(1)
Department of Orthopedic Surgery Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands
Abstract
Posterior ankle impingement is a pain syndrome. It is a clinical diagnosis in which the patient experiences pain in the hindfoot when the ankle is forced into a plantar-flexed position. Surgical treatment involves removal of the impediment like os trigonum, scar tissue, or hypertrophic posterior talar process. The anatomical considerations, etiology, diagnostic processes, and differential diagnosis are described. The operative technique of endoscopic removal of an os trigonum and endoscopic treatment of a posterior talar process and a posterior soft tissue impingement are described in detail. The chapter also contains a section on pitfalls of these procedures.
Posterior ankle impingement is a pain syndrome. The patient has pain in the hindfoot when the ankle is forced into a plantar-flexed position.
The most important mechanical cause of articular posterior ankle pain is the posterior impingement syndrome.
Surgical treatment of a posterior ankle impingement syndrome involves removal of the posterior impediment which can consist of an os trigonum, scar tissue, thickened/ruptured intermalleolar ligament, or hypertrophic posterior talar process.
13.1 Introduction
The most important mechanical cause of articular posterior ankle pain is the posterior impingement syndrome (Van Dijk et al. 2002). Posterior ankle impingement is a pain syndrome. The patient experiences posterior ankle pain which is predominantly present on forced plantar flexion. The syndrome can result from an acute or chronic injury. The presence of an anatomical anomaly such as an os trigonum is often associated with this entity (Fig. 13.1). Overuse injuries associated with posterior impingement often occur in ballet dancing and running, whereas acute symptoms result from a hyperplantarflexion or supination trauma, predominantly in soccer players. In one study posterior impingement caused by overuse seemed to have a better prognosis (Stibbe et al. 1994). An os trigonum is usually not the cause of impingement on its own (Van Dijk et al. 1995). This anatomical anomaly must be combined with a traumatic event such as a supination trauma, dancing on hard surfaces, or pushing beyond anatomical limits to cause pain. The pain is caused by an abnormal movement between the os trigonum and talus or compression of a thickened joint capsule or scar tissue between the os trigonum and the posterior tibial rim (Hedrick and McBryde 1994; Hamilton et al. 1996).
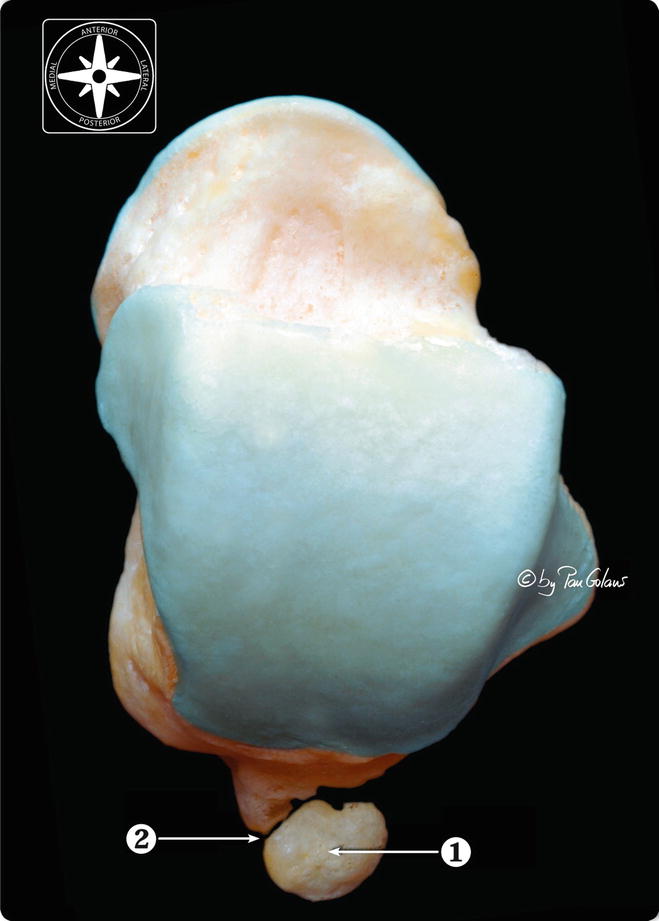
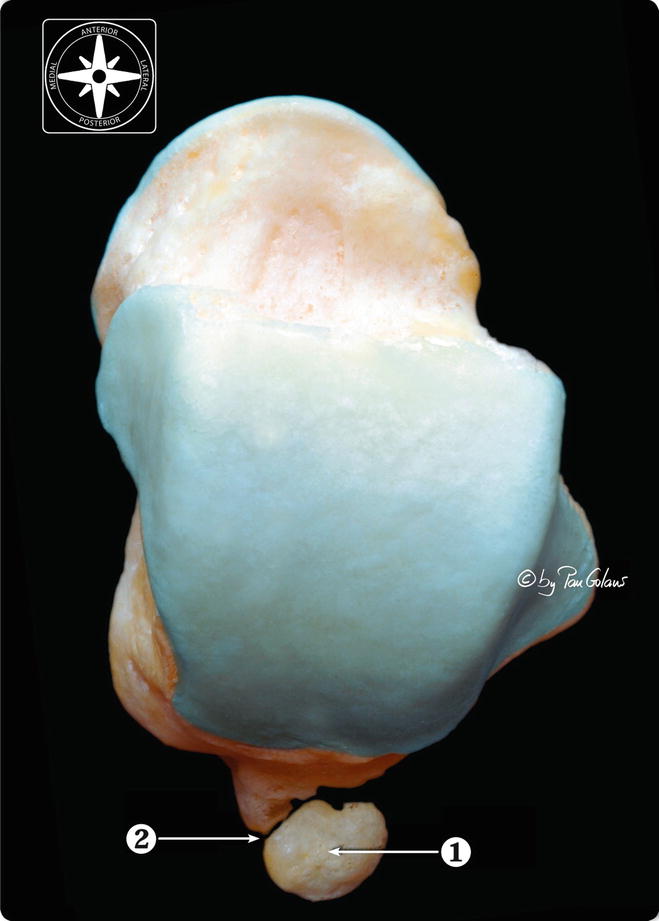
Fig. 13.1
Superior view of the right os talus associated with an accessory bone, the os trigonum. 1 Os trigonum. 2 Fibrous synchondrosis between the ossicle and the talus (With kind permission of © Pau Golanó 2013)
After failure of conservative treatment, posterior intra- and extra-articular ankle pathology demands for open surgery. Open surgery may require postoperative plaster immobilization to prevent equinus malformation and to stimulate wound healing (Lapidus 1972; Richardson 1992). The incidence of complications associated with open surgery has been reported to be 13–24 % (Hamilton et al. 1996; Marotta and Micheli 1992; Abramowitz et al. 2003). A -portal posterior endoscopic ankle approach (hindfoot endoscopy) with the patient in the prone position has demonstrated to offer excellent access to the posterior compartment of the ankle joint, the posterior subtalar joint, as well as the flexor hallucis longus tendon and os trigonum (Van Dijk et al. 2000). Hindfoot endoscopy is performed in an outpatient setting, followed by functional postoperative treatment. It offers the advantages of less morbidity and reduction in postoperative pain when compared to open surgery (Van Dijk 2000). The safety of the procedure was confirmed in two cadaver studies by Sitler et al. (2002) and Lijio et al. (2003).
We enrolled 57 patients with endoscopic treatment of a posterior ankle impingement syndrome in a prospective protocol. Our primary hypothesis was that endoscopic surgery would be associated with less morbidity and faster recovery time when compared to open surgery. In addition, differences in functional outcome between patients who suffered from impingement caused by either overuse or trauma and between patients who suffered from either bony or soft tissue impingement were investigated.
13.2 Anatomy
The talus has no muscular insertions. Any movement of the talus in relation to the tibia is realized by passive transmission of motion by means of the ligamentous guiding system (Van Dijk 1994). Active motion is realized by the long foot muscles, which insert onto the midtarsal and metatarsal bones. The posterior joint capsule envelops the posterior joint space. It is attached to the posterior surface of the tibia and to the talus at the border between bone and cartilage. The outer fibrous layer of the capsule is continuous with the fibrous layer of the periosteum. The posterior capsule is lax in plantar flexion and tight in dorsiflexion (Van den Bekerom et al. 2008). The posterior talofibular ligament (PTFL) passes almost horizontal from a groove at the inside of the posterior margin of the lateral malleolus to the posterior prominence of the talus. Frequently, a separate bundle of fibers originates from the same groove on the inside of the posterior part of the lateral malleolus and runs below the posterior tibiofibular ligament to the posterior surface of the tibia (Ludolph and Hierholzer 1986). Both structures are incorporated in the joint capsule (De Leeuw et al. 2010). In plantar flexion and neutral position, the ligament is relaxed, while in dorsiflexion the ligament is tensed. The posterior tibiofibular ligament is a flat fibrous band, with the distal fibers being the longest. The fibers originate from the posterior tubercle of the tibia and run at an approximate angle of 45° distally and laterally, where they attach to the posterior aspect of the fibula. Sometimes the ligament consists of a double structure. The proximal part crosses directly from the tibia to the posterior part of the fibula, whereas the distal section is part of the joint capsule and runs to a groove on the inner side of the posterior margin of the lateral malleolus. It can be recognized as a ligament structure when observing the posterior joint capsule from the inside of the joint as is done in arthroscopy (Van Dijk 1990).
The most prominent posterior part of the talus is located posterolateral. Apart from the posterior joint capsule, the posterior talofibular ligament attaches to this posterior talar process. Medial from this prominent bony process is the flexor hallucis longus. The flexor hallucis longus tendon thus separates the posterior talar process from the medial talar tubercle. The posterior talar process forms the roof of the posterior facet of the subtalar joint. Embryological, the body of the talus and posterior talar process are separate ossification centers. The posterior talar process appears as a separate ossicle, which is called “os trigonum,” between the 8th and 10th years of life. The body of the talus is usually visible on radiographs around 7 months. The os trigonum may be considered as a secondary ossification center, similar to the calcaneal apophysis. The os trigonum usually fuses with the talus within a year of its appearance. In about 7 % of the normal adult population, however, it is still present as an accessory bone (Salyers and Fu 1989). It can be present bilaterally or unilaterally.
13.3 Etiology
Posterior ankle impingement can be caused by overuse or trauma. It is important to distinguish between these two, because posterior impingement resulting from overuse has a better prognosis (Stibbe et al. 1994).
13.3.1 Overuse
A posterior ankle impingement syndrome resulting from overuse is mainly found in ballet dancers and runners (Van Dijk 1990; Hamilton et al. 1996; Hedrick and McBryde 1994). Running that involves forced plantar flexion, such as downhill running, can put repetitive stress on the posterior aspect of the ankle joint (Van Dijk et al. 1995). The forceful plantar flexion that occurs during the “en pointe” position or the “demi-pointe” position produces compression at the posterior aspect of the ankle joint (Fig. 13.2). Either of these situations can put extreme pressure on the anatomical structures that are normally present between the calcaneus and the posterior part of the distal tibia (Fig. 13.3). Through exercise, the joint mobility and range of motion in the joint gradually increase, reducing the distance between the calcaneus and the posterior part of the distal tibia still further. Thus, if abnormal structures, such as an os trigonum, a hypertrophic posterior talar process, a thickened posterior joint capsule, a posttraumatic scar tissue, posttraumatic calcifications of the posterior joint capsule, a loose body in the posterior part of the ankle joint, or an osteophyte of the posterior distal tibia, are present in this region, they may be compressed.
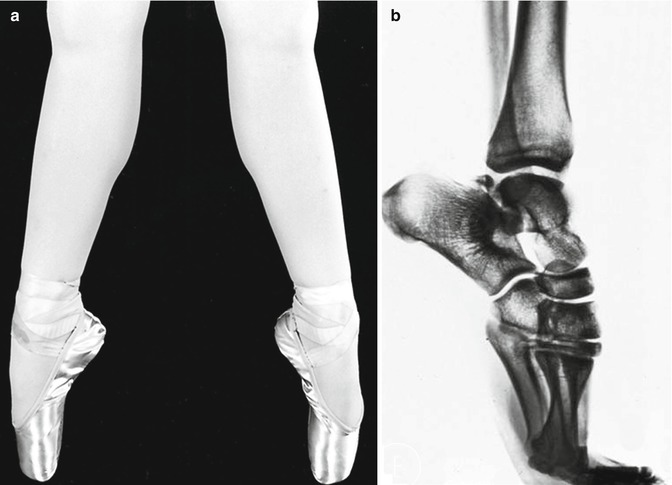
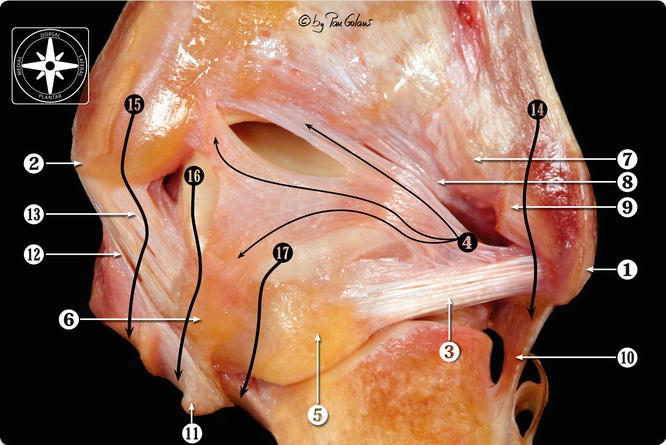
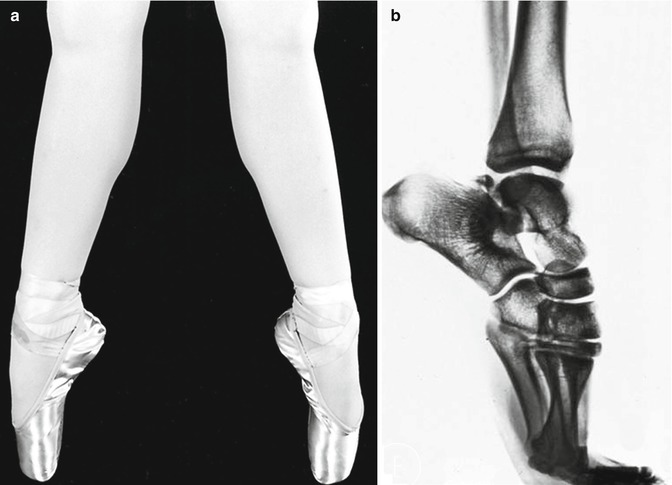
Fig. 13.2
The forceful plantar flexion during the “demi-pointe” position (a) produces compression at the posterior aspect of the ankle joint. Through exercise, the joint mobility and range of motion in ballet dancers gradually increase. In the presence of a prominent posterior talar process or an os trigonum, this can lead to compression of the posterior located structures (b)
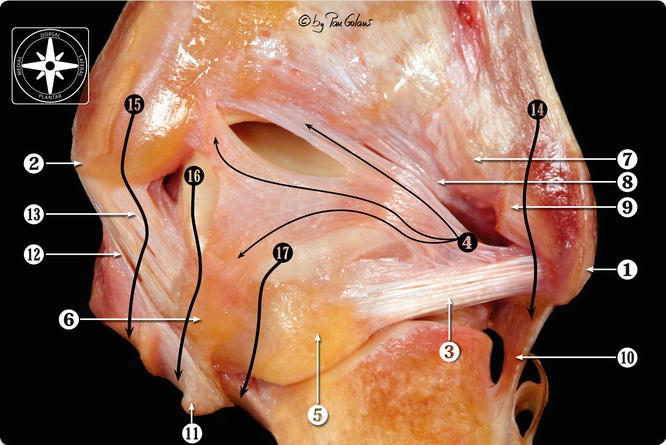
Fig. 13.3
Posterior view of osteoarticular dissection of the ankle. 1 Lateral malleolus. 2 Medial malleolus. 3 Posterior talofibular ligament. 4 Posterior intermalleolar ligament. 5 Lateral talar process. 6 Medial talar process. 7 Superficial component of the posterior tibiofibular ligament. 8 Deep component of the posterior tibiofibular ligament or transverse ligament. 9 Insertion of the fibulotalocalcaneal or Rouvière-Canela ligament (cut). 10 Calcaneofibular ligament. 11 Sustentaculum talk. 12 Superficial layer of the medial collateral ligament. 13 Deep layer of the medial collateral ligament (deep posterior tibiotalar ligament). 14 Peroneal tendons path. 15 Tibialis posterior tendon path. 16 Flexor digitorum longus tendon path. 17 Flexor hallucis longus tendon path. (With kind permission of © Pau Golanó 2013)
A prominent posterior talar process or os trigonum is not sufficient to produce the syndrome. In 1995 we reported on a group of 19 retired dancers and examined their ankle and subtalar joints (Van Dijk et al. 1995). The mean length of the ballet dancers’ professional careers was 37 years. All of the dancers had been dancing “on pointe.” The mean dance time per week was 45 h. The mean age of the dancers was 59 years (range 50–66). None of the ballet dancers had been free from injuries, but no macrotrauma had occurred. None of the dancers had experienced a posterior ankle impingement syndrome. In 18 of the 38 investigated ankle joints, a hypertrophic posterior talar process or an os trigonum was present. In most cases, the os trigonum was relatively large (Van Dijk et al. 1995). We concluded that the presence of an os trigonum or prominent talar process does not seem to be relevant. This anatomical anomaly must be combined with a traumatic event such as supination trauma, dancing on hard surfaces, or pushing beyond anatomical limits. The pain is caused by an abnormal movement between the os trigonum and talus, compression of thickened joint capsules or scar tissue between the os trigonum and tibia, or compression between os trigonum and calcaneus (known as “dancers’ heel”). A thickened or avulsed posterior intermalleolar ligament can also act as a posterior impediment.
13.3.2 Trauma
Forced plantar flexion causes compression of the posterior talar prominence between the tibia and calcaneus. In the presence of an os trigonum, this can lead to a displacement of the os trigonum (Fig. 13.4). In the case of a prominent posterior talar process, a fracture can occur. Compression of the posterior joint capsule can lead to local thickening or calcification. Combined supination and plantar flexion (leading to a lateral ankle ligament lesion) in some patients also leads to compression of posteromedial joint structures. The posttraumatic calcifications in these cases most often are located posteromedial (Fig. 13.5). Hyperplantarflexion can result from an automobile or motorcycle accident, but can also result from sporting activities such as soccer.
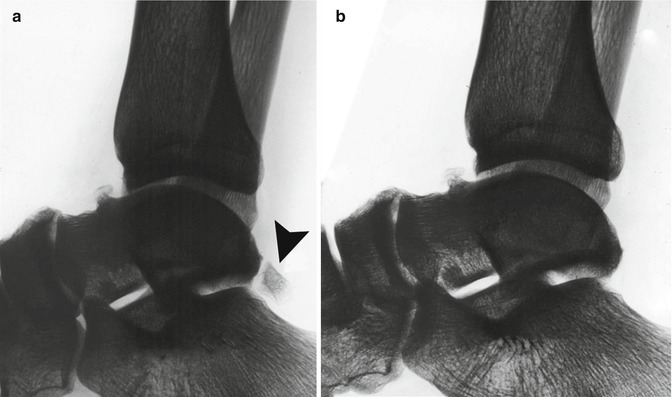
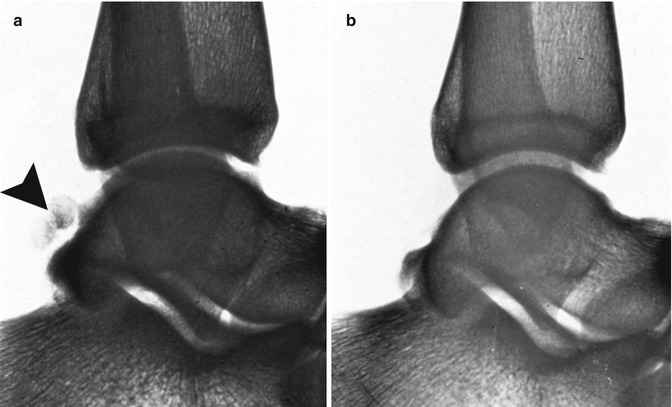
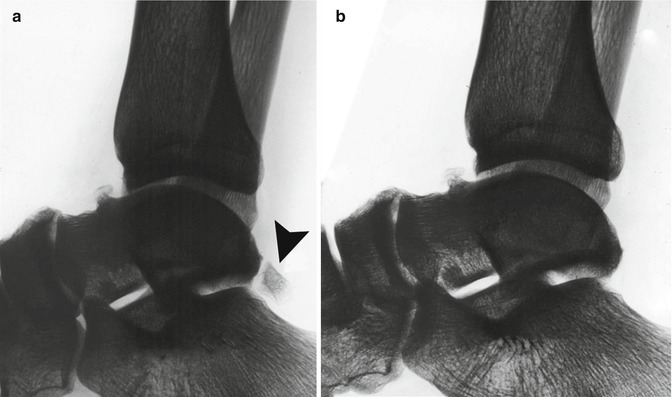
Fig. 13.4
A 27-year-old man who developed a posterior impingement syndrome of the left ankle after a hyperplantarflexion trauma 2 years before lateral X-ray which shows slightly displaced os trigonum (arrowhead) (a). (b) Situation after resection of the os trigonum. The patient became symptom-free
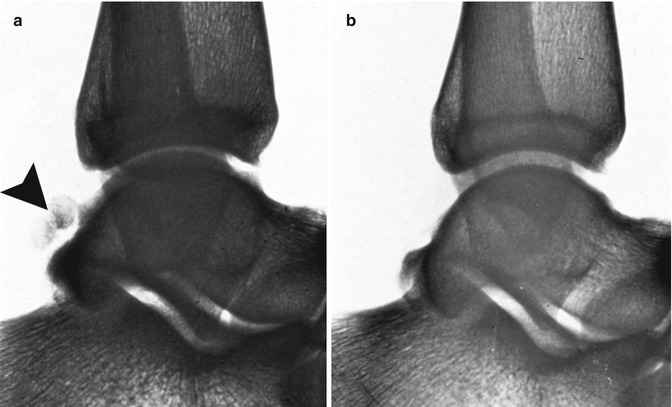
Fig. 13.5
A 25-year-old volleyball player with a supination plantar flexion trauma resulting in a lateral ligament rupture. After functional tape treatment, the patient developed a posterior impingement syndrome with painful, restricted plantar flexion. The radiograph (b) 3 months after trauma, apart from a small calcification, does not show an abnormality. Because of persisting symptoms 1 year postoperative, a bone scan was made. This bone scan showed a posteromedial hot spot. A new radiograph was made, which showed posterior calcifications (arrowhead) (a). The calcifications were removed
13.4 Diagnosis
A diagnosis or differential diagnosis can be made on the basis of the patient’s history, physical examination, and radiographs.
13.4.1 History
Posterior ankle impingement syndrome is a pain syndrome. The patient experiences pain on the posterior aspect of the ankle joint. This pain is mainly present on forced plantar flexion. In some patients, forced dorsiflexion is also painful. In this dorsiflexed position, traction is applied to the posterior joint capsule and posterior talofibular ligament, which both attach to the posterior talar process.
13.4.2 Physical Examination
On examination, there is pain on palpation of the posterior aspect of the talus. This posterior talar process can best be palpated posterolateral in between the peroneal tendons and the Achilles tendon. Posteromedial, the neurovascular bundle and flexor tendons are covering the talus (Fig. 13.6). Posteromedial pain on palpation therefore does not automatically mean impingement pain. The passive forced plantar flexion test is the most important test (Fig. 13.7). The test should be performed with repetitive quick passive hyperplantarflexion movements in a neutral position. The test can be repeated in slight exorotation or slight endorotation of the foot relative to the tibia. The investigator can apply this rotation movement on the point of maximal plantar flexion, thereby “grinding” the posterior talar process/os trigonum between the tibia and calcaneus. A negative test rules out a posterior impingement syndrome. A positive test in combination with pain on posterolateral palpation should be followed by a diagnostic infiltration. The infiltration is performed from the posterolateral side, so that the capsule between the prominent posterior talar process and posterior edge of the tibia is infiltrated with Xylocaine. If the pain on forced plantar flexion disappears, the diagnosis is confirmed.
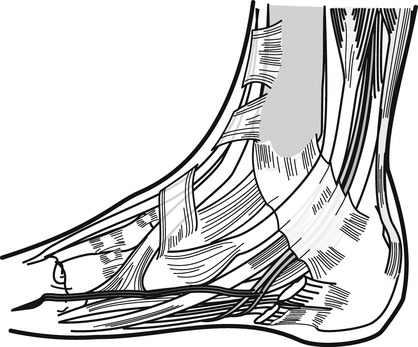
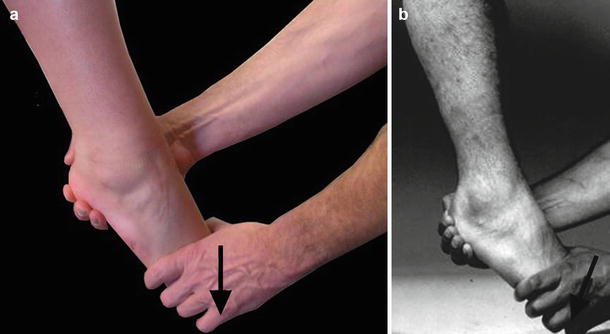
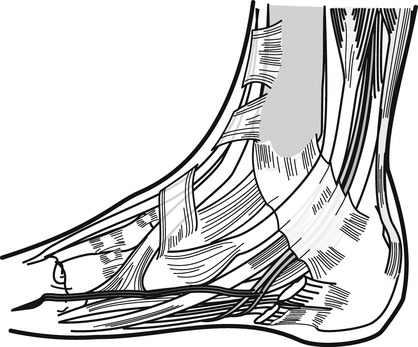
Fig. 13.6
Posteromedial structures: neurovascular bundle (NTP), posterior tibial tendon (TP), flexor digitorum longus tendon (FDL), and flexor hallucis longus tendon (FHL) are covering the talus. Together with the retinaculum (RF), it is not possible to exclusively palpate the posterior aspect of the talus from the medial side
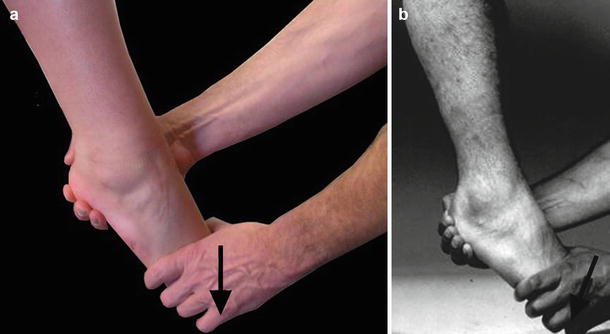
Fig. 13.7
The passive forced plantar flexion test. The test is performed with repetitive quick passive short hyperplantarflexion movements. The foot can be in relative endorotation, neutral position, or slight exorotation at the moment of maximal plantar flexion impaction. At the point of maximal plantar flexion, the investigator can apply this rotation movement, thereby “grinding” the posterior talar process/os trigonum between the tibia and calcaneus (a, b)
13.4.3 Diagnostic Imaging
The AP ankle view typically does not show abnormalities. On the lateral view, often a prominent posterior talar process or os trigonum can be recognized. In posttraumatic cases, we look for signs of nonunion in this area. The posterior talar process or os trigonum is located posterolateral. On the lateral view this posterolateral part is often superpositioned onto the medial talar tubercle (Fig.13.8). Detection of a nonunion on a standard lateral view, therefore, is often difficult. Calcifications, for the same reason, sometimes cannot be detected by this standard lateral view. In posttraumatic cases, therefore, a bone scan can be performed if the radiograph does not show abnormalities (Fig. 13.9). A positive bone scan can be followed by CT scan. Especially in posttraumatic cases, a CT scan is important in order to determine the extent of injury and the exact location of calcification or fragments.
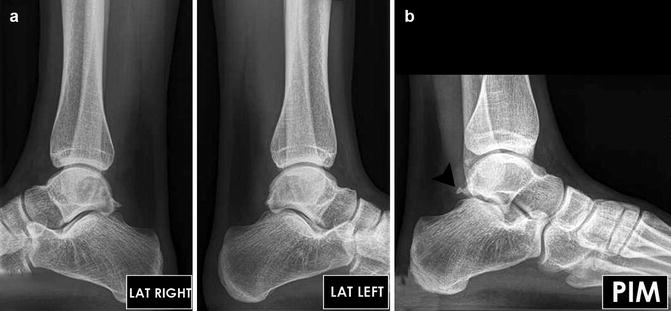
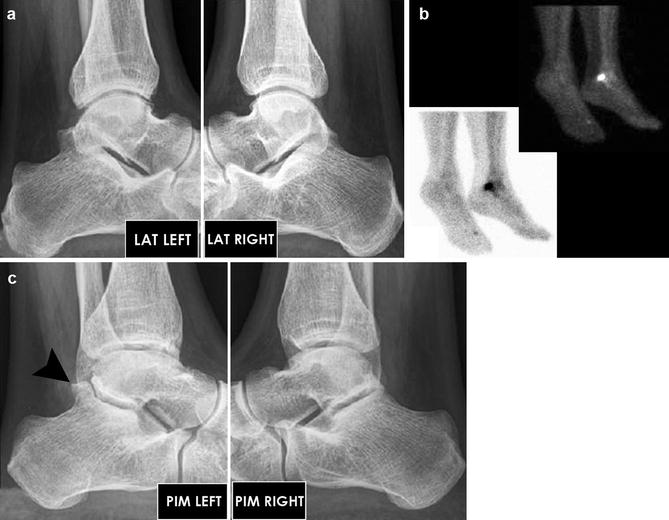
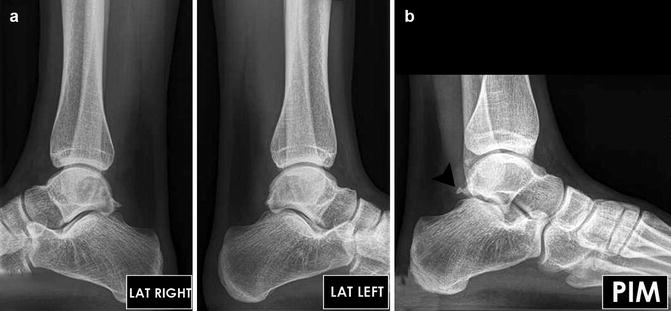
Fig. 13.8
A 24-year-old professional soccer player with persisting complaints 6 months after hyperplantarflexion trauma on the left ankle. On the lateral radiograph (a), no pathology was recognized (the right ankle shows a small posterior talar spur). The PIM view (b) of the left ankle now shows a small os trigonum (arrowhead)
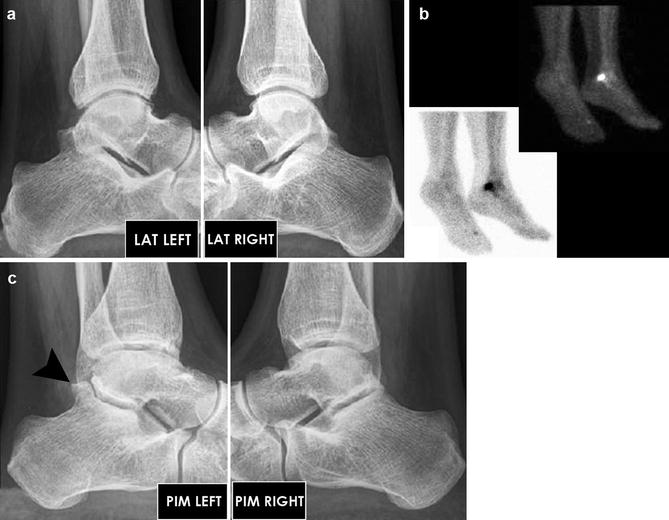
Fig. 13.9
Lateral view (a) of a 36-year-old man who developed a posterior ankle impingement syndrome after a hyperplantarflexion trauma of the left ankle. The radiographs do not show any abnormality (a). The technetium scan (b) shows a hot spot in the posterior aspect of the ankle joint. The PIM view (c) shows a slightly displaced os trigonum (arrowhead) of the left ankle
13.5 Differential Diagnosis
In the differential diagnosis, the following diagnoses are considered:
1.
Posterior rim pathology
2.
Osteochondral defect in the most posterior part of the ankle joint (tibial plafond or posterior talar dome)
3.
Chondromatosis
4.
Loose body in the posterior ankle compartment
5.
Tendinitis flexor hallucis longus
6.
Tarsal tunnel syndrome
7.
Subtalar pathology
Conditions such as posterior tibial tendinitis, chronic synovitis of the ankle joint, posterior osteochondral defect, or osteoid osteoma usually have a different clinical presentation (Van Dijk 1990; Van Dijk and Scholte 1997). A loose body in the posterior ankle joint can clinically present as posterior ankle impingement. Flexor hallucis longus tendinitis in ballet dancers is most important in the differential diagnosis. The pain is located posteromedial. It is present in “plié” and especially in “grand plié.” The flexor hallucis longus tendon can be palpated behind the medial malleolus. By asking the patient to repetitively flex the toes with the ankle in 10°–20° of plantar flexion, the flexor hallucis longus tendon can be palpated in its gliding channel behind the medial malleolus. The tendon glides up and down under the palpating finger of the examiner. In case of stenosing tendinitis or chronic inflammation, we feel for crepitus and pain, while sometimes a nodule in the tendon can be felt to move up and down under the palpating finger. Subtalar pathology of the posteromedial compartment is called “dancers’ heel” (Van Dijk et al. 2001). The movement in the subtalar joint is a “gliding” and rotating movement. Even though there is little movement of the subtalar joint surfaces in relation to each other, a statistically significant increase in degenerative subtalar joint disease in retired professional female ballet dancers compared with a matched-paired control group was found (Van Dijk et al. 1995). The “dancers’ heel” can be subdivided into three stages.
Stage 1: Chondropathy without radiographic changes
Stage 2: Subchondral changes, osteophytes, no joint space narrowing
Stage 3: Joint space narrowing
Because of the close relationship between the structures located in the tarsal tunnel and the posteromedial aspect of the subtalar joint, the dancers’ heel can give rise to secondary tendon pathology.
13.6 Therapy
Nonoperative treatment involves modification of activities, physical therapy (massage, stretching, and muscle strengthening), icing, use of nonsteroidal anti-inflammatory medication, and injection of steroids. The steroids are injected posterolateral into the posterior joint capsule between the prominent posterior tibial talar process and the posterior tibial edge. Physicians who are not familiar with the local anatomy are advised to perform the infiltration under fluoroscopic control. Analysis and correction of the patient’s dance technique involves correction of sickling. Sickling in valgus is the result of hypertonic peroneal muscles and relative weakness of the posterior tibial tendon. Sickling in varus can be the result of a weakness of the peroneal muscles. Operative treatment involves the removal of a hypertrophic posterior joint capsule, an os trigonum, a hypertrophic posterior talar process, a pseudarthrotic fragment, calcifications, osteophytes, or loose bodies (Fig. 13.10).


Fig. 13.10




(a) AP and lateral views of a 50-year-old man showing no abnormality. Fifteen years before he sustained a hyperplantarflexion trauma. Current symptom is posterior ankle pain on walking long distance. Pain more prominent walking downhill. On investigation recognizable pain on the hyperplantarflexion test. PIM view shows os trigonum (arrowhead) (b) which is confirmed by CT scan (c)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








