Posterior Cervical Foraminotomy
Introduction
Minimally invasive posterior cervical foraminotomy offers alternative to traditional open techniques with similar outcomes
Posterior cervical foraminotomy eliminates risk of injuring carotid artery, esophagus, and recurrent laryngeal nerve associated with anterior approach
Does not require fusion; does not destabilize disk space; easy approach to directly decompress foramen
Limitation is inability to deal directly with pathology affecting central aspect of canal, compared with anterior approach
Posterior procedures require more dissection of extensor spine muscle mass, with possible increase in postoperative neck pain
May modify approach by undercutting spinous process to treat myelopathy; efficacy and safety not demonstrated
Patient Selection
Indications
Patients with persistent radiculopathy that correlates with findings on CT, MRI, or myelography
Failure of nonsurgical management
Refractory radiculopathy after anterior cervical diskectomy and fusion
Cervical radiculopathy due to foraminal stenosis, posterolaterally herniated disks, or persistent symptoms after anterior cervical fusion
Contraindications
Local skin infection
Cervical myelopathy
Significant kyphosis
Mechanical instability of cervical spine
Spinal cord compression
Significant disk herniation compressing the nerve root
Symptomatology not referable to pathology on imaging studies
Preoperative Imaging
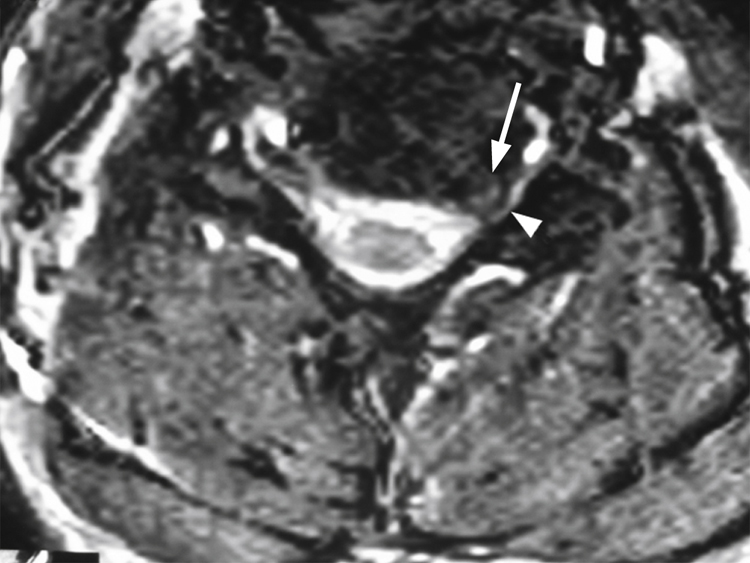
Figure 1T2-weighted axial MRI shows a disk herniation (arrow) in the C5-6 neural foramen compressing the left C5-6 nerve root (arrowhead).
AP and lateral radiographs to assess cervical alignment
Dynamic flexion-extension views to identify instability
MRI to evaluate spinal cord and nerve roots for sites of compression (Figure 1)
If MRI cannot be obtained, CT myelogram is alternative
Procedure
Room Setup/Patient Positioning
Prone or seated position
Apply three-pin Mayfield fixation, fixing head to table in prone position
Place Wilson frame or similar bolsters under torso
Protect and pad all potential neural compression points
Extend neck; avoid hyperextension
Slightly tucking in chin in “military” posture aids in approach
Reverse Trendelenburg position allows venous drainage, less bleeding
Position fluoroscopic C-arm under drapes to visualize retractors during procedure
Tape shoulders down for radiographic visualization of neck
Flex knees to prevent distal migration of patient
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


