CHAPTER 4
Physical Examination
General Principles of the Physical Examination
• Musculoskeletal examination should include the following 6 items, in order:
1. Inspection
2. Range of motion (active and passive)
3. Evaluation of muscle tone, strength, and flexibility
4. Neurologic examination
5. Joint stability
6. Palpation
• Special tests may elicit findings unique to specific diagnoses.
• Height, weight, and body mass index (BMI) should be plotted with a notation of trends over time.
BMI = weight (kg)/(height [m])2
BMI = 703 × weight (lb)/(height [in])2
• Have the family assist with keeping the child as calm and comfortable as possible during the examination; siblings often prove helpful in this regard.
• Ask the parent to help the child actively perform specific tasks, such as undressing, walking in the hallway, or even having the parent initially palpate to localize possible areas of tenderness in an extremely anxious toddler.
• Children may be more comfortable being examined on a parent’s lap; they can be transitioned to the examination table once they become more at ease with the physician.
• Inspection and active range of motion should be assessed before palpation and passive range of motion, lest the child become upset and resist examination altogether or it becomes too painful to move a joint.
• Children often have difficulty localizing pain, and pain may be referred from an adjacent joint. Always examine the joint above and the joint below the reported location of symptoms. Remember that the spine is the “joint” above the hips.
• To gain the child’s trust, begin by examining areas farthest from the region of concern.
• Hip, spine, and gait evaluation should be a standard part of the routine well-child visit.
— Evaluate the hips until the child walks with a normal gait.
— Evaluate the spine for scoliosis at each visit.
• Any child with skeletal anomalies requires examination for associated congenital or systemic abnormalities (see Chapter 3, History, Tables 3-2 and 3-3, for examples).
Inspection
• Inspect areas that are less directly related to the patient’s chief issue first to make sure they are not overlooked.
• Note posture, symmetry, surface landmarks, and muscle bulk or atrophy.
• Inspect for deformities such as abnormal alignment, joint effusions, skin changes, and unusual prominences.
Range of Motion
• Passive and active range of motion are best measured with a goniometer (Figure 4-1), which allows for comparison to normal ranges (Table 4-1) and provides baselines for follow-up examinations. Measurements should include the opposite limb for comparison.
• When a goniometer is unavailable, reasonably estimate to the closest 15 degrees.
• If necessary, comparison with the opposite limb may suffice (eg, “symmetrical,” “right is decreased compared to left”).
• Very young or uncooperative children should be prompted to reach for or move toward a desired object, such as a toy or a sticker. Alternatively, have the parent perform passive range of motion on the child.
• The degree of ligamentous laxity or joint range of motion tends to be hereditary and is highly variable among individuals.
• Children and females tend to have greater joint mobility. As such, criteria for diagnosing generalized joint hypermobility is based on age and sex. In boys and men aged 8 years and older and women aged 40 years and older, a Beighton score (Figure 4-2) greater than 4 indicates generalized ligamentous laxity (ie, joint hypermobility). For everyone else, a Beighton score greater than 5 indicates generalized hypermobility.
— Approximately 7% of the population demonstrates generalized ligamentous laxity.
— Because a proportion have syndromic hypermobility, such as Marfan syndrome or Ehlers-Danlos syndrome, further evaluation by a geneticist may be warranted for children with diffuse, extreme joint mobility because of potential involvement of other organ systems (specifically cardiovascular and ocular).
— Generalized ligamentous laxity has been associated with hip dysplasia and pes planus, and patients with “benign” and syndromic hypermobility frequently experience chronic pain.
— Hypotonia often manifests as hypermobility and vice versa.

Figure 4-1. A goniometer quantifies joint range of motion.
Table 4-1. Normal Joint Range of Motion for Childrena
| Joint | Direction | Normal Degree of Motion |
|---|---|---|
| Cervical spine | Flexion Extension Lateral rotation Lateral bending | 65 85 75 45 |
| Shoulder | Abduction Forward flexion Extension Internal rotation External rotation | 180 180 45 55 45 |
| Elbow/Forearm | Flexion Extension Supination Pronation | 140–150 0 5 70 |
| Wrist | Extension Flexion Ulnar deviation Radial deviation | 80 70 30 20 |
| Hip | Flexion Extension Abduction Internal rotation External rotation | 120–145 20–25 45–70 35–50 45–55 |
| Knee | Flexion Extension | 150 0 |
| Ankle | Dorsiflexion—knee flexed Dorsiflexion—knee extended Plantar flexion | 20–25 10–20 50 |
a Normal range of motion varies with age and sex and with girls and younger children who demonstrate greater joint mobility.
Muscle Tone
• Tone is resting muscle tension.
— Normal tone demonstrates some degree of resistance to passive joint range of motion.
— Hypotonia is decreased resistance to passive joint range of motion.
■An infant who “slips through” the examiner’s hands when being held underneath the arms has hypotonia.
■Mild hypotonia is not uncommon in infants.
— Hypertonia is increased resistance to passive joint range of motion.
■Indicates an upper motor neuron lesion, such as spastic cerebral palsy. In these patients, tone will be greatest with the initiation of passive movement and will decrease somewhat with continued movement.

Figure 4-2. The Beighton 9-point score screens for widespread joint hypermobility, as seen in this patient with Ehlers-Danlos syndrome. Score 1 point for each thumb that can touch the palmar aspect of the wrist (A), 1 point for each index finger that extends past 90 degrees at the metacarpophalangeal joints (B), 1 point for each elbow that hyperextends greater than 10 degrees (not shown), 1 point for each knee that hyperextends greater than 10 degrees (not shown), and 1 point for placing palms flat on the floor without bending the knees (not shown).
■ Normally, during abrupt ankle dorsiflexion, there is a “catching sensation” followed by a relaxation. This catch is often absent in patients with hypotonia. When this catch repeats itself rhythmically, clonus is present.
❖ The number of beats determines whether clonus is pathologic.
❖ Normal infants may exhibit up to 5 beats of clonus, whereas adults should have fewer than 2.
❖ Sustained clonus usually represents upper motor neuron pathology and related spasticity.
Muscle Strength
• Evaluate strength in infants by noting grasp strength, head control, ability to bear weight on the legs, and resistance to movements.
• For children and adolescents, manual muscle testing is commonly used to grade strength of individual muscles or functional movements (eg, elbow flexion) by asking the patient to actively contract the muscle as the examiner provides resistance (Table 4-2). The pattern of weakness can locate the deficit to a specific muscle, nerve, or spinal cord level (Table 4-3).
• Assess proximal lower extremity strength by watching the child rise from a seated position on the floor. A child with proximal lower extremity weakness (eg, muscular dystrophy) will use the Gowers maneuver (Figure 4-3) to rise by walking the hands up the thighs.
Table 4-2. Grading Muscle Strength
| Grade | Response |
|---|---|
| 1 | Patient has muscle contraction that can be seen or felt but does not result in movement. |
| 2 | Movements can be made only when the force of gravity is counteracted by changing patient’s position. |
| 3 | Patient can resist gravity but no additional force. |
| 4 | Patient has only some ability to resist the examiner. |
| 5 | Patient has full ability to resist the examiner. |
Table 4-3. Reflexes and Motor Function of Specific Spinal Cord Levels



Figure 4-3. Gowers maneuver. Child rises from a seated position on the floor by using his hands to walk up his thighs, indicating proximal lower extremity weakness, as seen in muscular dystrophy.
Muscle Flexibility
• Because bones grow faster than muscles, children often experience symmetric tightness in the lower extremity muscles during growth spurts.
• This tightness increases traction on growth centers, increasing the risk for some overuse syndromes (see Chapter 33, Overuse Injuries).
• The most commonly affected muscles are those that cross 2 joints—the gastrocnemius (Figure 4-4), the hamstring (Figure 4-5), the rectus femoris (Figure 4-6), and the tensor fascia lata/iliotibial band (Figure 4-7).
Reflexes
• Each reflex represents a specific level of spinal cord function (see Table 4-3).
• Deep tendon reflexes are graded on a 0 to 4 scale (Table 4-4) or characterized as normal, increased, or decreased.

Figure 4-4. (A) With gastrocnemius tightness or contracture, passive ankle dorsiflexion will be less than 10 degrees while the knee is fully extended. (B) Degree of ankle dorsiflexion should increase when the knee is flexed; if it does not, the soleus muscle is also tight.

Figure 4-5. Popliteal angle to measure hamstring flexibility. Patient is supine with the contralateral leg flat on the examination table. Hold the ipsilateral hip at 90 degrees and passively extend the knee to its natural limit. Generally, the complement of the angle formed by the thigh and lower leg is recorded. Popliteal angle (α) greater than 30 degrees indicates hamstring tightness.
• Children with upper motor neuron pathology often have increased reflexes, whereas children with lower motor neuron or muscle disease tend to have decreased reflexes.
• Superficial reflexes, including umbilical, cremasteric, and plantar reflexes, may yield information about spinal cord pathology.
• Distraction techniques reduce inhibition so reflexes can be more easily elicited.
— Ask the child about their interests or activities, or ask the child to interlock their hands and pull while reflexes are checked (Figure 4-8).
• When neonatal reflexes persist beyond the age at which they normally extinguish, suspect a neurodevelopmental problem.
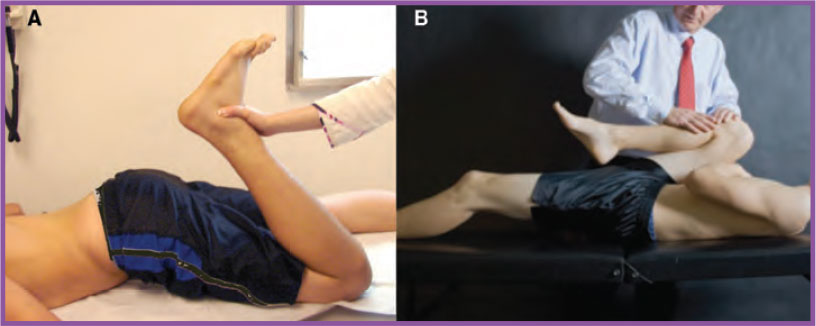
Figure 4-6. (A) Ely test for rectus femoris contracture. With patient prone, passively flex the knee; in the presence of a rectus femoris contracture, the pelvis will rise off the examination table as shown. (B) The Thomas test assesses rectus femoris flexibility. With the patient supine, the test is positive when the leg rises above the table while the opposite hip is maximally flexed (indicates tight hip flexors on leg that rises up).
(B) from Gomez JA. Hip, pelvis, and thigh. In: Harris SS, Anderson SJ, eds. Care of the Young Athlete. 2nd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2010: 393–408.

Figure 4-7. Ober test to assess for iliotibial (IT) band tightness. Child is placed on his side. With one hand under the knee for support, use the other hand to bring the hip into extension and slight abduction. Remove the hand supporting the knee, and allow the knee to fall to the table. The Ober test is positive for tight IT band if the hip does not adduct past the midline of the body.
From Gomez JA. Hip, pelvis, and thigh. In: Harris SS, Anderson SJ, eds. Care of the Young Athlete. 2nd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2010: 393–408.
Table 4-4. Grading Reflexes
| Grade | Response |
|---|---|
| 0 | No response |
| 1 | Minimal response |
| 2 | Normal response |
| 3 | Slightly hyperactive |
| 4 | Very hyperactive with clonus present |

Figure 4-8. Distraction technique to elicit deep tendon reflexes. Ask patient to clasp the hands and pull outward.
Sensation
• Older children and adolescents can participate in a thorough sensory examination.
• Sensation to light touch is tested first.
• When a sensory deficit is present, determining which dermatomes or nerve distributions are affected can point to the location of the pathology (nerve distributions) (see Table 4-3).
•
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








