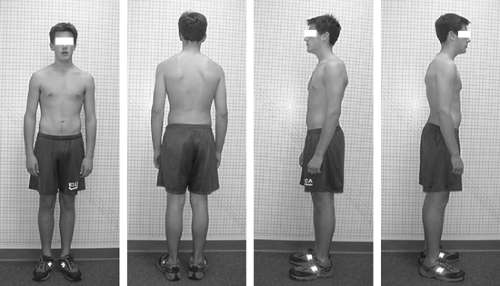
The patient should be as minimally clothed as possible so that the examiner may clearly visualize the contours, bony prominences, and other anatomical landmarks from the front (anteroposterior [AP] view), back (posteroanterior [PA] view) and sides (left and right lateral views) (Fig. 2-4).
The patient should be told to stand straight and look straight ahead. The patient who adopts a rigid standing straight posture (i.e. bilateral shoulder or abdominal tightening on assuming a straight posture) should be told to relax and assume a comfortable position. Patients will try to assume a “good” posture, so to observe a true resting posture it is important not to coach patients by asking them to straighten up what is misaligned.
If there is poor alignment of the feet and the torso or if both feet are not facing at the same angle, instruct the patient to march in place for five steps. A postural distortion is indicated if the feet and torso are still misaligned.
In a balanced posture, the body appears equal from left to right. A vertical plumb line over the center of the body (Fig. 2-5) should show alignment of the occipital protuberance; cervical, thoracic, and lumbar spinous processes; coccyx; and gluteal folds. The arms should hang equally from the torso, with an equal and small amount of the palms visible. The space between the arms and the body should be the same on both sides. The legs should appear equally abducted from the centerline, and the backs of the knees should appear the same. The ankles and feet should display bilaterally symmetric alignment (e.g., no pronation or supination) and toe out. In balanced posture, the following structures should be level and equal: tips of the mastoid processes, acromia, scapula, lower margins of the 12th ribs, iliac crests, posterior superior iliac spines, and ischial tuberosities.
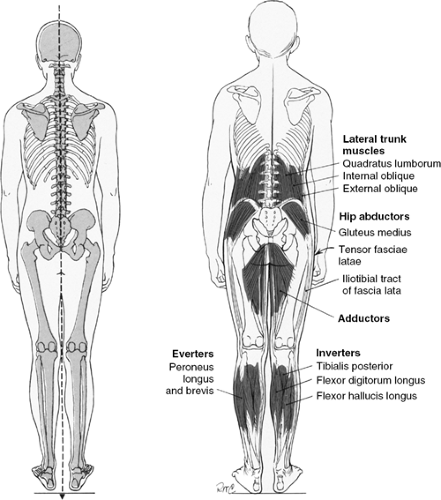 Figure 2-5. Ideal alignment, posterior view. (Modified with permission from Kendall FP, McCreary EK, Provance PG. Muscles: Testing and Function. 4th ed. Baltimore: Williams & Wilkins, 1993:88.) |
Most people have a slight postural distortion because of left- or right-hand dominance. Right-handed people tend to have a high right hip and a low right shoulder (Fig. 2-6). Left-handed ones tend to have a high left hip and a low left shoulder. In addition, the normal AP spine has a slight right convex thoracic curve, most likely due to an individual’s left or right-handedness (1).
The examiner should evaluate the patient from both sides. From the side view, a plumb line should show alignment between the external auditory canal, acromion process of the shoulder, axillary line, midpoint of the iliac crest, greater trochanter of the hip, lateral condyles of the femur, and tibia slightly anterior to the lateral malleolus.
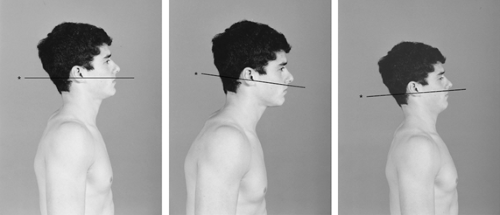
The head, chest, pelvis, and lower extremities should be in alignment and balanced. There should be a normal cervical lordosis, thoracic kyphosis, and lumbar lordosis (Fig. 2-7). The head is balanced when a horizontal line can be drawn from the occipital protuberance to the lower margin of the zygomatic arch. In neutral posture the head should be above the shoulders, not forward. The eyes have a strong tendency to seek level, so if there is postural distortion, the head position may tilt forward or backward to compensate (Fig. 2-8).
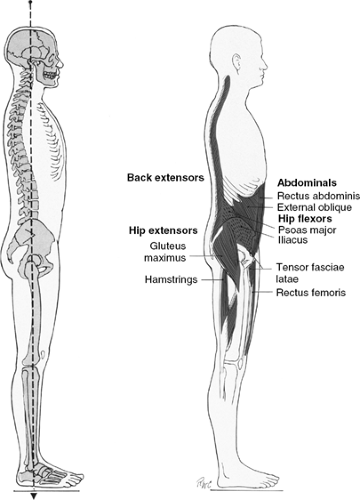 Figure 2-7. Lateral posture alignment. (Modified with permission from Kendall FP, McCreary EK, Provance PG. Muscles: Testing and Function. 4th ed. Baltimore: Williams & Wilkins, 1993:83.) |
On a lateral view, the shoulder girdle and torso are balanced when a horizontal line can be drawn from the medial end of the spine of the scapula to the head of the humerus and then to the medial end of the clavicle. The scapulae should appear equal and lie symmetrically against the torso (Fig. 2-9).
The pelvis is level and balanced when a horizontal line can be drawn from just below the anterior superior iliac spine to the posterior superior iliac spine. Ideally, the anterior superior iliac spine should be vertically aligned with the symphysis pubes (Fig. 2-9).
The lower extremities should be vertically aligned with the knee joints neutral (e.g., not locked in hyperextension). The legs should be equally vertical and at a right angle to the sole of the foot (Fig. 2-9).
Balanced posture should appear equal from left to right. A vertical plumb line over the center of the body will show alignment of the bridge of the nose, center of the chin, episternal notch, xiphoid process, umbilicus, and pubes. The arms should be hanging similarly, both palms at the side of the thighs. Shoulder girdle symmetry is indicated if the hands show similar rotation and placement on the body. The legs should appear equally abducted from the centerline, with the feet displaying bilaterally symmetric alignment (e.g., no pronation or supination) and toe out. The knees should be forward and bilaterally symmetric in their alignment and orientation on the lower extremity (Fig. 2-10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree