Fig. 17.1
Depending on the talar location of the osteochondral defect, the pathology can be addressed via anterior or posterior ankle arthroscopy. To determine whether the osteochondral defect can be approached via anterior ankle arthroscopy, the foot is forced in maximum plantarflexion. (a) Posteriorly located talar osteochondral defect with the foot in neutral position. (b) By forcing the foot in maximum plantar flexion, the osteochondral defect moves anteriorly. In this case, the osteochondral defect cannot be reached via anterior ankle arthroscopy but can be reached via posterior ankle arthroscopy
17.3.2 Posterior Compartment Subtalar Joint
17.4 Periarticular Pathology
17.4.1 Posterior Ankle Impingement
Posterior ankle impingement syndrome is by definition a pain syndrome. The pain is present in the hindfoot during forced plantar flexion. The patients can be divided into an overuse and a trauma group based on the mechanism to produce this syndrome.
The overuse group is mainly composed of ballet dancers, downhill runners, and soccer players.18–20 In professional ballet, the specific dancing steps force the ankle in hyper-plantar-flexion. The anatomic structures in between the calcaneus and the posterior part of the distal tibia thereby become compressed. Through exercise, the dancer will attempt to increase the range of motion and joint mobility, ultimately decreasing the distance between the calcaneus and the talus. The anatomical structures at the back of the ankle joint hereby can become compressed. During downhill running, the ankle is repetitively forced into plantar flexion, resulting in repetitive stress on the anatomical structures in this posterior area.21 Kicking the ball with the foot in plantar flexion results in high forces on the anatomical structures in the hindfoot. These repetitive high forces can eventually cause posterior ankle impingement.
A hyper-plantar-flexion trauma and supination trauma can cause damage to the anatomical structures in the hindfoot and can finally lead to a chronic posterior ankle impingement syndrome.
A differentiation must be made between the two groups, since overuse trauma seems to have a better prognosis22 and patients are more satisfied after arthroscopic treatment.22 Congenital anatomic anomalies such as a prominent posterior talar process, an os trigonum, or a talus bipartitus23 can facilitate the occurrence of the syndrome. An os trigonum is estimated to be present in 1.7–7% and occurs bilateral in 1.4% people.24–26 These congenital anomalies in combination with a traumatic or overuse injury facilitate the occurrence of symptoms.20,27–29 During plantar flexion, the soft tissue structures like synovium, posterior ankle capsule, or one of the posterior ligamentous structures can get pinched and compressed, eventually resulting in swelling, partial rupture, or fibrosis.
The diagnosis is clinical. The forced passive hyper-plantar-flexion test is positive when the patient experiences recognizable pain during the test (Fig. 17.2). A negative test rules out the posterior ankle impingement syndrome. A positive test is followed by a diagnostic infiltration with Xylocaine® (AstraZenica, Zoetermeer, The Netherlands) in the posterior ankle compartment. Disappearance of pain following infiltration confirms the diagnosis.


Fig. 17.2
The forced hyper-plantar-flexion test is performed with the patient sitting with the knee flexed in 90°. The test should be performed with repetitive quick passive hyper-plantar-flexion movements. The test can be repeated in slight external rotation or slight internal rotation of the foot relative to the tibia. The investigator can apply this rotational movement on the point of maximal plantar flexion, thereby “grinding” the (enlarged) posterior talar process/os trigonum in between tibia and calcaneus
17.4.2 Deep Portion of the Deltoid Ligament/Cedell Fracture
Hyper-dorsiflexion or eversion trauma can result in avulsed fragments, posttraumatic calcifications, or ossicles in the deep portion of the deltoid ligament. The patient typically presents with posteromedial ankle pain, which is aggravated by running and walking on uneven grounds. Ligament avulsion of the deep portion of the deltoid ligament from the posteromedial talar process was first described by Cedell.30 A computed tomography (CT) scan is most often necessary to confirm the diagnosis.
17.4.3 Flexor Hallucis Longus
Posterior ankle impingement syndrome is often accompanied by tendinopathy of the flexor hallucis longus (FHL). The patient experiences posteromedial ankle pain. On physical examination, the tendon can be palpated behind the medial malleolus, just lateral to the flexor digitorum longus. By asking the patient to repetitively flex the big toe, the FHL tendon can easily be identified in between the medial and lateral talar processes while the ankle is in 10–20° plantar flexion. In patients with tendinopathy or paratendinopathy, crepitus and recognizable tenderness can be provoked by the examiner’s finger placed over the tendon just behind the medial malleolus. In some patients, a painful nodule in the tendon can be palpated.
17.4.4 Achilles Tendon and Retrocalcaneal Bursa
A symptomatic inflammation of the retrocalcaneal bursa is caused by repetitive impingement of the bursa between the anterior aspect of the Achilles tendon and a bony postero-superior calcaneal prominence. A prominent postero-superior calcaneal rim in combination with retrocalcaneal bursitis was first described by Haglund in 1928.31 Physical examination reveals swelling on both sides of the Achilles tendon at the level of the postero-superior calcaneal prominence. Pain is aggravated by palpating this area just medial and lateral to the Achilles tendon.
Retrocalcaneal bursitis can be accompanied by midportion and/or insertional tendinopathy. In case of insertional tendinopathy, there is pain at the bone–tendon junction, which gets worse after exercise. The area of maximal tenderness is often located in the central part of the insertion. Patients with tendinopathy of the main body of the Achilles tendon report pain and stiffness. A thick nodule is present 2–6 cm proximal to the insertion, which is tender on palpation.
17.4.5 Neurovascular Bundle
Entrapment of the posterior tibial nerve within the tarsal tunnel is commonly known as a tarsal tunnel syndrome.32 Clinical examination should be sufficient to differentiate these disorders from an isolated posterior tibial tendon disorder.
17.4.6 Peroneal Tendons
Peroneal tendon disorders are an uncommon, under-recognized source of posterolateral hindfoot pain and dysfunction. Pathology of the peroneal tendons is often overlooked because it is sometimes difficult to distinguish them from lateral ankle ligament disorders.33
Instability and dislocation are pathologies associated with the peroneal tendons and are often provoked by sports-related injuries. In 1803, Monteggia was the first describing peroneal instability in a ballet dancer.34 There are two factors which can cause the tendons to dislocate. First, the superior peroneal tendon retinaculum can be too lax or disrupted.35–37 The retinaculum normally tightly covers the peroneal tendons at the posterior distal fibula, maintaining the tendons at their anatomical site. In case of trauma, this function can be impaired. The second mechanism is a (congenital) flat/non-concave configuration of the posterior distal part of the fibula,38,39 with or without an inadequate amount of cartilaginous rim.36 In the normal situation, this part of the fibula is concave with a cartilaginous rim at the most distal part, nurturing the peroneal tendons behind the lateral malleolus. Superior peroneal retinacular dysfunction and an inadequate fibular groove often coexist in recurrent peroneal tendon dislocation.
Patients typically complain of a recurrent painful and snapping sensation at the lateral aspect of the ankle with a perception of ankle instability, especially when walking on uneven ground. The pain and dislocation can be provoked by combined dorsiflexion and eversion of the foot during physical examination.
17.5 Preoperative Planning
After history taking and physical examination, the diagnosis can be confirmed or rejected based upon different available imaging techniques. If history taking and the physical examination do not reveal abnormalities, additional diagnostics can be used to search for a clue or to rule out pathology, i.e., medico-legal reasons. Close consultation between the surgeon and the radiologist is necessary to decide upon optimal radiographic diagnostics.40
Always start with routine weight-bearing radiographs in an anteroposterior (AP) and lateral direction. In patients with an osteochondral defect, the standard weight-bearing radiographs may show an area of detached bone, surrounded by radiolucency. Initially the defect might be too small to be visualized. A heel rise mortise view may reveal a posteriorly located osteochondral defect.41 For further diagnostic evaluation, CT and magnetic resonance imaging (MRI) have demonstrated similar accuracy.41 A multi-slice helical CT scan is preferred to determine the extent of the defect and also to decide upon anterior or posterior arthroscopic approach for debridement and bone marrow stimulation.41
In patients with a posterior ankle impingement, the AP ankle view typically does not show abnormalities. Osteophytes, calcifications, loose bodies, chondromatosis as well as hypertrophy of the postero-superior calcaneal border can often be detected by the lateral ankle radiograph. In case of doubt for the differentiation between hypertrophy of the posterior talar process or an os trigonum, we recommend a lateral radiograph view with the foot in 25° external rotation in relation to the standard ankle view (Fig. 17.3). Especially in posttraumatic cases, a spiral CT scan can be important to ascertain the extent of the injury and the exact location of calcifications or fragments. In general, soft tissue pathology consequently can be visualized best using a MRI scan. Ultrasonography seems to be a good and relatively cheap alternative, with a positive predictive value of 100% for peroneal tendon dislocation.42,43


Fig. 17.3
A 27-year-old male patient presenting with posterior left ankle pain during plantarflexed movement of the foot. Hyper-plantar-flexion test is positive. (Left) The standard lateral radiograph shows a possible prominent posterior talar process (arrow). (Right) Lateral X-ray with the foot in 25° exorotation. An os trigonum can be recognized (arrow)
17.6 Operative Techniques
17.6.1 Posterior Ankle Arthroscopy
The procedure is carried out in an outpatient setting under general anesthesia or spinal anesthesia. The patient is placed in a prone position. The involved leg is marked by the patient with an arrow to avoid wrong side surgery, with a tourniquet inflated around the thigh, pressured 300 mmHg. A small support is placed under the lower leg, making it possible to move the ankle freely (Fig. 17.4). We use a soft tissue distraction device when indicated.44


Fig. 17.4
For posterior ankle arthroscopy, the patient is placed in a prone position. A tourniquet is applied around the upper leg and a small support is placed under the lower leg, making it possible to move the ankle freely
For irrigation, normal saline is used, but Ringers solution is also possible. A 4.0-mm arthroscope with an inclination angle of 30° is routinely used for posterior ankle arthroscopy. Apart from the standard excisional and motorized instruments for treatment of osteophytes and ossicles, a 4-mm chisel and periosteal elevator can be useful.
The anatomical landmarks on the posterior ankle are the lateral malleolus, medial and lateral border of the Achilles tendon, and the foot sole. The ankle is kept in a neutral position. A straight line is drawn from the tip of the lateral malleolus to the Achilles tendon, parallel to the foot sole (Fig. 17.5).


Fig. 17.5
For marking the anatomical landmarks that are needed for portal placement, the ankle is kept in a neutral position. A hook can be useful to determine the plane in which the portal must be positioned. A straight line is drawn from the tip of the lateral malleolus to the Achilles tendon, parallel to the foot sole. The posterolateral portal (arrow) is made just above the line from the tip of the lateral malleolus to the interception with the Achilles tendon
The posterolateral portal is made directly in front of the Achilles tendon just proximal to this line. After making a vertical stab incision, the subcutaneous layer is split by a mosquito clamp. The mosquito clamp is directed anteriorly, pointing toward the interdigital webspace, in between the first and second toes (Fig. 17.6a). When the tip of the clamp touches the bone, it is exchanged for a 4.5-mm arthroscopic shaft with the blunt trocar pointing in the same direction (Fig. 17.6b). By palpating the bone in the sagittal plane, the level of the ankle joint and subtalar joint can often be distinguished since the prominent posterior talar process or os trigonum can be felt as a posterior prominence in between the two joints. The trocar is situated extra-articularly at the level of the ankle joint. The trocar is exchanged for the 4-mm arthroscope with the direction of view 30° to the lateral side.
Fig. 17.6
Macroscopic image of a right ankle indicating the stepwise portal placement for hindfoot endoscopy. (a) After making a vertical stab incision, the subcutaneous tissue is bluntly divided by a mosquito clamp in the direction of the first interdigital webspace. (b) The mosquito clamp is exchanged for the blunt trocar, still the direction is toward the interdigital webspace. (c) After the medial portal has been created, a mosquito clamp is introduced, directed toward the arthroscopic shaft in a 90° angle. (d) The arthroscopic shaft is used as a guide to travel anteriorly with the mosquito clamp toward the bone. (e) The arthroscope is slightly pulled back until the clamp comes into view
The posteromedial portal is made at the same level, just above the line from the tip of the lateral malleolus, but just in front of the medial aspect of the Achilles tendon (Fig. 17.7). After making a vertical stab incision, a mosquito clamp is introduced and directed toward the arthroscope shaft in a 90° angle (Fig. 17.6c). When the mosquito clamp touches the shaft of the arthroscope, the shaft is used as a guide to “travel” anteriorly in the direction of the ankle joint, all the way down while contacting the arthroscope shaft until it reaches the bone (Fig. 17.6d). The arthroscope is now pulled slightly backward and slides over the mosquito clamp until the tip of the mosquito clamp comes into view (Fig. 17.6e). The clamp is used to spread the extra-articular soft tissue in front of the tip of the lens. In situations where scar tissue or adhesions are present, the mosquito clamp is exchanged for a 5-mm full radius shaver. The tip of the shaver is directed in a lateral and slightly plantar direction toward the lateral aspect of the subtalar joint.
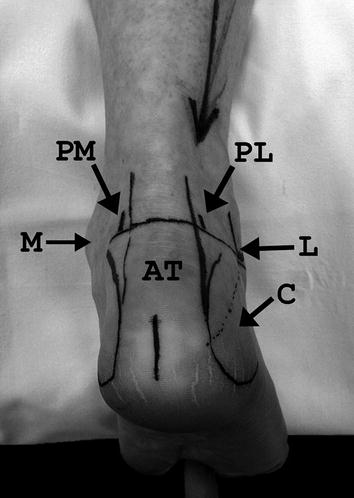
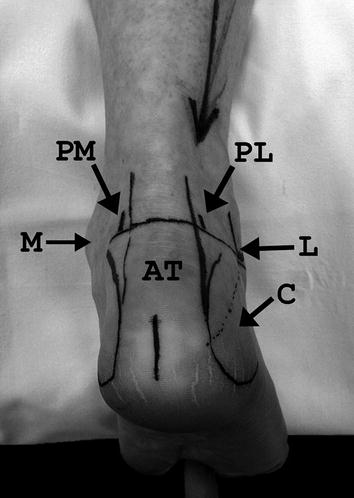
Fig. 17.7




The anatomical landmarks for posterior ankle arthroscopy are marked on a left ankle. The posterolateral portal (PL) is made just above a horizontal line drawn from the tip of the lateral malleolus (L) to the Achilles tendon (AT), parallel to the foot sole with the foot in the neutral position. The posteromedial portal (PM) is created at the same level, just medial to the Achilles tendon. M medial malleolus, C calcaneus)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








