Fig. 16.1
The overhead throwing motion can be broken down into six phases: (1) windup, (2) early cocking, (3) late cocking, (4) acceleration, (5) deceleration, and (6) follow-through
As the elbow extends at over 2,300 °/s, a medial shear force of 300 N and lateral compressive force of 900 N are produced [1, 2]. In addition, the valgus stress applied to the elbow during the acceleration phase of throwing is 64 Nm [1, 2]. The posterior compartment is subject to tensile, compressive, and torsional forces during acceleration and deceleration phases. This valgus stress at the elbow is associated with biomechanical variables: late trunk rotation, reduced shoulder external rotation, reduced total rotation, and increased elbow flexion appear to be overhand pitchers to reduced elbow valgus torque [3, 4]. Another research suggests that the rising incidence of shoulder and elbow injuries in pitchers may not be caused by the curveball mechanics [5]. This mechanism may result in valgus extension overload within the posterior compartment, potentially leading to chondromalacia, osteophytes and loose bodies formation, proximal ulna stress fractures, triceps pathology, or physeal injury (Fig. 16.2).
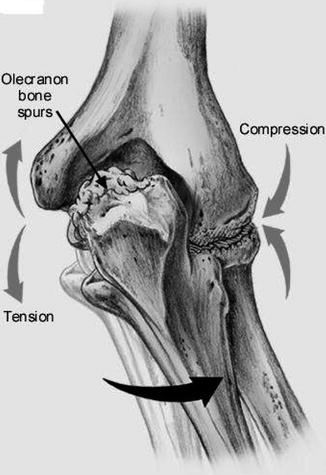
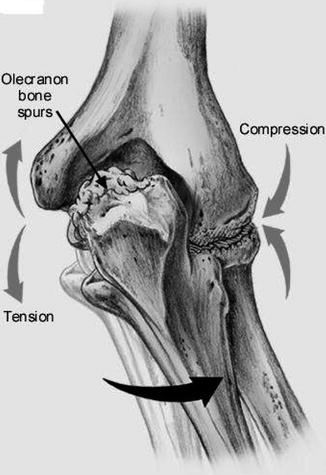
Fig. 16.2
Valgus extension overload within the posterior compartment, potentially leading to chondromalacia, osteophytes and loose bodies formation, proximal ulna stress fractures, triceps pathology, or physeal injury
16.3 History and Physical Examination
Overhead athletes complain of medial/olecranon pain during follow-through phase of throwing. Athletes who have pain during earlier phases of throwing (late cocking) more likely have other pathologies, as ulnar collateral ligament (UCL) insufficiency, posteromedial impingement complaints and loose bodies, or an inability to fully extend the arm due to pain, posterior olecranon/fossa osteophytes, or loose bodies. Checking for factors relating to (changes in) training and performance is mandatory.
Besides the routine elbow physical examination, including determination of the carrying angle of the arm, the valgus extension overload test is valuable (VEOLS). The VEOLS test or valgus extension snap maneuver was first described by Andrews: a moderate valgus stress is applied to the elbow with simultaneous palpation of the posteromedial tip of the olecranon while the elbow is moved from 30° of flexion to full extension. To be noted that valgus laxity has been described in the dominant arm of asymptomatic overhead athletes. It is important to evaluate and document the location and mobility of the ulnar nerve within the cubital tunnel during flexion in all patients undergoing elbow arthroscopy. An arthroscopy should never be performed without knowing the exact location of the ulnar nerve [19]. The examiner should keep in mind that there is a large variation in ROM and carrying angle in the overhead athletes.
16.4 Radiology
Imaging of elbow in overhead athletes should include plain radiographs with anteroposterior and lateral views. An axial oblique view may be helpful to detect osteophytes on the olecranon or on the borders of the posterior fossa, where loose bodies can be identified as well. For this additional view, the elbow should be bent at 110° with the arm on the cassette. The beam should then be angled at 45° toward the ulna. CT scan can be useful for the assessment of osteophytes, stress fractures, avulsion fractures, or loose bodies (Fig. 16.3). In posteromedial impingement the osteophytes are located on the medial side of the olecranon tip and not on both sides and in other locations in the elbow as it happens commonly in osteoarthritis [16]. Magnetic resonance imaging (MRI) with or without intra-articular contrast is considered the gold standard imaging modality for the athlete’s elbow. The sensitivity of the MRI scan for posterior soft tissue or loose bodies is nearly 90 % [13]. MRI findings also show high correlation with arthroscopic evaluation [14].


Fig. 16.3
CT scan can be useful for the assessment of osteophytes, stress fractures, avulsion fractures, or loose bodies
Dynamic ultrasound allows a real-time evaluation of the moving elbow and can help to assess the stability of the UCL and thereby guide in the diagnosis of posteromedial elbow impingement [15].
16.5 Conservative Treatment
Treatment of posteromedial impingement starts with nonoperative measures such as physiotherapy and NSAIDs, in combination with rest, ice, compression, and elevation (RICE). This treatment should also include other joints as the shoulder. Sometimes steroid injections can give some pain relief if there is only soft-tissue impingement. Nonoperative treatment of posteromedial elbow impingement was initially reported in javelin throwers in 1946 by Waris [6]. If conservative treatment fails, arthroscopy of the elbow can then a successful choice.
16.6 Operative Treatment
When performing elbow arthroscopy, we prefer general anesthesia because it allows more comfort for the patient and muscle relaxation, which prevents patient’s movement during surgery (therefore decreasing the risk of nerve injuries) and avoids complications associated with a regional block [20]. We also prefer the lateral decubitus, because it offers increased stability, access to the arm, and unrestricted elbow motion, compared to the supine position [17]. This position is also favorable for the anesthesia. Standard equipment necessary for shoulder and knee arthroscopy can be utilized for elbow arthroscopy. Before starting the arthroscopy, bony landmarks, arthroscopic portals, and location of the ulnar nerve have to be marked on the skin. After inflation of the tourniquet to 250 mmHg, the joint is then injected with physiologic saline from posterior to allow full distension of the capsule [18] and shift the neurovascular structures away from the joint [5]. When the fluid is in the joint, the elbow will extend a little. In case of a posteromedial impingement without loose bodies and without contracture, a posterior arthroscopy can be sufficient to treat this pathology. In case of loose bodies, the anterior compartment should be inspected; even in the case these loose bodies are in the posterior compartment on the CT or MRI scan. Through the postero-central “trans-tricipital” portal and the proximal posterolateral portal, the posterior compartment can be reached and loose bodies can be removed, impinging osteophytes debrided back to a normal olecranon contour, and articular cartilage lesions can be addressed. Capsular contracture may also be addressed with anterior and posterior arthroscopy.
16.7 Results After Treatment
In the literature, there is often ambiguity between posterior and posteromedial impingement and these terms have often been used interchangeably. As such, it is a challenge to tease true cases of [29] posteromedial impingement out of the outcomes data. Fideler and colleagues reported on 113 professional baseball players (97 pitchers) who underwent arthroscopic treatment for posterior impingement of their dominant elbow. Given the demographic data, it is likely that most of these patients were cases of posteromedial impingement. Seventy-four percent of these athletes had good to excellent results, meaning that they were able to return to their sport for a minimum of 24 months. However, motion only objectively improved in 22 % of patients and 10 % required a subsequent UCL reconstruction. Andrews et al. [23] reported on 34 professional baseball players with posteromedial impingement who underwent arthroscopic debridement. They found a 68 % return to play rate, but a 41 % reoperation rate, often for [30] debridement of recurrent osteophytes and/or UCL reconstruction. Reddy and colleagues reported on 172 patients that underwent elbow arthroscopy, 96 of which for posterior impingement. The study population was dominated by baseball players, suggesting again that these were mostly cases of posteromedial impingement. The specific outcomes for the posterior impingement cases were not reported, but overall 56 % of patients had an excellent result and 36 % ended with a good result [31].
Pitfalls of the Treatment
1.




Baseball players who underwent partial olecranon excision for posterior impingement did not have universally excellent results, 42 % of these patients requiring a second operation and several undergoing UCL reconstruction. It cannot be concluded whether removal of the osteophytes and a part of the olecranon uncovered UCL insufficiency or whether this procedure resulted in increased strain on the UCL, making it susceptible to rupture when the athlete returns to throwing [23, 24]. Resection of the olecranon osteophytes may “unmask” subtle UCL insufficiency [25]. We therefore recommend that only the osteophyte and no native olecranon should be removed during arthroscopy [22, 23].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








