Pharmacology considerations for the aging individual
Charles D. Ciccone
Introduction
Older adults receiving physical rehabilitation services are commonly taking medications to help resolve acute and chronic ailments. These medications are intended to improve the patient’s health but they frequently cause side-effects that can have a negative impact on the patient’s response to physical rehabilitation. The elderly are more susceptible to adverse effects of drugs owing to many factors, including excessive drug use, declining function in various physiological systems, and altered drug metabolism and excretion.
In particular, age-related physiological changes in liver and kidney function can profoundly affect drug metabolism and excretion (Shi & Klotz, 2011). Many medications are metabolized and inactivated to some extent in the liver, and age-related decreases in liver size, hepatic blood flow and enzymatic capacity can impair the body’s ability to metabolize these medications. Likewise, the kidneys are the primary site of drug excretion, and progressive decreases in renal mass, renal blood flow, filtration capacity and nephron function can reduce the body’s ability to remove various drugs and their metabolites from the bloodstream. Because of these age-related physiological changes, the body is not able to eliminate drugs in a timely and predictable manner, thus leading to drug accumulation and an increased risk of adverse drug reactions.
Deficiencies in other physiological systems may also increase the likelihood of adverse drug reactions in older adults (Petrovic et al., 2012). For example, an older adult with impaired balance reactions will be more likely to fall when taking benzodiazepines (i.e., Valium-like drugs) and other drugs that impair balance. An older patient who has cognitive deficits might become more confused when taking opioids and other medications that affect cognition. Hence, problems related to a decline in any physiological system will almost certainly be magnified by drugs that adversely affect that system.
Nonetheless, older adults often rely on medications to help improve their health and quality of life. It follows that health professionals should be aware of the primary medications being taken by their elderly clients and how those medications can affect patients’ participation in rehabilitation.
Some of the primary medications used to treat conditions commonly seen in older adults are addressed here. This discussion is not meant to be all-inclusive but should help clinicians to recognize and understand how medications taken by the elderly can affect their response to rehabilitation.
Treatment of pain and inflammation
Opioid analgesics
Opioid (narcotic) medications such as morphine and meperidine (Table 12.1) are powerful analgesics that bind to neuronal receptors in the spinal cord and brain. These medications reduce synaptic activity in pain-transmitting pathways, thereby decreasing pain perception. Common side-effects of opioids include sedation, respiratory depression, constipation and orthostatic hypotension. Practitioners should also be aware that older adults are more susceptible to opioid-induced psychotropic reactions such as confusion, anxiety, hallucinations and euphoria/dysphoria (Papaleontiou et al., 2010). Opioids can also increase the risk of falls in older adults, by either increasing sedation or causing dizziness from orthostatic hypotension. These reactions are especially common in elderly patients recovering from surgery, perhaps because of opioid side-effects being magnified by the residual effects of the general anesthetic, and because of the disorientation and wooziness that often occur after surgery.
Table 12.1
Analgesic and anti-inflammatory medications
| Category | Common Examples | |
| Generic Name | Trade Name | |
| Opioid analgesics | Hydromorphone | Dilaudid, others |
| Meperidine (pethidine) | Demerol | |
| Morphine | Many trade names | |
| Oxycodone | OxyContin, others | |
| Propoxyphene | Darvon | |
| Non-opioid analgesics | Aspirin | Many trade names |
| NSAIDs | Ibuprofen | Advil, Motrin, others |
| Ketoprofen | Orudis, others | |
| Ketorolac | Toradol | |
| Meloxican | Mobic | |
| Naproxen | Aleve, others | |
| Piroxicam | Feldene, others | |
| COX-2 inhibitors | Celecoxib | Celebrex |
| Acetaminophen | – | Tylenol, others |
| Glucocorticoids | Betamethasone | Celestone |
| Dexamethasone | DexPak | |
| Hydrocortisone | Cortef, others | |
| Methylprednisolone | Medrol, others | |
| Prednisolone | Prelone, others | |
| Prednisone | Sterapred | |
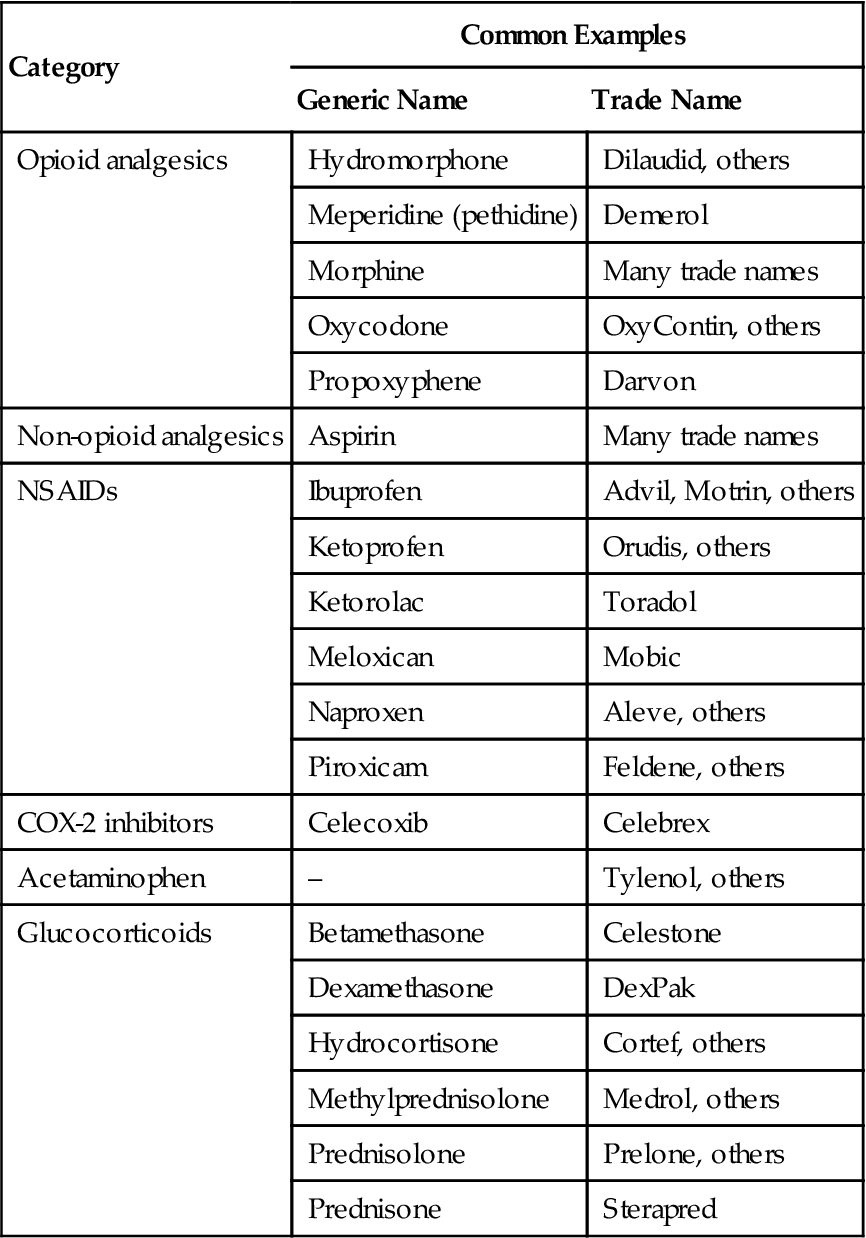
COX-2, cyclooxygenase type 2; NSAIDs, nonsteroidal anti-inflammatory drugs
Non-opioid analgesics
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the primary group of non-opioid analgesics. NSAIDs include aspirin, ibuprofen and similar agents (see Table 12.1), and these drugs are often effective in treating mild to moderate pain. These medications actually produce four clinically important effects: decreased pain, decreased inflammation, decreased fever and decreased blood coagulation. There is also considerable evidence that NSAIDs may decrease the risk of certain cancers, including colorectal cancer. All of these effects are mediated through inhibition of the biosynthesis of lipid compounds called prostaglandins. Certain prostaglandins mediate painful sensations by increasing the nociceptive effects of bradykinin. NSAID-mediated inhibition of prostaglandin synthesis therefore helps reduce painful sensations in a variety of clinical conditions. The primary problem associated with NSAIDs is gastrointestinal distress, including gastric irritation and ulceration. These medications may also cause damage to the liver and kidneys, especially in older adults who have preexisting hepatic or renal dysfunction.
In addition to traditional NSAIDs, newer drugs known as COX-2 inhibitors have been developed (Gatti & Adami, 2010). These drugs are so named because they inhibit the cyclooxygenase (COX)-2 enzyme that synthesizes prostaglandins during pathological conditions. The COX-2 enzyme synthesizes prostaglandins that cause pain, inflammation and other harmful effects, whereas the COX-1 enzyme synthesizes prostaglandins that are beneficial and often help protect various tissues and organs. Whereas traditional NSAIDs (e.g. aspirin, ibuprofen) inhibit both isoforms of the COX enzyme, the COX-2 drugs are designed to inhibit only the production of harmful prostaglandins (reducing pain and inflammation) while sparing the production of beneficial prostaglandins in the stomach, kidneys, and other organs and tissues. Indeed, the incidence of gastric problems is lower with COX-2 drugs, and some older adults have used these drugs successfully for extended periods to treat osteoarthritis and similar problems with minimal side-effects. The COX-2 drugs, however, may also produce serious cardiovascular problems including heart attack and stroke in susceptible patients. Hence, these drugs should be avoided in those at risk for cardiovascular disease (Gatti & Adami, 2010). Currently, celecoxib (Celebrex) is the only COX-2 drug that remains on the market, and this drug must be used cautiously when treating pain in older adults.
Acetaminophen (paracetamol), the active ingredient in Tylenol and other products, is another type of non-opioid analgesic. This agent is different from the NSAIDs in that it does not produce any appreciable anti-inflammatory or anticoagulant effects. Likewise, acetaminophen does not produce gastrointestinal irritation, but this medication can cause severe hepatotoxicity in those with liver disease or after an overdose.
Anti-inflammatory medications
Treatment of inflammation consists primarily of the NSAIDs and anti-inflammatory steroids. As indicated earlier, NSAIDs inhibit the synthesis of prostaglandins, and this inhibition reduces the proinflammatory effects of certain prostaglandins. NSAIDs tend to be effective in treating a variety of conditions that exhibit mild to moderate inflammation. More severe inflammatory conditions often require the use of anti-inflammatory steroids known as glucocorticoids. Medications such as hydrocortisone and prednisolone (see Table 12.1) inhibit a number of the cellular and chemical aspects of the inflammatory response, often producing a dramatic decrease in the symptoms of inflammation. However, glucocorticoids cause many severe side-effects including breakdown of collagenous tissues, hypertension, glucose intolerance, gastric ulcer, glaucoma and adrenocortical suppression. Tissue breakdown (catabolism) can cause severe muscle wasting and osteoporosis, especially in older people who may already be somewhat debilitated.
Psychotropic medications
Antianxiety drugs
Treatment of anxiety has traditionally consisted of benzodiazepines, including diazepam and similar agents (Table 12.2) (Rheinhold et al., 2011). These drugs work by increasing the inhibitory effects of gamma-aminobutyric acid (GABA), an endogenous neurotransmitter, in areas of the brain that control mood and behavior. The primary side-effect of benzodiazepine agents is sedation. These drugs may also cause tolerance and physical dependence when used continually for prolonged periods (more than 6 weeks). Benzodiazepines also have extremely long metabolic half-lives in older adults, which means that it takes a very long time to metabolize and eliminate these drugs. As a result, benzodiazepines can accumulate in older patients and reach toxic levels, shown by symptoms of confusion, slurred speech, dyspnea, incoordination and pronounced weakness.
Table 12.2
| Category | Common Examples | |
| Generic Name | Trade Name | |
| Antianxiety drugs | ||
| Benzodiazepines | Alprazolam | Xanax |
| Chlordiazepoxide | Librium, others | |
| Diazepam | Valium | |
| Lorazepam | Ativan | |
| Oxazepam | Serax, others | |
| Azapirones | Buspirone | Buspar |
| Antidepressants | ||
| Tricyclics | Amitriptyline | Elavil, others |
| Amoxapine | Asendin | |
| Doxepin | Sinequan, others | |
| Imipramine | Tofranil, others | |
| Nortriptyline | Pamelor, others | |
| Trimipramine | Surmontil | |
| MAO inhibitors | Isocarboxazid | Marplan |
| Tranylcypromine | Parnate | |
| Second-generation drugs | Buproprion | Wellbutrin |
| Citaloprama | Celexa | |
| Desvenlafaxineb | Pristiq | |
| Escitaloprama | Lexapro | |
| Duloxetineb | Cymbalta | |
| Fluoxetinea | Prozac | |
| Maprotiline | Ludiomil | |
| Paroxetinea | Paxil | |
| Sertralinea | Zoloft | |
| Venlafaxineb | Effexor | |
| Antipsychotics | ||
| Aripiprazolec | Abilify | |
| Chlorpromazine | Thorazine | |
| Clozapinec | Clozaril | |
| Haloperidol | Haldol | |
| Olanzapinec | Zyprexa | |
| Prochlorperazine | Compazine, others | |
| Quetiapinec | Seroquel | |
| Risperdonec | Risperdal | |
| Thioridazine | Mellaril | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







