Fig. 12.1
Functional classification of nervous injuries
This classification was first made by Seddon in 1943 and includes three types of nervous injuries: neurapraxia, axonotmesis and neurotmesis. Sunderland then added two other stages:
1.
Neurapraxia or Sunderland’s first stage: damage of the myelin but preservation of the axonal continuity. There’s usually a full recovery in 3–12 weeks.
2.
Axonotmesis or Sunderland’s second stage: damage of the fascicle, but conservation of the endoneurial tubes. Therefore, there’s usually a full recovery except if the denervation lasts too long and causes irreversible damages in the motor plate or the sensorial receptors. The volar plate stays functional during approximately a year; the sensorial receptors can survive several years.
3.
Stage 3 with damage of the endoneurial tubes but preservation of the perineurium. The axon is damaged and the prognosis uncertain.
4.
Stage 4 with damage of the perineurium but preservation of the epineurium. The continuity of the nerve is only due to the epineurium. Surgery is necessary to have any hope of recovery.
5.
Neurotmesis or Sunderland’s fifth stage: total rupture of the nerve, there isn’t continuity anymore and surgery is needed.
12.3 Sensorial Physiology [11]
The sensitivity of the hand allows transmitting to the cortex any information that brings an adapted motor answer. Therefore, it has a huge importance in every thin or strong prehension. The mechanoreceptors and thermoreceptors of the palmar side of the hand are the most precise and transform the mechanical stimulus in nervous impulse, which travels through different types of nervous fibres corresponding to different types of sensitivities.
12.3.1 Sensorial Receptors
The hand has approximately 17,000 tactile unities, which gives it important precision allowing precise prehensions. The discriminative sensitivity can be lower than 2 mm between the thumb and the radial index.
Very briefly, there are two big categories of receptors that work differently and don’t react the same way when receiving a stimulus. The essential difference is that the fast-adapting receptors (FA) react to the stimulus with only 1 pulse, whereas the slow-adapting receptors (SA) modify the frequency of their pulses.
Hairless skin presents several types of receptors that react to mechanical, thermic or painful stimuli.
12.3.1.1 Mechanoreceptors (Fig. 12.2)
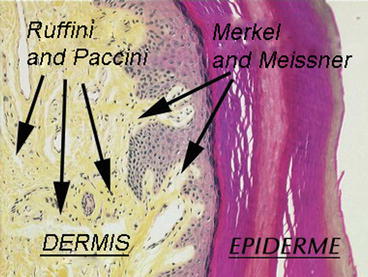
Fig. 12.2
Location of the mechanoreceptors in the palmar side of the hand
Meissner corpuscles localised in the papillary groove between the epidermis and the dermis. They are fast-adapting receptors sensitive to low frequencies (30–40 Hz) and to exploratory touch.
Pacinian corpuscles localised in the deep dermis and the subcutaneous tissue. They are fast-adapting receptors, very sensitive to frequencies between 250 and 350 Hz.
Merkel cells localised at the level of the junction between the epidermis and the dermis. They are slow-adapting receptors, and their capacity of modulating their pulses favours the touch and pressure evaluation. Cold temperatures increase their excitability, while hot temperatures inhibit them.
Ruffini corpuscles localised in the dermis. They are slow-adapting receptors sensitive to pressure and play a role in detecting displacements and positions. They are more sensitive to cutaneous stretching than to vertical pressures and are excited by cold temperatures and inhibited by hot temperatures.
12.3.1.2 Thermoreceptors (Fig. 12.3)
Fig. 12.3
Thermoreceptors’ activity depending on the cutaneous temperature
Hot receptors are point located, which explains why the thermo-sensitivity works by “stains” of approximately 1 mm. They are active from 30 °C, to liberate a pulse peak between 38 and 43 °C. They stop emitting this pulse below 32 °C or above 48 °C (then the nociceptive fibres are the ones that are active).
Cold receptors are also point located, with a reception field of 1 mm. They are active from approximately 10 °C to liberate a pulse peak between 20 and 30 °C. They stop emitting this pulse below 10 °C and between 38 and 48 °C. Between 48 and 50 °C, they react paradoxically, creating a feeling of cold.
When we put the hand in cold water, the thermoreceptors’ activity is important at first, and then it decreases. This can explain the fact that water seems less cold after a short time. The same phenomenon exists with hot temperatures.
12.3.1.3 Nociceptors
They are activated by stimulations which excitement threshold is higher than for other types of receptors. They allow defining risky stimulations, potentially damaging. There are 3 types of receptors (mechanonociceptors, thermic and mechanic receptors, polymodal), related to fibres with different diameters, which permit transmitting a well-localised acute pain followed by a delayed burning pain, less localised but during longer.
12.3.2 Sensitivity Types
12.3.2.1 Nociceptive Sensitivity
Types of Pain
According to the medical dictionary Flammarion, pain is “an abnormal and unpleasant sensation caused by the excessive excitation of a living part of the organism, perceived and integrated at the highest level of the cerebral cortex, which gives it a characteristic of personal experience and an emotional nature”. This definition is in accordance with the fact that pain is related to physical factors, perceived differently depending on the individual.
It can be defined according to clinical or physiopathological criteria.
Clinically, we distinguish acute and chronic pain.
Acute pain is an alarm signal in response to an aggression that could jeopardise the integrity of the individual. When the injury heals, the painful message disappears. This system allows the subject to adapt his behaviour to the injuries he’s suffering and therefore favours his recovery.
Chronic pain is pain that has been lasting more than 3–6 months. It works on its own without associated tissue injuries and causes structural modifications in the central nervous system, leading to modifications of the pain threshold. These modifications can make pain more intense (hyperalgesia), make painless stimuli painful (allodynia) or allow the apparition of spontaneous pains. This kind of pain can change the patient’s behaviour with social and family consequences that can be catastrophic.
On a physiopathological level, we differentiate neuropathic pains and pains with excess of nociception.
The last ones are triggered by a stimulation of the nociceptors, are mechanical and are located on the damaged area without neurological topography.
Neuropathic pains are related to a peripheral or central nervous damage and can be continued or intermittent, without mechanical stress. They can feel like a burn, an electric shock or a dysesthesia and are located on the topographic area of the damaged nerve. They can be associated with hyperesthesias, allodynias, hypoesthesias or anaesthesia.
We also have to add to these two types of pain: the pains maintained by the sympathetic system (CRPS types 1 and 2) and the psychogenic pains (somatisation, hypochondria, delirium, etc.).
In practice, this classification raises problems as several types of pain can be involved. Sometimes we don’t know the pain’s origin, and a pain that seems psychogenic can in fact be a chronic pain with a side effect on the patient’s psyche.
Transmission of the Nociceptive Message
The nociceptors are either mechanonociceptors Aδ responding to mechanical and hot stimulations or polymodal nociceptors C responding to intense mechanical, thermal or chemical stimuli. They convey the pain message towards the spine through Aδ fibres poorly myelinated (localised and sharp pain) or C fibres unmyelinated (delayed and widespread pain). These fibres have a moderate diameter and a conduction speed inferior to the Aβ fibres conveying sensitivity for fine touch (Table 12.1).
Table 12.1
Characteristics of the sensorial fibres
Sensorial fibers | Roles | Myelination | Diameter (μm) | Conduction speed (m/s) |
|---|---|---|---|---|
Aβ | Proprioception: neuromuscular bundles | + | 12–20 | 70–120 |
Golgi tendon organ | + | |||
Cutaneous sensitivity: touch | + | 5–12 | 30–70 | |
Aδ | Cutaneous pressure: temperature | + | 2–5 | 12–30 |
C | Cutaneous pain: pain | − | 0.4–1.2 | 0.5–2 |
These fibres enter the dorsal horn of the spinal cord where there is a medullary relay with two types of neurons:
Specific nociceptive neurons that convey only pain messages.
Polymodal neurons that convey any kind of information, nociceptive or not, coming from the skin, the guts or the muscles. The convergence of informations at the cortical level can lead to a processing error that can cause referred pain, where we find a cutaneous metameric pain when the origin is visceral, articular or muscular.
When coursing towards the brain, the pain message is modulated by various factors that can amplify or inhibit it.
Nociceptors Sensitivity
The substances released around the damaged tissues can increase the inflammatory phenomena, lowering the excitability threshold and causing allodynia.
Pain Memory
The pain message lasts too long; the hormonal and chemical phenomena involved in the message transmission can “soak up” the nerve cells that “remember” this pain signal. Any other signal is then traduced as if it were nociceptive.
Axon Reflex
In the dorsal horn, the affluence of nociceptive messages can create a neurogenic inflammation that can maintain pain.
Gate Control or Melzack and Wall’s Theory
Large fibres have an inhibitory action on the nociceptive message conveyed by fibres Aδ and C with antidromic conduction.
The Opioid System
The opioid receptors of the nervous system are present at the level of the central and peripheral systems and oppose nociceptive messages.
There is an integration of pain in the brain where there is also a modulation of the pain message that depends on the circumstances of the injury and the individual’s culture and background.
12.3.2.2 Protopathic Sensitivity Other Than Nociceptive
Besides the nociceptive message, Aδ and C fibres convey informations about temperature and cutaneous pressure. The thermoreceptors react after 45 °C and under 10 °C and can convey a pain message in case of important stimulus. The informations arrive in the dorsal horn of the spinal cord at the level of convergent cells that receive nociceptive informations and other sensorial messages.
12.3.2.3 Epicritic Sensitivity
The epicritic sensitivity conveys informations of fine and discriminative displacements, pressure or vibration. Two types of mechanoreceptors collect mechanical informations and change them in nervous impulses:
Type 1 receptors are small and cover a small skin surface.
Type 2 receptors cover a wider surface and don’t have precise limits.
Each of these receptor types can have a slow adaptation (and send the message during the whole stimulation) or a fast adaptation (and send the message at the beginning and at the end of the stimulation).
The cutaneous territory concerned by one receptor is small in the hand, which explains the important sensorial precision at this level.
The sensorial message coming from these receptors is conveyed by Aβ fibres that are large myelinated fibres with important conduction speeds.
12.3.2.4 Proprioceptive Sensitivity
It conveys informations concerning the limbs’ position and movements, essential for the cortex to regulate the muscular tensions and adapt to every situation. The sensitivity relies on several mechanoreceptors at a muscular, tendinous and articular level, to which we must add cutaneous receptors that also participate in the formation of the proprioceptive message:
Golgi tendon receptors that gives informations about the tendon tension and whose message is conveyed by Aβ fibres and has an inhibitory role on motoneurons during tendon stretching.
Joint receptors at the level of the capsule and ligaments, which give information about the joint position and movements. They’re made by three slow adaptation mechanoreceptors (Golgi organ, Ruffini corpuscles and free nerve endings) and one fast adaptation receptor (Pacinian corpuscles).
Neuromuscular bundle, made by two types of receptors: nuclear chains fibres reacting to continuous stretching and nuclear bag fibres reacting to short stretching. The number of fibres in the bundle is very important in the hand for fine movements. In each extremity, the bundle is innervated by Aγ motor fibres that regulate its tension.
12.3.2.5 Autonomic System
The autonomic system concerns the innervation of the guts and the endocrine and exocrine glands and the vasomotor activity.
The autonomic system is composed by two antagonist but complementary systems:
The parasympathetic system whose role is to reduce the use of energy (trophotropism)
The sympathetic system that produces energy (ergotropism)
Any disturbance in the balance between them can lead to important autonomic disorders, like the ones we can find in CPRS where the predominance of the sympathetic system causes vasomotor, pilomotor and sudoriparous disorders, as well as pain exacerbation by axon reflex.
12.4 Assessment and Rehabilitation of Sensorial Disorders [3–5, 12, 17]
In axonal injuries of cutaneous nerves, the skin can develop two different states:
It presents a decrease or even total loss of sensitivity, depending on the number of axons damaged in the nerve (no pain).
It develops an unpleasant or even painful sensitivity (tingling, neuroma, allodynia, neuralgia, etc.), depending on the gravity of the phenomenon, with stimuli that aren’t normally painful.
These two categories are assessed and treated in different ways, knowing that in case of pain there is also an underlying hypoesthesia that has to be treated later.
Therefore, we have to figure out if we’re dealing with a “hypersensitive skin” or a “hypoesthesic skin”.
12.4.1 Hyposensitivity
12.4.1.1 Assessment [8, 14]
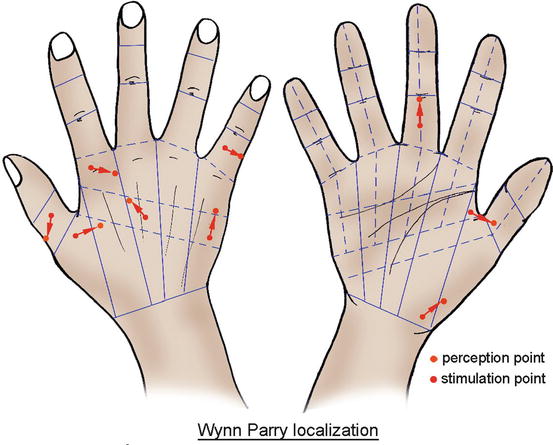
Identification of a Hyposensitive Area (Esthesiography)
The first exam we realise in case of a partial nerve injury is an esthesiography that defines the hyposensitive area.
The pressure perception threshold in the palmar side of the hand is 0.1 g and the one in the dorsal side is 0.3 g. The one for the rest of the body is 0.6 g.
We, respectively, use aesthesiometers of 0.2, 0.4 and 0.7 g depending on the area we want to assess.
During the test, the patient must close his eyes and say “touch” when he feels the contact of the monofilament.
When touching the patient, the monofilament must bend under pressure, and the contact must last 2 s. We have to wait 10 s between two applications.
The assessment is realised in order to define an area as precise as possible, in relation to a reference point like a flexion crease, a scar, etc.
The first point is placed on the longitudinal axis of the damaged nerve branch. We progress centimetre by centimetre from distal to proximal, until the first point where the patient doesn’t feel anything. The therapist then progresses from proximal to distal millimetre by millimetre until the first detected point, then one last time from distal to proximal millimetre by millimetre until the first non-detected point. This point is transferred on the graph paper on which we realise the assessment.
The same process is realised to define the most proximal non-detected point and then the 2 transverse points of the area (Fig. 12.4).