Abstract
Posterior cortical atrophy (PCA) is a degenerative syndrome heralded by progressive visual and spatial disorders, while the memory and execution capacities remain preserved for a long time. We report the clinical case of a female patient who received a global Physical and Rehabilitation Medicine (PRM) therapy. Our objective is to highlight the interest of a multidisciplinary approach in PCA. A female patient, LO, 60 years old, presented with visual and spatial difficulties of progressive worsening, while global cognitive efficiency was preserved, signing PCA, with a loss of autonomy in daily life. A six-month multidisciplinary approach (speech therapy, occupational therapy, and physiotherapy) centered on her visual disturbances and associated to the reinforcement of her preserved abilities, as well as a rehabilitation program, was proposed. At the end of this period, LO was again able to read, find efficient exploratory strategies, use the underground, visit museums, have leisure activities, and carry out everyday life activities, which she had ended up abandoning. The specific therapeutic management allowed reaching functional objectives. Our hypothesis is that the absence of other cognitive disorders allowed this type of rehabilitation “contract”. The neurodegenerative pathologies responsible for specific instrumental disabilities without global cognitive alteration, and particularly PCA, should be able to benefit from a specific, or even multidisciplinary PMR therapy approach.
Résumé
L’atrophie corticale postérieure (ACP) est un syndrome dégénératif qui se manifeste par des troubles visuels et spatiaux progressifs, alors que les capacités mnésiques et exécutives restent longtemps conservées. Nous rapportons le cas clinique d’une patiente ayant bénéficié d’une prise en charge globale en médecine physique et de réadaptation (MPR). Notre objectif est de souligner l’intérêt d’une prise en charge multidisciplinaire dans l’ACP. Nous présentons une patiente, LO, 60 ans, qui présentait des difficultés visuelles et spatiales d’aggravation progressive alors que l’efficience cognitive globale était conservée, signant l’ACP avec une perte d’autonomie dans sa vie quotidienne. Une prise en charge multidisciplinaire (orthophonie, ergothérapie, et kinésithérapie) centrée sur ses troubles visuels associée à un renforcement de l’utilisation de ses capacités préservées et un programme de réadaptation lui a été proposée durant six mois. Au terme de cette période, LO a pu de nouveau lire, retrouver des stratégies exploratoires efficaces, réutiliser le métro, retourner visiter des musées, reprendre des activités de loisirs et s’acquitter de tâches de la vie courante qu’elle avait fini par abandonner. La prise en charge spécifique a permis d’atteindre des objectifs fonctionnels. Notre hypothèse est que l’absence d’autres troubles cognitifs a permis ce type de « contrat » de rééducation. Les pathologies neurodégénératives responsables de troubles instrumentaux spécifiques sans altération cognitive globale et notamment l’ACP doivent pouvoir bénéficier d’une prise en charge spécifique, voire multidisciplinaire de MPR.
1
English version
1.1
Introduction
Posterior cortical atrophy (PCA) or Benson’s syndrome is a rare neurodegenerative syndrome mainly characterized by progressive visual-perceptive deficits. PCA is often described as a visual variance of Alzheimer’s disease where neurovisual disorders without any alteration of episodic memory and executive functions in the early stage of the disease are prevailing . The histo-pathological lesions are actually similar to those of Alzheimer’s disease (senile and neurofibrillary plaques) but with different locations. By comparison with Alzheimer patients, the cerebral perfusion scintigraphy shows that the patients with PCA have a more severe occipitoparietal hypoperfusion and few perfusional anomalies in the frontal, cingular anterior and mesiotemporal regions . PCA can however be the consequence of other neurodegenerative pathologies like corticobasal degeneration, dementia with Lewy bodies or prion diseases . PCA is characterized by deficits of visual origin which, by reference to the cortical visual pathways, are classified in two clinical syndromes :
- •
a ventral, occipito-temporal stream (the “what” pathway) where patients present with difficulties of recognition, for objects, images, or places, with prosopagnosia, as well as with visual extinction and even a campimetric deficit in quadrant or hemifield;
- •
a dorsal, occipito-parietal stream (the “where” pathway) where the difficulties of visual integration are of visual-spatial type proposing simultagnosia, optical ataxia able to develop into a complete Balint’s syndrome, alexia, as well as spatial agraphia .
Praxic and spatial disorders (dressing apraxia, constructive apraxia, ideomotor apraxia) are associated. Memory, language, and judgement are preserved for a long time. Rehabilitation therapy of these patients is still little documented in literature, although advised , as its benefits for the patients are encouraging .
We report the clinical case of a female patient who benefited from a multidisciplinary approach in speech therapy, occupational therapy, and physiotherapy in Physical Medicine and Rehabilitation, centered on her visual disorders and associated to the reinforcement of the use of her preserved capacities, as well as a program of rehabilitation aiming to the resumption of everyday life activities. Our objective is to highlight the interest of a multidisciplinary therapeutic approach in PCA.
1.2
Patient case
LO is a 60-year-old female patient presenting with visual difficulties of progressive worsening starting in 2001 as she was 54. She was describing a setting-up mode of specifically visual difficulties over 2 or 3 years. The ophthalmology consultations had revealed a left inferior quadranopsia without any explanation of its neurological mechanism. The progressive worsening of the symptoms led her to retire from the management of an informatics SME. Her complaints had started with the impossibility to recognize photos, up to the impossibility to reproduce gymnastic movements executed by a teacher in front of her, while she was able to execute them if they were described verbally. She was unable to move around alone, driving had become impossible, she could not anymore read books, hand-written writings, even her own writing “There are some words that are leaving, there was a book and I was reading, I didn’t understand the text, it was non-sense”, nor watch television. She had difficulties finding objects at home, and finding the right direction. She put on her clothes the wrong way, was unable to count the change or find an object in her bag. However, she had not stopped getting dressed by herself, although she did it slowly.
1.3
Evaluation before intervention in Physical and Rehabilitation Medicine
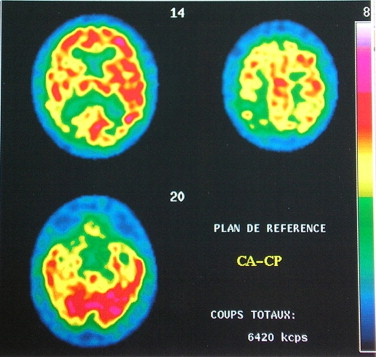
It took several years before LO was addressed to the center of reference for young subject dementia. A neuropsychological check-up performed in 2007 objectivized visual agnosia, simultagnosia, visual-constructive apraxia, visual-spatial work memory disorder, left spatial neglect while global cognitive efficiency was preserved, and in particular, the patient had no mnesic or executive disorder ( Table 1 ). The clinical examination was normal except for the deficit of the visual field in the left inferior quadrant. A moderate depressive syndrome was also noted. This visual and spatial instrumental impairment of progressive evolution, and in the absence of mnesic disorder, suggested a PCA, the diagnosis of which was confirmed by brain scintigraphy authenticating a bilateral parieto-temporo-occipital hypoperfusion with a clear right predominance including the primary visual cortex on the right ( Fig. 1 ).
| Neuropsychological evaluation | 2007 | 2008 | ||
|---|---|---|---|---|
| Raw scores | Normal ranges | Raw scores | Normal ranges | |
| MMS (/30) | 26 | − 3,6 δ | 28 | −1.1 δ |
| Direct verbal span | 6 | 0 δ | 5 | −0.7 δ |
| Indirect verbal span | 4 | 4 | ||
| Spatial span | 3 | −3 δ | 4 | − 2.7 δ |
| Indirect spatial span | 2 | 3 | ||
| FAB (/18) | 16 | −1.6 δ | 17 | −0.4 δ |
| Picture naming test (DO−80) | 72/80 | 73/80 | ||
| Picture naming test I | 10/10 | 11/12 | ||
| Verbal fluency (1 min) | ||||
| Animals | 20 | −0.43 δ | 21 | −0.23 δ |
| M letter | 24 | 2.1 δ | 19 | 1 δ |
| Copy of Rey’s figure | NA | − | 6,5/36 | < Cent 10 |
| Type IV (317 s) | ||||
| Episodic memory | ||||
| RL/RI 16 items | ||||
| Identification (/16) | 16 | 16 | ||
| Immediate piloted recall (/16) | 16 | > Cent 50 | 14 | Cent 5–25 |
| Total free recall (/48) | 34 | 39 | ||
| FR 1 | 11 | 0.3 δ | 10 | 0.2 δ |
| FR 2 | 10 | −1 δ | 13 | 0.8 δ |
| FR 3 | 13 | −0.2 δ | 16 | 1.6 δ |
| Total free + piloted recall (/48) | 47 | 45 | ||
| TR 1 | 16 | > Cent 75 | 13 | Cent 5–25 |
| TR 2 | 15 | Cent 5 – 25 | 16 | > Cent 50 |
| TR 3 | 16 | > Cent 25 | 16 | > Cent 25 |
| Recognition (/16) | 16 | 16 | ||
| Delayed free recall (/16) | 12 | 0.4 δ | 14 | 0.5 δ |
| Delayed total recall (/16) | 16 | 16 | ||
| Incident memory of picture naming test 1 | 4/6 | 6/6 | ||
| Rey’s figure memory | NA | NA | ||
In front of the importance of the functional complaints, LO was then oriented to the consultation of the PMR department for the management of her difficulties, six months following the initial evaluation. A neurovisual examination, according to the works by Ducarne and Barbeau was performed in speech therapy in complement to the neuropsychological test ( Table 1 ). Listening to LO’s initial complaints, we made the hypothesis of an assessment with highly failed results. Spontaneously, LO’s look was fixed, vague, and wasn’t exploring anything. There was no frank seeking of her interlocutor’s eyes, however the look was able to be mobilized upon simple verbal stimulations. The strategy of visual exploration was relatively correct in piloted situation: counting of cubes and objects with a compensation of the left inferior quadranopsia of good quality. The visual-motor coordination was preserved in the ticking tasks in all visual fields.
A picture-naming test consisting of drawings of objects (DO-80) revealed a disorder of visual recognition (72/80). In order to recognize certain items, LO had sometimes to orient the drawings differently for being able to name them, the global form being generally perceived (ash-tray: a table mat, a plate? clog: isn’t it a bath tube? mushroom: head of carapace), while the performances during word evocation task showed no difficulty of phasic or semantic type.
The recognition of complex photos (0/7) was on the other hand much more impaired as illustrated by her comment on a photo with a background/form-related difficulty of a butterfly on a water-lily: “It looks like the Earth seen from the sky.” ( Fig. 2 ). It was the same for the photos of places (1/5) and personalities (3/14). The difficulties of recognition of faces and persons were however not observed in daily life, neither for the patient’s familiar circle, nor for the acquisition of new faces. In addition, LO has never mixed up or not recognized her rehabilitators.

The description of a complex setting was impossible as a global picture, revealing simultagnosia. LO was able to distinguish certain details, but could not see the whole of it, particularly hindered by the mass of information. Contrary to the simple tests of visual exploration, there was no exploration strategy any more, there was a wandering of the look.
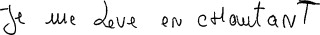
Reading was possible on a non-handwritten medium, but some skipped words or lines made it inefficient. LO had difficulties reading her own writing, and whenever she succeeded, she was unable to correct herself. She was unable to position the tip of her pen on the letter or word to correct, revealing a visual-motor coordination deficit, which did not express itself in the test of simple pointing. Moreover, her handwriting revealed some praxical difficulties to form some letters, as well as an allographic disruption characterized by case errors within a same word ( Fig. 3 ). By taking the classifications proposed by Ross , the signs attributable to an impairment of the dorsal, occipito-parietal route were: simultagnosia, difficulties of visual-motor coordination during self-correction task while writing, apparent fixedness of the look more marked in spontaneous mode than during piloted tasks, trouble in identifying complex pictures because of the mass of information linked to the dorsal simultagnosia. Those imputable to an impairment of the ventral occipito-temporal route were less numerous like the left inferior quadranopsia and the visual agnosia.
While the functional deficits were present, what was striking during this check-up was the clear dissociation between the complaints and the performances effectively obtained in a piloted situation, as if her real capacities were under-utilized, and mainly when the simultagnosia came into play.
1.4
Rehabilitation
The patient was proposed a multidisciplinary therapy in the PMR department in order to benefit from the rehabilitation usually intended for the patients with cerebellar lesions following a CVA or a CT. The patient was informed that the rehabilitation could not prevent the worsening of the degenerative disease, but aimed to allow her utilizing to the best all her preserved capacities.
The therapy started with two sessions of speech therapy of one hour per week during which the following was performed, while favoring exercises training the occipito-parietal dorsal route:
- •
a training of the visual exploration, thanks to exercises of visual pursuit of stimuli of light, then of objects, and exercises of detection of stimuli of light then of objects, in the visual hemifields, insisting nevertheless on the left inferior quadrant. These exercises were performed in ego-centrered then in exo-centered mode. LO showed a slowness of realization characterizing the patients with neurovisual disorders, and her performances improved progressively. This slowness amended itself quickly, allowing the insertion of other exercises;
- •
exercises aiming to decrease the simultagnosia by starting with simple pictures (example: teapot: distinguish the handle and the spout of the teapot at the same time), then with more and more complex scenes with images;
- •
recognizing pictures was trained in parallel with the help of image books. This training started with simple pictures, then more and more complex images in the details and form of the objects and in the mass of information to deal with simultaneously;
- •
finally, the training on printed text could be approached, then that of handwritten writing, and finally that of her own writing. For each phase of reading, we had in a first time to enlarge the print characters up to a 24 font size and to reset the exploration strategies on a linguistic material with much constrained guidance (for example, a small green ruler was placed on the left margin indicating the limit of the text. The reading of the next line could not be possible as long as this small ruler was not seen by LO), followed by personal guidance (the left hand index replaced the small ruler while the right hand index acted as a line guide). Another major complaint by LO was that it was impossible for her to read her own writing and the handwritten manuscripts in general. From the moment when reading had become functional again, a specific training through tasks of words dictation, handwritten words matching printed words, handwritten texts reconstitution could be realized. Finally, the capacity to read again her own writing had become possible again, allowing LO resuming autonomy of taking notes, although this remained still difficult when it was question to be quick;
- •
in parallel, the elements of apraxic agraphia were trained for some letters (g and r). The speed of writing was deleterious at the letters forming. In order to preserve the control of her handwriting, we proposed her to write the words and spell them simultaneously to slow down her writing.
The sessions of occupational therapy as well as of physiotherapy have focused on the precise requests of the patient in order to favor autonomy in her daily life. Compensation strategies have therefore been proposed to her for spatial or visual tasks in daily life, especially for dressing which was difficult because of her visual difficulties to orient her clothes before putting them on and which could have some similarities with dressing apraxia. This act, which had become troublesome, had not been abandoned by the patient. Compensation was proposed, like placing the labels back on her clothes in order to identify their sense before putting them on.
In view of the patient’s improvement in terms of reduction of deficiencies, we proposed her to integrate the rehabilitation outpatient hospital for patients with cerebral lesions for a period of 7 weeks with the objective of a transfer to daily life and of the use of more global autonomy capacities, like planning and organizing projects or walks using public transport .
1.5
Evaluation after intervention in Physical and Rehabilitation Medicine
At the end of 6 months of global therapy, another neurovisual check-up was proposed. It included the same tests that those proposed during the first evaluation. The results showed clear improvements especially concerning simultagnosia. LO reports that she “learnt again watching and mobilizing her look”. The visual recognition disorders have regressed, although a relative latency remained during the visual decoding, which goes hand in hand with the complexity of the visual information to be treated (complex pictures [7/7], pictures of places [4/5], and of personalities [8/14]). The performances during the neuropsychological test remained stable compared with the initial test ( Table 1 ). On the functional level, LO was able to read again, use again the underground, visit again museums, and perform everyday activities like renovating her second home.
1.6
Discussion
LO corresponds to the descriptions of Benson’s et al. PCA , as well as to the characteristics found by Tang-Wai et al. , like the mean age of onset at around 60, the mean diagnostic delay of 4 years, and the clinics. PCA had started by a low left quadranopsia, which was diagnosed during ophthalmology consultations without explaining its neurological mechanism. The lateral homonymous hemianopsias are very often only incidentally reported in PCA, while this sign could be one of the forerunners in some patients . In LO, the neuropsychological disorders with visual predominance while the mnesic and executive abilities are preserved are in accordance with those described so far .
The objective of this clinical case study was to underline the interest of a multidisciplinary approach (speech therapy, occupational therapy, and physiotherapy) in PMR in PCA on the visual performances and on quality of life. In this perspective, a 6-months rehabilitation program was proposed to LO.
Our hypothesis was that the absence of more global cognitive deficits, like the preservation of episodic memory and executive skills, was able to contribute to the success of this rehabilitation by allowing LO integrating compensation modes.
Only few publications in literature report on rehabilitation therapy of neurovisual disorders or of patients with PCA, but they report the interest of such a management . Perez et al. , like Roca et al. , describe patients presenting with Balint’s syndrome secondary to a PCA to whom a rehabilitation program had been proposed. Roca’s et al. patient SS, a 64-year-old man, presented a PCA characterized by visual agnosia as well as a complete form of the Balint’s syndrome: a simultagnosia of dorsal type responsible for a difficulty to perceive more than one object at the same time, as well as to recognize a simple isolated object because of a defect of visual attention focusing the recognition process to an isolated part of the object, an optical ataxia as well as oculomotor disorders.
Numerous similarities need to be precised between SS and LO. On one hand, the onset of their clinical history is marked by their joint wandering in ophthalmology consultations before being directed towards a specialized neurological consultation. On the other hand, they share a common semiology of the occipito-parietal dorsal visual route with conjugated signs of visual agnosia consecutive to a perturbation of the occipito-temporal ventral visual route, without any dysexecutive or mnesic impairment, and present a relative preservation of their cognitive performances.
For both, the therapies have started by an explanation of the nature of their visual deficits and the limits of the cognitive rehabilitation as a remedy in dementias. The objectives of their therapeutic approach were prepared with a focus on the recovery of autonomy in daily life with the help of training aiming to stimulate their visual deficits, but also by establishing modes of compensation.
Like for SS, the specific management of LO has allowed reaching functional objectives responding to particular and focused requests of the patient. The reinforcement of the visual capacities contributed to the decrease of errors in everyday life and the improvement of the quality of life. It was certainly the awareness of the existence of certain of her preserved capacities and the incitement to use them, which allowed LO recovering visual autonomy. This recovered autonomy allowed therefore moving around alone and getting back a little into her previous occupational activities.
Following their respective therapies, LO and SS have learnt knowing their deficits and developing compensation strategies. This management turns out to be beneficial as long as the global cognitive capacities are preserved allowing therefore a transfer in daily life, as it was the case for LO.
This clinical history does not allow demonstrating the efficacy of rehabilitation, not being an experimental rehabilitation methodology in unique case; however, this case appeared as an example and the basis for experience transmission and educational exchange.
1.7
Conclusion
This study describes a multidisciplinary management in PMR of a patient with PCA without deficit of the executive functions. The specific therapeutic management allowed reaching the functional objectives responding to the patient’s request and has shown benefits in daily life. It could be envisaged to propose sessions over a limited period to a greater number of patients with the objective of helping them to improve their capacities and to compensate their deficits.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
L’atrophie corticale postérieure (ACP) ou encore le syndrome de Benson est un syndrome neurodégénératif rare se caractérisant principalement par des déficits visuoperceptifs progressifs. L’ACP est souvent décrite comme une variante visuelle de la maladie d’Alzheimer dans laquelle prédominent des troubles neurovisuels sans atteinte de la mémoire épisodique et des fonctions exécutives dans le stade initial de la maladie . Les lésions histopathologiques sont en effet semblables à la maladie d’Alzheimer (plaques séniles et neurofibrilaires) mais diffèrent par leurs localisations. Par comparaison aux patients Alzheimer, la scintigraphie cérébrale de perfusion montre que, les patients victimes d’ACP ont une hypoperfusion occipitopariétale plus sévère et peu d’anomalies perfusionnelles dans les régions frontales, cingulaires antérieures et mésiotemporales . L’ACP peut toutefois être la conséquence d’autres pathologies neurodégénératives telles que les dégénérescences corticobasales, les démences à corps de Lewy ou les maladies à prions . L’ACP se manifeste par des déficits d’origine visuelle qui en référence aux voies visuelles corticales sont classés en deux grands tableaux distincts :
- •
une voie ventrale occipitotemporale (voie du quoi) dans laquelle les patients présentent des difficultés de reconnaissance que ce soit pour les objets, les images, les lieux, une prosopagnosie ainsi qu’une extinction visuelle, voire un déficit campimétrique en quadrant ou en hémichamp ;
- •
une voie dorsale occipitopariétale (voie du où) dans laquelle les difficultés d’intégration visuelle sont de type visuospatial proposant une simultagnosie, une ataxie optique qui peuvent évoluer vers un syndrome de Balint complet, une alexie, ainsi qu’une agraphie spatiale .
Des troubles praxiques et spatiaux (apraxie d’habillage, apraxie constructive, apraxie idéomotrice) s’y associent. La mémoire, le langage et le raisonnement sont longtemps conservés. La prise en charge en rééducation de ces patients est encore peu documentée dans la littérature, et pourtant conseillée car elle se montre encourageante quant aux bénéfices qu’elle peut leur apporter .
Nous rapportons un cas clinique d’une patiente qui a bénéficié d’une prise en charge multidisciplinaire en orthophonie, ergothérapie, et kinésithérapie en médecine physique et réadaptation, centrée sur ses troubles visuels et associée à un renforcement de l’utilisation de ses capacités préservées et à une réadaptation en situation de réadaptation en vie quotidienne.
Notre objectif est de souligner l’intérêt d’une prise en charge multidisciplinaire dans l’ACP.
2.2
Présentation de la patiente
LO est une femme de 60 ans qui a présenté des difficultés visuelles d’aggravation progressive qui ont débuté en 2001 alors qu’elle avait 54 ans. Elle décrivait un mode d’installation de difficultés spécifiquement visuelles sur deux ou trois ans. Les consultations en ophtalmologie avaient mis en évidence une quadranopsie inférieure gauche sans en expliquer le mécanisme neurologique. L’aggravation progressive des symptômes l’avait amenée à prendre sa retraite de gérance d’une PME en informatique. Ses plaintes avaient débuté par une impossibilité à reconnaître des photos jusqu’à une impossibilité à reproduire des mouvements de gymnastique qu’un professeur exécutait devant elle, alors qu’elle pouvait les réaliser si ceux-ci lui étaient décrits verbalement. Elle ne pouvait plus se déplacer seule, la conduite lui était devenue impossible, elle ne pouvait plus lire de livres, les écritures manuscrites, ni même sa propre écriture « Il y a des mots qui partent, il y avait un livre et je lisais, je ne comprenais pas le texte, ça veut dire n’importe quoi », ni regarder la télévision. Elle éprouvait des difficultés à retrouver certains objets chez elle, et à s’orienter. Elle se trompait de sens lorsqu’elle revêtait ses habits, était incapable de compter la monnaie ou de retrouver un objet dans son sac. Elle n’avait cependant pas arrêté de s’habiller seule même si elle le faisait lentement.
2.3
Évaluation avant intervention en Médecine Physique et de Réadaptation
Le diagnostic a erré plusieurs années avant que madame LO ne soit adressée au centre de référence démence sujet jeune. Un bilan neuropsychologique réalisé alors en 2007 objectivait une agnosie visuelle, une simultagnosie, une apraxie visuoconstructive, un trouble de mémoire de travail visuospatiale, une négligence spatiale gauche alors que l’efficience cognitive globale était conservée et en particulier la patiente n’avait pas de trouble mnésique ou exécutif ( Tableau 1 ). L’examen clinique était sans particularité en dehors du déficit du champ visuel dans le quadrant inférieur gauche. Il existait aussi un syndrome dépressif modéré. Cette atteinte instrumentale visuelle et spatiale, d’installation progressive et en l’absence de trouble mnésique évoquait une ACP, dont le diagnostic a été confirmé par une scintigraphie cérébrale authentifiant une hypoperfusion pariéto-temporo-occipitale bilatérale à nette prédominance droite incluant le cortex visuel primaire à droite ( Fig. 1 ).









