Posterior Occiput-C2 and C1-C2 Cervical Fusion
Leok-Lim Lau
Suken A. Shah
INTRODUCTION
The occipitocervical junction has complex transitional anatomy that allows a significant range of motion in multiple planes while supporting a physiologically normal but disproportionately large cranium in children. Stability is provided by anatomical geometry that facilitates the inherent stability of the articulating joints and substantial ligamentous restraint. Growth of the synchondroses allows expansion of the spinal canal to accommodate the spinal cord. Failure of any of these processes may result in cervical instability and/or stenosis.
PERTINENT ANATOMY
Occipital Bone (Occ)
The occiput has the thickest bone in the midline. It thins out laterally. The thick internal occipital protuberance at the midline provides the best fixation point in the skull. Cranially, the external occipital protuberance is the most prominent portion of the occipital bone (Occ). It corresponds to the confluence of the dural sinuses and should be avoided for any bony fixation.
Atlas (C1)
The atlas is between the occiput and C2 and is the smallest vertebra with limited bony purchase. Occiput to C1 has no intervertebral disc. The convex occipital condyle and concave lateral mass at the sagittal plane facilitate flexion-extension motion of the skull. The joints slope downward medially at the frontal plane, which provides bony stability. The apical ligament, which is a continuation of the posterior longitudinal ligament ,provides significant ligamentous restraint. The range of movement of occiput to C1 is flexion-extension 13 degrees and lateral bending 8 degrees.
The atlas has two anterior neurosynchondroses (between anterior atlas arch and two lateral masses) and a posterior synchondrosis. The anterior neurosynchondrosis closes by age 5 to 7 years, and the posterior synchondrosis closes by age 3 to 5 years and may have a cartilaginous cleft prior to closure. The cervical spinal canal expands rapidly from 0 to 3 years old (reaches 80% of adult canal diameter) with minimal expansion beyond age 6 years.
Axis (C2)
The C1-C2 facet joints have planar articulation to allow lateral rotation movement. The range of movement is as follows: axial rotation movement is 47 degrees, flexion-extension is 10 degrees, and lateral bending is 8 degrees. The taut alar ligament strutted against an intact dens is a significant ligamentous restraint.
C2 has five primary ossification centers: a centrum, two vertically aligned odontoid columns, and two lateral masses. Persistent synchondrosis at the secondary ossification center between centrum and dens beyond the age of 7-year-old results in ossiculum odontoideum. Persistent apicodental synchondrosis (chondrum terminale) at the cranial tip of the dens beyond the age of 12 years results in ossiculum terminale, though ossiculum terminale is more commonly believed to be due to trauma.
Vertebral Artery
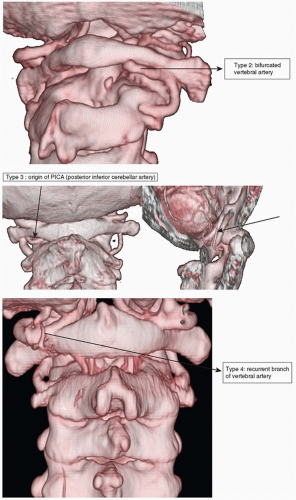
The vertebral artery takes its origin from the subclavian artery. It travels deep to the anterior scalene muscle and is located outside the transverse foramen of C7. The artery runs within the transverse foramen as it ascends from C6 to C2 (V2). At C2 transverse foramen, it emerges and travels laterally to within C1 transverse foramen to loop around it, makes a sharp posteromedial turn just below the superior articular facet of the atlas, runs on the sulcus arteriosus before penetrating the atlanto-occipital membrane and dura, and travels cranially within the dura to enter the foramen magnum. The risk of vertebral artery injury may increase with the following anatomic variants, which can be present in 30% of the population:
The variation in vertebral artery tributaries at C1-C2 area is present in 6% of the population particularly in patients with Down syndrome or Klippel-Feil syndrome. The variation includes persistent first intersegmental artery and bifurcated vertebral artery that may have tributaries posterior to the lateral mass of C1. Rarely, the posteroinferior cerebellar artery may take its origin from the vertebral artery and course around the area near C1 lateral mass entry point (see Fig. 39-1).
The presence of ponticulus posticus (Latin for “little posterior bridge”), an osseous anomaly that projects a vertical ridge at the C1 posterior arch over the crossing vertebral artery at the sulcus arteriosus. It gives an appearance of a broader posterior C1 arch and may misguide C1 screw placement (see Fig. 39-2).
A high-riding vertebral artery is present when the isthmus or pars that adjoins the superior and inferior articular process of the atlas is narrow (≤5 mm) in the parasagittal CAT scan of the trajectories of the planned transarticular screw of C1-C2. The vertebral artery may veer too close to the pars anteroinferiorly from the vertebral artery groove for a safe passage of a transarticular C1-C2 screw or C2 pars screw.
DIAGNOSIS OF CERVICAL INSTABILITY
Cervical instability is diagnosed by imaging. A lateral cervical spine x-ray is used to ascertain static instability or incongruity. In dynamic instability, flexion and extension lateral cervical radiographs are obtained in patients who are conscious and cooperative without any evidence of neurologic deficits. In a child who is too young to follow instructions or unreliable, MRI cervical spine is obtained first in neutral position under general anesthesia with the supervision of an anesthesiologist. An abnormal reading in the neutral position obviates the need to proceed with MRI cervical spine in flexion and extension. This may be followed by flexion and extension views. One may consider clinical evaluation in flexion and extension prior to obtaining flexion and extension views, especially under anesthesia. Dynamic computed tomography (CT) scan is indicated for C1-C2 rotatory subluxation. The CAT scan is performed with patient in the rotated position followed by maximum rotation in the opposite direction.
INDICATIONS FOR ARTHRODESIS
C1-C2 posterior arthrodesis is indicated for patients with atlantoaxial instability that results in spinal cord compression. The hard signs include cervical myelomalacia and direct evidence of spinal cord impingement on MRI scan. Softer radiologic signs are determined by the amount of the instability or Steel’s “rule of thirds.” When coupled with clinical evidence of upper motor neuron signs, surgery is indicated. Dynamic MRI scan is indicated when the clinical signs are absent but instability or dynamic compression is suspected.
C1-C2 instability is determined by lateral cervical spine x-ray or midsagittal MRI cervical spine using atlantodental interval (ADI) or posterior ADI (also known as space available for cord or SAC). Radiologic cervical instability occurs when the ADI is greater than 4 mm in children. In older children than 8 years, cervical instability occurs when ADI is greater than 3 mm. Up to 7 to 10 mm is tolerable in patients with Down syndrome if asymptomatic. SAC of less than 13 mm suggests spinal cord compression. The Steel “rule of thirds” is an alternative way to determine spinal cord compression. A third of spinal canal in C1 is occupied by the dens and spinal cord, respectively. The remaining third is the “reserve zone” to buffer against physiologic movement. Movement beyond “reserve zone” suggests spinal cord impingement. Its utility may be limited in patients with congenital small C1 rings, for example, spondyloepiphyseal dysplasia congenita.
Occiput to C2 posterior arthrodesis is indicated for patients with occiput to C1 instability, C1-C2 vertical instability that results in basilar invagination, or C1-C2 instability that requires C1 posterior arch decompression in a child younger than 3 years old in whom a screw-based construct may not be possible. The indications for C1 posterior arch decompression include congenitally small C1 ring, the presence of pseudotumor at the C1 spinal canal, and unreducible C1-C2 subluxation.
ETIOLOGY OF UPPER CERVICAL INSTABILITY
Congenital and developmental
Down syndrome
Skeletal dysplasia (except achondroplasia)
Os odontoideum or os terminale
Congenital C1 hypoplasia/aplasia
Occipitalization of atlas
Inflammatory
Juvenile rheumatoid arthritis
Seronegative arthritis (e.g., psoriatic arthritis)
Fixed atlantoaxial rotatory subluxation
Tumor
Posterior arch aneurysmal bone cyst
Traumatic
Atlanto-occipital dislocation
Occipital condyle fracture
Odontoid fracture
C1 burst fracture (Jefferson fracture)
Traumatic spondylolisthesis of C2 (Hangman’s fracture)
Iatrogenic
Posterior access to intradural operation (chordoma or intradural abscess)
Extensive C1 decompression for cervical stenosis or Chiari malformation
HALO APPLICATION
Indications
A halo vest is a good option for patients who need immobilization of the upper cervical spine. It allows them to eat, talk, and move their jaw, avoids skin breakdown from chin or occipital pressure, and allows inspection of the surgical area, if needed. It may be indicated for patients who need stabilization after trauma or surgery or those who are not suitable candidates for surgical intervention. Its immobilization may be useful in combination with a wire-based construct, which has little rotational control. In patients with behavioral problems or developmental delay, a halo vest may be used as an adjunct for added immobilization.
Contraindication
Halo rings may not be suitable in children who are less than 1 year old or those with large cranial defects, or poor osteology (osteogenesis imperfecta is a relative contraindication).
Procedure
The halo ring is sized and applied 1 cm cranial to the eyebrows and tip of the ear and caudal to the largest circumference of the skull. A well-fitting halo ring has a fingerbreadth of space between the ring and skull. In very young children, 10 to 12 pins are inserted and torqued to 1 to 2 inch-pounds. In school-going children, as few as 6 pins may be used and torqued to 6 inch-pounds. In older adolescents, 4 pins are used and torqued to 6 or 8 inch-pounds. The pins are positioned at anterolateral and posterolateral aspects of the halo ring. The tips of the pins are dipped in iodine solution. The skin and underlying periosteum at the pin site is preinjected with local anesthetic in the awake patient. Ensure that the eye is tightly closed and the eyebrow is drawn down prior to pin penetration to avoid undue tethering of the orbicularis oculi muscle that may prevent complete eye closure. The pins are applied and torqued opposite to each other to maintain the ring at a central position. The anterolateral safe zone is at the outer third of the eyebrow, which avoids supratrochlear nerve and artery, which is along the medial eyebrow. A halo adaptor can be attached to a radiolucent table for surgical positioning, or the bars can be connected to the vest.
PREOPERATIVE PREPARATION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree