Communication and swallowing disorders are common after stroke. Targeted surveillance followed by prompt evaluation and treatment is of paramount importance. The overall goals of rehabilitation for impaired swallowing and communication and swallowing deficits may differ based on the specific deficits caused by the stroke but the main goal is always to improve the patient’s everyday interpersonal interactions and optimize participation in society. Fortunately, therapeutic or compensatory interventions can decrease the effects that communication and swallowing deficits have on the quality of life of stroke survivors.
Key points
- •
Communication and swallowing disorders are very common after stroke.
- •
Evaluation of communication disorders after stroke requires formal testing of each area of language for accurate diagnosis.
- •
Swallowing disorders improve for most stroke patients but chronic deficits occur.
- •
Treatment of swallowing disorders after stroke should focus on the underlying impairment while maintaining the least restrictive diet.
Stroke can significantly affect a person’s ability to communicate and swallow effectively. In many cultures, people interact by conversing during meals. When the ability to express oneself and/or understand others is affected, rehabilitation of other impairments becomes more challenging. The overall goals of rehabilitation for impaired swallowing and communication and swallowing deficits may differ based on the specific deficits caused by the stroke but the main goal is always to improve the patient’s everyday interpersonal interactions and optimize participation in society. The specific goals vary, in part because of the variety of functional deficits caused by the stroke. In impairments of communication and swallowing, involvement of a speech language pathologist is valuable for assessment and treatment.
Communication disorders
Verbal communication is a complex process dependent on intact language, speech, and hearing functions. The focus here is on speech and language because they are most commonly impaired by stroke. A brain lesion can affect (1) the formulation, expression, and/or understanding language (aphasia); (2) planning and/or coordination of articulatory movements and rate/rhythm for speech production (apraxia of speech [AOS]); or (3) motor patterns (dysarthria).
Neural Control
Aphasia
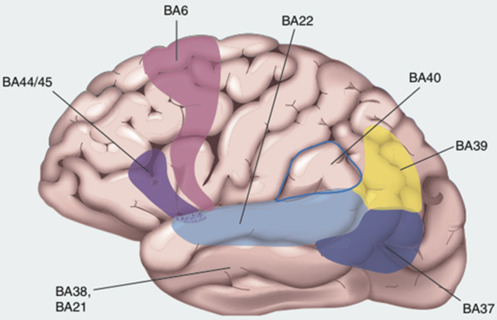
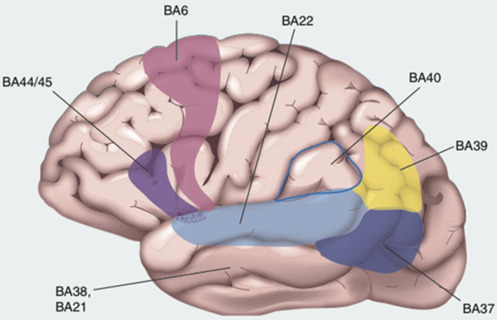
The brain networks that support language function are largely circumscribed to specific areas of the cerebral cortex and the white matter tracts connecting those areas ( Fig. 1 ). Traditional language control models identify Broca area (Brodmann area [BA] 44 and BA45) and Wernicke area (BA22) as among the most crucial cortical locations for language control. Other important areas include the angular gyrus (BA39) and the inferior temporal cortex (BA21). The left posterior inferior frontal gyrus or Broca area is related to most language functions including comprehension and production of language. The superior temporal cortex (Wernicke area) has been associated with language reception and processing. Other important areas include BA6, premotor cortex; BA40, supramarginal gyrus; BA37, posterior inferior and middle temporal cortex and fusiform cortex; BA21, inferior temporal cortex; and BA38, anterior temporal cortex.
Dysarthria
Dysarthria occurs when weakness, dyscoordination, and/or sensory loss affect muscle function in one or more of the five subsystems of speech (ie, respiration, articulation, phonation, resonance, and/or prosody [rate/rhythm]). There is abnormal neuromuscular control of the structures involved in speech generation. The motor control of the larynx, pharynx, tongue, and lips occurs at the level of the primary motor cortex (M1) through the internal capsule to the brainstem nuclei. Such structures as the basal ganglia, red nucleus, substantia nigra, reticular formation, and cerebellum are also important in speech production as part of the extrapyramidal system. The principal cranial nerve nuclei for the muscles of speech production are the trigeminal, facial, and hypoglossal motor nuclei, and the nucleus ambiguous; they are located in the medulla and pons.
Apraxia of speech
In people who have AOS the high level organization of motor speech is impaired resulting in an inability to plan or coordinate articulatory movements. In this context the person “knows what he or she wants to say and how it should sound” but cannot effect these plans of action into accurate speech. Lesions in the left inferior frontal gyrus (Broca area) have been associated with AOS. Others challenge this notion and have proposed that the left anterior insular cortex is more frequently damaged in AOS. A study contrasting patients with acute stroke with and without insular damage failed to find a significant association between AOS and the insula. Conversely, a strong association was found between AOS and lesions in the left inferior frontal gyrus. Other areas have also been associated with AOS. These include left subcortical structures within the basal ganglia and the left frontal and temporoparietal cortices.
Diagnosis
Accurate diagnosis of speech and language deficits requires a systematic approach. Specific language areas and speech in the context of its subsystems have to be tested and deficits clearly described. Treatment efforts are later tailored based on comprehensive testing. A comprehensive speech and language evaluation should include the following:
- 1.
Formal testing within each of the specific language domains.
- 2.
Comprehensive motor speech evaluation to include pitch, loudness, voice quality, duration, contextual speech component integration, and intelligibility and a focused cranial nerve examination.
- 3.
Formal examination of speech samples to characterize phonemic errors and their frequency and pattern.
Aphasia
Important areas in the evaluation of stroke survivors with aphasia include auditory comprehension, reading comprehension, verbal expression, and written expression. Several batteries are available including the Boston Diagnostic Aphasia Examination and the Western Aphasia Battery.
Aphasia has been traditionally classified into various syndromes based on clinical deficits ( Table 1 ). Classification is based primarily on the identification of deficits in three areas: (1) repetition, (2) auditory comprehension, and (3) fluency. These aphasia syndromes do not have a single underlying cause but tend to co-occur because the brain areas responsible for these functions have shared vascular supply. The co-occurrences of these deficits are important because it can allow clinicians to predict stroke location based on the presence or absence of specific clinical deficits. The use of this classification has been challenged because it has been proposed that classification should be based on theoretically significant groups.
| Syndrome | Fluency | Repetition | Comprehension | Content | Naming | Spelling | Reading | Associated Features |
|---|---|---|---|---|---|---|---|---|
| Broca | Poor | Poor (nonfluent) | Intact for words/simple sentences | Good | Worse for verbs | Poor | Poor | AOS Right arm weakness |
| Wernicke | Good | Poor (jargon) | Poor | Poor | Worse for nouns | Poor | Poor | Superior visual field cut |
| Conduction | Fair-good | Poor | Intact for words/simple sentences | Good | Fair-good | May be spared | May be spared | Poor working memory |
| Transcortical motor | Poor | Good | Intact for words/simple sentences | Good | Fair-good | May be spared | May be spared | Abulia |
| Transcortical sensory | Good | Good | Poor | Poor | Poor | Poor | Poor | Right visual field cut |
| Mixed transcortical | Poor | Good | Poor | Poor | Poor | Poor | Poor | Right hemiplegia |
| Global | Poor | Poor | Poor | Poor | Poor | Poor | Poor | Right hemiplegia |
| Anomic | Good | Good | Good | Good | Worse for nouns | May be spared | May be spared | — |
Dysarthria
Evaluation of the patient with dysarthria includes evaluation of neuromuscular function and speech characteristics. Evaluation should include assessment of prosody (rate and the rhythm, stress, and intonation of speech), articulation (intelligibility), velophayngeal function and resonance (sound quality), phonation (voice qualities, such as pitch variability), and respiratory function (coordination and loudness). Based on these characteristics, dysarthria may be classified into the following groups: ataxic, hyperkinetic, hypokinetic, spastic, flaccid, unilateral upper motor neuron, or mixed. Ataxic dysarthria is associated with cerebellar lesions resulting in speech that is dyscoordinated. Disorders affecting the basal ganglia result in hyperkinetic dysarthria. Lesions in the substantia nigra are associated with hypokinetic dysarthria. Spastic dysarthria, characterized by speech slowness and reduced range of motion of articulators, is associated with lesions of the corticopontine or corticobulbar pyramidal tracts. Flaccid dysarthria often presents with varying degrees of slow, labored, and imprecise articulation; a hypernasal resonance; and a hoarse voice, most often related to conditions commonly associated with brainstem impairments. Unilateral upper motor neuron dysarthria is characterized by imprecise articulation and slowed rate and a monotone quality voice and is linked to unilateral upper motor neuron lesions in the central nervous system bulbar or pseudobulbar syndromes.
Apraxia of speech
The apraxia battery for adults is the most commonly used test for AOS evaluation. Other tests available include the Quick Assessment of Apraxia for Speech and the Motor Speech Evaluation. Deficits seen in AOS are difficult to differentiate from those seen in other speech-language disorders. As such, the evaluation of patients by an experienced speech-language pathologist is of paramount importance.
Treatment
Aphasia
Treatments of aphasia can be broadly classified as behavioral or biologic. Behavioral language therapy uses various approaches including stimulation, facilitation, modality model, nondominant hemisphere approach, neurolinguistic, functional communication or pragmatic, or information processing. These treatment approaches are summarized in Table 2 .
| Approach | Treatment Characteristics and Techniques |
|---|---|
| Stimulation-facilitation | Targets access to language and not complete loss of language to improve language processing Treatment involves intensive auditory stimuli and repetition Errors are not corrected – followed by additional stimulation |
| Modality model | Language is multimodal thus aphasia is modality specific Performance in strong performing modalities is used to improve performance of weak modalities |
| Information processing | Based on the cognitive models developed for the specific tasks that are part of language: reading, spelling, naming, semantics, sentence production, auditory discrimination/recognition Treatment focuses on the specific process impaired When treatment of impaired processes is not successful compensation using intact processes is used |
| Nondominant hemisphere | Based on the hypothesis that nondominant hemisphere capabilities may facilitate communication Visual-spatial, paralinguistic, or musical skills are used to facilitate language |
| Neurolinguistic | Based on the premise that a specialized rule system applies to the organization of language Treatment focuses on improving disrupted rule-systems (phonologic, semantic, or lexical) by targeting the specific linguistic impairment |
| Functional communication (pragmatic) | This technique focuses on improving the person’s ability to communicate instead of the linguistic accuracy of the message Environmental modifications to facilitate communication may also be part of this treatment approach |
Biologic approaches aim to restore lost neuromuscular function. They are primarily considered adjuvant to traditional aphasia rehabilitation approaches. These may include such medications as bromocriptine, dextroamphetamines, donepezil, and piracetam. Drugs with opposite effects on neutotransmitters (ie, cholaminergic and GABAergic effects) should be avoided. Cortical stimulation (including transcranial direct current stimulation and transcranial magnetic stimulation) is thought to facilitate recovery by fostering brain plasticity. For a summary of the evidence on therapeutic interventions for aphasia see the review by Allen and colleagues.
In severe cases, alternative means of communication may be necessary. These include the use of writing, drawing, communication books, or electronic communication devices. Applications have been developed for this purpose for use with smartphones or tablet computers.
Apraxia of speech
The main goal of treatment in AOS is to improve functional communication. Affected features of speech, such as articulatory accuracy, rate, timing, or rhythm, should be targeted specifically. Spared systems can be used to facilitate speech production. Singing or intonation therapies are techniques designed to engage the undamaged contralateral hemisphere to facilitate speech production. The evidence summarized in a recent systematic review suggests a strong effect of articulatory/kinematic and rate/rhythm approaches for the treatment of AOS.
Dysarthria
Treatment of dysarthria focuses on improving control for breathing related to speech, phonation, resonance, articulation, and prosody. Exercises can improve muscle tone, strength, coordination, and precision of speech. Biofeedback can also be helpful.
Specific therapeutic approaches for the treatment of dysarthria are described in Table 3 . In severe cases, augmentative communication techniques may be necessary to allow for functional communication.
| Approach | Characteristics |
|---|---|
| Lee Silverman Voice Treatment | Focused on increasing respiratory drive and vocal fold adduction |
| Behavioral communication interventions | Targets management of respiratory/phonation dysfunction Biofeedback Strategies to increase volume, reduce speed of speech, and improve intelligibility Orofacial and articulation exercises |
| Speech supplementation strategies | Gestures Alphabet supplementation Semantic/topic supplementation Syntactic supplementation |
| Systems approach | Targets components, such as breathing, phonation, nasal resonance, articulation, and intonation |
Communication disorders
Verbal communication is a complex process dependent on intact language, speech, and hearing functions. The focus here is on speech and language because they are most commonly impaired by stroke. A brain lesion can affect (1) the formulation, expression, and/or understanding language (aphasia); (2) planning and/or coordination of articulatory movements and rate/rhythm for speech production (apraxia of speech [AOS]); or (3) motor patterns (dysarthria).
Neural Control
Aphasia
The brain networks that support language function are largely circumscribed to specific areas of the cerebral cortex and the white matter tracts connecting those areas ( Fig. 1 ). Traditional language control models identify Broca area (Brodmann area [BA] 44 and BA45) and Wernicke area (BA22) as among the most crucial cortical locations for language control. Other important areas include the angular gyrus (BA39) and the inferior temporal cortex (BA21). The left posterior inferior frontal gyrus or Broca area is related to most language functions including comprehension and production of language. The superior temporal cortex (Wernicke area) has been associated with language reception and processing. Other important areas include BA6, premotor cortex; BA40, supramarginal gyrus; BA37, posterior inferior and middle temporal cortex and fusiform cortex; BA21, inferior temporal cortex; and BA38, anterior temporal cortex.
Dysarthria
Dysarthria occurs when weakness, dyscoordination, and/or sensory loss affect muscle function in one or more of the five subsystems of speech (ie, respiration, articulation, phonation, resonance, and/or prosody [rate/rhythm]). There is abnormal neuromuscular control of the structures involved in speech generation. The motor control of the larynx, pharynx, tongue, and lips occurs at the level of the primary motor cortex (M1) through the internal capsule to the brainstem nuclei. Such structures as the basal ganglia, red nucleus, substantia nigra, reticular formation, and cerebellum are also important in speech production as part of the extrapyramidal system. The principal cranial nerve nuclei for the muscles of speech production are the trigeminal, facial, and hypoglossal motor nuclei, and the nucleus ambiguous; they are located in the medulla and pons.
Apraxia of speech
In people who have AOS the high level organization of motor speech is impaired resulting in an inability to plan or coordinate articulatory movements. In this context the person “knows what he or she wants to say and how it should sound” but cannot effect these plans of action into accurate speech. Lesions in the left inferior frontal gyrus (Broca area) have been associated with AOS. Others challenge this notion and have proposed that the left anterior insular cortex is more frequently damaged in AOS. A study contrasting patients with acute stroke with and without insular damage failed to find a significant association between AOS and the insula. Conversely, a strong association was found between AOS and lesions in the left inferior frontal gyrus. Other areas have also been associated with AOS. These include left subcortical structures within the basal ganglia and the left frontal and temporoparietal cortices.
Diagnosis
Accurate diagnosis of speech and language deficits requires a systematic approach. Specific language areas and speech in the context of its subsystems have to be tested and deficits clearly described. Treatment efforts are later tailored based on comprehensive testing. A comprehensive speech and language evaluation should include the following:
- 1.
Formal testing within each of the specific language domains.
- 2.
Comprehensive motor speech evaluation to include pitch, loudness, voice quality, duration, contextual speech component integration, and intelligibility and a focused cranial nerve examination.
- 3.
Formal examination of speech samples to characterize phonemic errors and their frequency and pattern.
Aphasia
Important areas in the evaluation of stroke survivors with aphasia include auditory comprehension, reading comprehension, verbal expression, and written expression. Several batteries are available including the Boston Diagnostic Aphasia Examination and the Western Aphasia Battery.
Aphasia has been traditionally classified into various syndromes based on clinical deficits ( Table 1 ). Classification is based primarily on the identification of deficits in three areas: (1) repetition, (2) auditory comprehension, and (3) fluency. These aphasia syndromes do not have a single underlying cause but tend to co-occur because the brain areas responsible for these functions have shared vascular supply. The co-occurrences of these deficits are important because it can allow clinicians to predict stroke location based on the presence or absence of specific clinical deficits. The use of this classification has been challenged because it has been proposed that classification should be based on theoretically significant groups.









