(1)
Department of Orthopedic Surgery Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands
Abstract
This chapter describes the endoscopic access to the posterior tibial tendon. The indications, technique, and results are described. Patients tend to show a quick recovery, early mobilization, none or mild postoperative pain, and good wound healing.
The main indication and procedures for posterior tibial tendoscopy are tenosynovectomy, tendon sheath release, adhesiolysis, and tendon debridement in partial rupture.
25.1 Introduction
Disorders of the ankle joint can be caused by intra-articular as well as extra-articular pathology (Fig. 13.7). In the absence of intra-articular pathology, posteromedial ankle complaints most often are caused by disorders of the posterior tibial tendon (Meyerson 1992). In the event of failure of conservative treatment, posterior tibial tendon disorders can be treated by open surgery (Lapidus and Seidenstein 1950; Richardson 1993). An endoscopic procedure offers the advantage of less morbidity, reduction in postoperative pain, and outpatient treatment (Barett and Day 1993). Postoperative open surgical treatment requires plaster immobilization to prevent equines malformation and stimulate wound healing (Lapidus and Seidenstein 1950; Richardson 1993). Endoscopic surgery on the contrary is followed by functional postoperative treatment. A cadaver study was performed, and in a subsequent prospective study, diagnostic and therapeutic tendoscopy (tendon sheath endoscopy) was performed.
25.2 Pathology
The posterior tibial tendon can be subject to a number of pathologic conditions (Bulstra et al. 2006). Two predominant groups with a dysfunction of the tendon can be distinguished: the first group involves younger patients who may present with some form of systemic inflammatory disease, and the second group involves older patients whose dysfunction is caused by chronic overuse (Meyerson et al. 1989). Although the exact etiology of the disorder is unknown, the condition has been classified on the basis of clinical and radiographic findings. In the early stages of dysfunction, patients describe discomfort medially along the course of the tendon in addition to fatigue and aching on the plantar medial aspect of the ankle. In the presence of tenosynovitis, swelling is common. By clinical examination, a valgus angulation of the hindfoot and abduction of the forefoot can be seen and a “too-many-toes” sign is described (Trnka 2004). For radiographs, MRI scanning is the best method for assessing a ruptured tendon. Investigation by means of ultrasound is a cost-effective and an accurate method for evaluating disorders of the tendon (Miller et al. 1996).
Inactivity of the posterior tibial tendon gives midtarsal instability. The relative strength of the posterior tibial tendon is more than twice that of the peroneus brevis, its primary antagonist. Without the activity of the posterior tibial tendon, there is no stability at the midtarsal joint, and the forward propulsive force of the complex of gastroc-soleus acts at the midfoot instead of at the metatarsal heads. A total dysfunction eventually leads to a flatfoot deformity.
Pain is often located in the relative hypovascular zone immediately distal to the medial malleolus. The hypovascularity contributes to the development of degenerative changes and consequent ruptures. We described the vincula that connect the posterior tibial tendon with its tendon sheath (Van Dijk et al. 1997). Damage to the vincula can cause thickening, shortening, and scarring of the distal free edge. In posttraumatic, postsurgery, and postfracture situations, the vincula can be thickened and become symptomatic. In these patients, a painful local thickening can be palpated posterior and just proximal to the tip of the medial malleolus. Most dysfunctions of the tendon eventually lead to a painful tenosynovitis. The conservative treatment includes rest combined with immobilization using plaster or tape and nonsteroidal anti-inflammatory drugs. There is no consensus whether to use steroid injections; ruptures have been described. If conservative treatment fails, then operative treatment can be indicated. An open synovectomy is performed by means of sharp dissection, completely removing all the inflamed synovium while preserving the blood supply of the tendon. Postoperative management includes plaster cast immobilization for 3 weeks followed by wearing a boot with controlled ankle movement for another 3 weeks and physiotherapy (Bare and Hadded 2001). Tenosynovitis is a common extra-articular manifestation of rheumatoid arthritis. Systemic inflammatory disease in the hindfoot in rheumatoid arthritis is a significant cause of disability for patients. Tenosynovitis in rheumatoid patients eventually leads to a ruptured tendon. In a group of patients who had rheumatoid arthritis and hindfoot pathology, Michelson and colleagues (Michelson et al. 1995) found a dysfunction of the posterior tibial tendon in 13–64 % depending on the specific diagnostic criteria. The criteria used were loss of the longitudinal arch, inability to perform a heel rise, or lack of palpable posterior tibial tendon.
25.3 Anatomic Study
Seven ankles in five specimens with no previous history of ankle pathology were dissected (de Leeuw et al. 2009). Special attention was paid to the relation of the posterior tibial tendon to the posteromedial aspect of the tibia, the flexor digitorum longus, the neurovascular structures, and to the insertion onto the navicular bone.
The dorsomedial surface of the tibia has a slightly concave smooth surface. A consistent (seven out of seven) membranous mesotendineal structure was found between the tendon and tendon sheath. This thin vincula-like structure runs between the posterior tibial tendon and the tendon sheath of the flexor digitorum tendon. It runs from all the way proximal to end with a free edge 3–4 cm above the level of the posteromedial tip of the medial malleolus. In six of the seven specimens, a small 1- to 2-cm wide interruption in the vincula was found, 1–2 cm proximal of its distal free edge (Fig. 25.1). As far as we know, these structures have not been previously described at this site. After traumatic injury to the ankle, this mesotendinal structure may have clinical implications.


Fig. 25.1
Anatomic specimen dissection of the right ankle. The posterior tibial tendon sheath has been opened. Proximally (right side of the picture) we see the posterior tibial tendon and behind it the flexor digitorum tendon. The posterior tibial tendon has been dislocated over the edge of the medial malleolus. We see the empty sliding channel between the posterior tibial tendon and the flexor digitorum. Note the vincula that attaches the posterior tibial tendon to the tendon sheath. In all tendisections that we performed, we found this same configuration. The posterior tibial tendon does not have a vincula at the level of the medial malleolus, but has a vincula more distal and more proximal as is shown. This proximal vincula therefore always has a free distal edge. This can become thickened in a pathologic situation (e.g., after direct trauma)
25.4 Surgical Technique
An autopsy study was performed to verify portal anatomy (Reilingh et al. 2010a). Access to the tendon can be obtained anywhere along its course. However, the two main portals are located directly over the tendon 2 cm distal and 2 cm proximal to the posterior edge of the medial malleolus (Fig. 25.2).
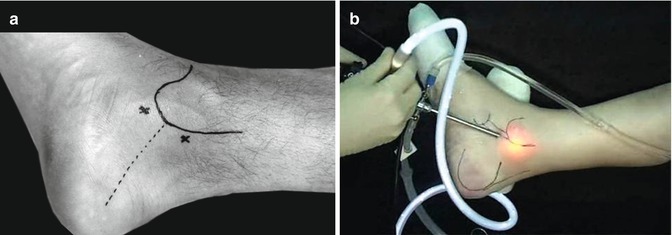
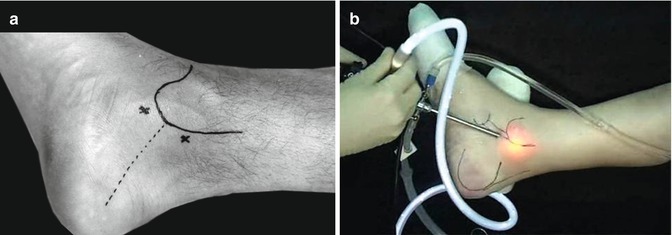
Fig. 25.2
Right ankle. Medial side to show the standard portals 2 cm distal from the posteromedial edge of the medial malleolus and 2 cm proximal. (a) The portals are located over the posterior tibial tendon. (b) The arthroscope in place through the posterior portal. In this case a 4-mm arthroscope has been introduced. We will perform the procedure routinely with a 2.7-mm scope, but in some circumstances it is possible to use the 4-mm arthroscope
The distal portal is made first: the incision is made through the skin only and the tendon sheath is penetrated by the arthroscope shaft with a blunt trocar (Fig. 25.3). The 2.7-mm arthroscope with an inclination angle of 30° is introduced, and the tendon sheath is filled with saline (Fig. 25.4). The 1-mm needle scope and the 1.8-mm arthroscope were used at first but were found to give inferior access and view. Another important advantage of the 2.7-mm arthroscope is the better flow that is necessary when surgery is performed. Under direct visualization, the proximal portal is made by introduction of a spinal needle, and subsequently an incision is made through the skin into the tendon sheath.
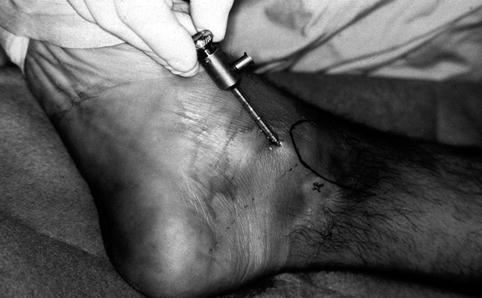
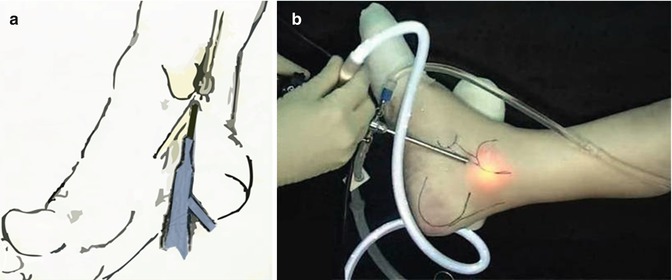
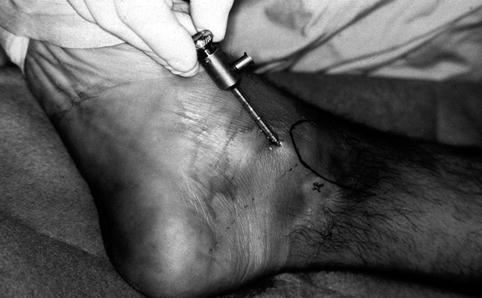
Fig. 25.3
After making a skin incision and using the mosquito clamp with curved tip, the 2.7-mm shaft with blunt trocar is introduced
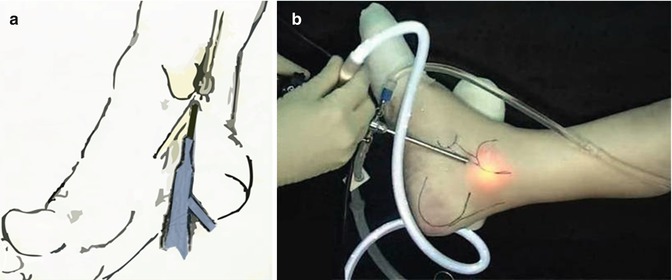
Fig. 25.4
(a and b) The arthroscope is in place through the posterior portal looking proximal
Instruments such as blunt probe, scissors, retrograde knife, and shaver system can be introduced. The distal portal allows a complete overview of the tendon from its insertion to the navicular bone to some 6 cm above the level of the tip of the medial malleolus. The complete tendon sheath can be inspected by rotating the scope around the tendon (Fig. 25.5). Special attention is given to inspect the tendon sheath covering the deltoid ligament, the posterior medial malleolus surface, and the posterior ankle joint capsule. More proximal, the free edge of the vincula can be inspected. The operation is performed as an outpatient procedure under general, regional, or local anesthesia. Local anesthesia has the advantage of a possible dynamic investigation. Before the anesthesia is administered, the patient is asked to actively invert the foot. The posterior tibial tendon thus can be palpated and the location of the portals can be drawn onto the skin. In case of local anesthesia, the anesthetic (plus epinephrine) is administered around the portals and into the tendon sheath. When a total synovectomy of the posterior tibial tendon is to be performed, it is advisable to create a third portal distally. In the case of tendon sheath release, we use a small retrograde knife. Under direct visualization, a release of the complete tendon sheath can be performed from 6 cm above the joint level up to the navicular bone. The neurovascular structures are located posterior and are not in danger because they are still covered by the flexor digitorum tendon. Nevertheless, the release is performed on the medial side.


Fig. 25.5
View of the posterior tibial tendon. Note the small vessels which might indicate a repair process and might indicate a (small) rupture or local degeneration of the tendon
In cases where access to the posteromedial compartment of the ankle joint is desired, this can be obtained by means of posterior tibial tendoscopy approach. The foot is brought into an inverted equines position. The arthroscope is introduced through the distal portal and placed in between the tendon and medial malleolus. The probe comes down from the proximal portal and crosses behind the posterior tibial tendon to palpate the posterior ankle joint capsule. By moving the ankle up and down, the posterior joint level can be identified by the surgeon’s palpating finger from the outside as well as with the probe under direct visualization from inside the tendon sheath. The shaver is introduced through the proximal portal, and the tendon sheath can be opened at the posterior joint level. The posterior joint capsule can then be partially resected, and the arthroscope (through the distal portal) and the shaver or other instrument (through the proximal portal) can both be brought into the posterior ankle joint compartment. Synovectomy or loose body removal can subsequently be performed. There is however only limited possibility for free manipulation of the scope and the instruments. In cases where access to the posterior compartment of the ankle joint or subtalar joint are desired, we much prefer the 2-portal hindfoot approach in the prone position.
At the end of the procedure, the portals are sutured. Postoperative treatment consists of a pressure bandage and partial weight bearing for 4–5 days. Active movements are stimulated from the first day.
25.5 Indications
With an accurate clinical examination, a differentiation can be made between intra-articular and extra-articular pathology in most cases. On the posteromedial side, intra-articular lesions, such as posteromedial impingement syndrome, calcifications in the dorsal capsule of the ankle joint, subtalar pathology, loose body, or osteochondral defect, have to be excluded. The most common extra-articular disorders are tenosynovitis of the posterior tibial tendon, disorders of the flexor hallucis longus tendon, and the tarsal tunnel syndrome.
Postsurgery and postfracture adhesions and irregularity of the posterior aspect of the tibia (posterior tibial sliding channel) can be responsible for symptoms in this region. The posterior tibial tendon plays an important role in normal hindfoot function (Funk et al. 1986). Several investigators have described development of posterior tibial dysfunction as the disease progresses from peritendinitis to elongation, degeneration, and rupture (Meyerson 1992; Richardson 1993; Cosen 1965; Johnson and Strom 1989; Williams 1963).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








