Current Concepts and Techniques in Foot and Ankle Surgery
Antithrombotic Pharmacologic Prophylaxis Use During Conservative and Surgical Management of Foot and Ankle Disorders: A Systematic Review
Keywords
• Deep venous thrombosis • Low molecular weight heparin • Pulmonary embolism • Venous thromboembolism
There are currently no widely accepted standardized guidelines regarding the use of antithrombotic pharmacologic prophylaxis during conservative or postoperative management of foot and ankle disorders. Recommendations range from providing antithrombotic pharmacologic prophylaxis to high-risk patients only to providing no prophylaxis at all based on the low reported incidence of clinically significant deep venous thrombosis (DVT) and pulmonary embolus (PE) associated with conservative or postoperative management of foot and ankle disorders.1–16 The current guidelines from the American College of Chest Physicians (ACCP) are not specific to foot and ankle disorders and instead address isolated injuries of the lower extremity, defined as any tendinous or osseous injury occurring distal to the knee.17 In this guideline, data were reviewed from 6 randomized clinical trials, 2 focused on conservative management of lower extremities injuries and the incidence of DVT/PE and 4 focused on the postoperative management of below-knee fracture open reduction and internal fixation (ORIF) and surgical repair of Achilles tendon rupture and the incidence of DVT/PE. The pooled data demonstrated that patients with lower extremity injuries had a 10% to 45% risk of developing an asymptomatic DVT. Risk factors associated with the development of DVT/PE were found to be older age, surgical intervention, obesity, fractures, and Achilles tendon ruptures. The use of low molecular weight heparin (LMWH) was found to reduce the frequency of asymptomatic DVT, particularly in cases of surgical repair of Achilles tendon rupture. However, as these trials only addressed asymptomatic DVT/PE, it was determined that the results could not be extrapolated to clinically significant DVT/PE. The cost-effectiveness of providing antithrombotic pharmacologic prophylaxis for isolated lower extremity injuries was not reported. Based on these considerations, the ACCP does not currently recommend the use of routine antithrombotic pharmacologic prophylaxis for injuries of the lower extremity distal to the knee.
This is in contrast with the current protocol of the authors that involves administration of antithrombotic pharmacologic prophylaxis in the form of a weight-based prophylactic dose of heparin (5000 international units twice or 3 times a day) while patients are hospitalized and the use of a prophylactic dose of LMWH (40 mg Lovenox once daily) on discharge, which is administered until the patient is fully ambulatory. The use of mechanical prophylaxis in the form of sequential compression devices is also used while patients are hospitalized, and compression stockings for the contralateral limb during the recovery period. All patients treated by the authors are considered moderate to high risk because of the presence of evidenced-based risk factors for the development of DVT/PE including advanced age, increased body weight, presence of varicose veins, and after lower extremity surgery being performed under general anesthesia (Box 1).18–20 Despite the use of pharmacologic and mechanical antithrombotic prophylaxis, the authors have experienced the formation of DVT leading to PE, which was a near-fatal event in 1 patient and a fatal event in another.21 Given our standard protocol for antithrombotic pharmacologic and mechanical prophylaxis and the controversy that remains regarding administration of antithrombotic pharmacologic prophylaxis during treatment of foot and ankle disorders, a systematic review was undertaken to determine the incidence of DVT/PE during conservative or postoperative management of traumatic injuries or elective surgery of the foot and ankle in patients who did or did not receive antithrombotic pharmacologic prophylaxis for any portion of the recovery period, as well as to determine whether antithrombotic pharmacologic prophylaxis reduces the incidence of either asymptomatic or symptomatic DVT/PE.
Box 1 Risk factors for postoperative DVT
Risk factors with evidence showing a significant association are in bold type.
Materials and methods
Eleven electronic databases, including the American College of Physicians Journal Club (http://www.acpjc.org/), Cumulative Index of Nursing and Allied Health Literature (http://www.ebscohost.com/cinahl/), Cochrane Collaboration Library (http://www.thecochranelibrary.com/view/0/index.html?CRETRY&;), Cochrane Controlled Trials Register (http://www.ovid.com/site/products/ovidguide/cctrdb.htm), The Cochrane Collaboration Cochrane Reviews (http://www.cochrane.org/reviews/), Cochrane Methodology Register (cmr.cochrane.org), Center for Reviews and Dissemination (http://www.crd.york.ac.uk/crdweb/Home.aspx?DB=DARE), The Cochrane Library (http://mrw.interscience.wiley.com/cochrane/cochrane_clhta_articles_fs.html), Infotrieve-PubMed/MEDLINE (http://www4.infotrieve.com/newmedline/search.asp), and Ovid MEDLINE(R) In-Process and other nonindexed citations (http://www.ovid.com/site/products/ovidguide/medline.htm) were searched from inception to July 2010. The search was restricted to the English language with no restriction on date using an inclusive text word query for “foot” AND “ankle” AND “immobilization” OR “cast” OR “orthosis” AND “surgical” OR “nonsurgical” AND “deep venous thrombosis” OR “pulmonary embolism” OR “thromboembolism” AND “prophylaxis” OR “thromboprophylaxis” OR “low molecular weight heparin” with the words in all upper case representing the Boolean operators used. To maximize the number of potentially useful references, every combination of text words was queried through each of the electronic databases. In addition, an Internet-based general interest search engine, specifically Google (http://www.google.com/), was used to identify available sources that could potentially provide useful information, by using various combinations of the text words listed earlier. References from each manuscript identified were hand searched to identify any pertinent material for review that was not identified from the electronic searches. If a reference could not be obtained through purchase, librarian assistance, or email contact with the author, it was excluded from consideration. Studies were eligible for inclusion if they were prospective studies, randomized or nonrandomized, with consecutive enrollment of subjects undergoing conservative treatment or postoperative management of traumatic injuries or elective surgery of foot and ankle disorders that received either antithrombotic pharmacologic prophylaxis for any portion of the treatment period, placebo, or were untreated for thrombotic events. Diagnosis of DVT had to have objective confirmation with either duplex ultrasonography (DUS) showing a noncompressible lumen or ascending phlebography showing a segment-filling defect on 1 or more views. A proximal DVT was defined as a thrombosis occurring within or proximal to the popliteal vein. A distal DVT was defined as a thrombosis occurring distal to the popliteal vein. The diagnosis of PE had to have objective confirmation with either a computed tomography pulmonary angiogram or ventilation/perfusion scan for inclusion in analysis (Box 2). The incidence of major or minor bleeding complications was assessed when reported but was not a requirement for inclusion in analysis.
Results
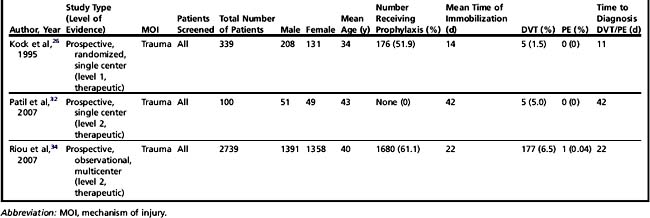
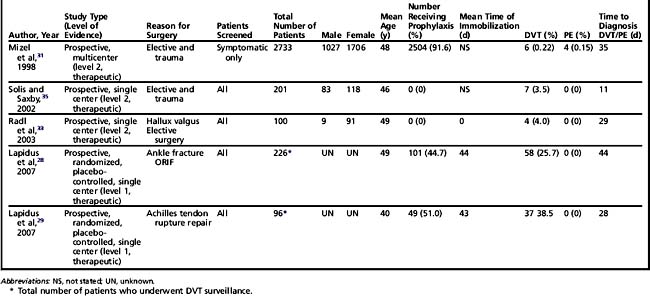
The search for potentially eligible information for inclusion in the systematic review yielded a total of 36 publications. All publications were obtained and reviewed in their entirety by the authors in July 2010. On completion of review, 15 publications were determined potentially eligible for inclusion in analysis.22–36 Detailed review of these references revealed that 1 reference was a quasi-systematic review, 1 reference was a meta-analysis with different study inclusion parameters, and 1 reference was a response to another study for further clarification of the data presented in the study.22–2430 In addition, 4 references did not meet the inclusion criteria because of the inability to determine whether the trauma sustained was localized to the foot and ankle or included injuries of the proximal lower leg (ie, tibial plateau fractures).25,27,30,36 This left 8 publications (22.2%) that met all the inclusion criteria.26,28,29,31–35 Three were related to the use of antithrombotic pharmacologic prophylaxis during conservative management of traumatic foot and ankle injuries and 5 were related to the use of antithrombotic pharmacologic prophylaxis during the postoperative management of elective surgery and surgical repair of traumatic foot and ankle injuries (Tables 1 and 2).
Conservative treatment
There were a total of 339 patients in the study by Kock and colleagues,26 with 176 patients receiving 32 mg LMWH (specific medication not stated) daily by subcutaneous injection and the remaining 163 patients being untreated (see Table 1). The duration of antithrombotic pharmacologic prophylaxis was not mentioned. Injuries were classified as grade II strains and bruises, grade III strains, fractures, or others. All were treated with a below-knee cast with weight-bearing status not mentioned. The mean immobilization time was 11 (range 1–29) days in the treatment group and 17 (range 1–76) days in the untreated control. All patients were screened using DUS for DVT at the time of cast removal. All DVT diagnosed with DUS were confirmed with ascending phlebography. Although the injuries could not be specifically localized to the foot and ankle, 5 of the 7 DVT reported occurred in patients who sustained trauma to the foot or ankle (ie, 1 fracture of the hallux, 1 fracture of the fifth metatarsal, 1 contusion of the ankle, 1 tear of an ankle ligament, and 1 severe distortion of the ankle). All DVT occurred in the untreated control group. Of these 5 DVT, 2 were proximal and 3 were distal. Proximal DVT occurred in the patients who sustained the fracture of the hallux and the tear of an ankle ligament. It was not stated whether any of the DVT were symptomatic. No PE were reported. The mean age of the patients with a DVT was 55 (±6.7) years (range, 47–60 years). The mean time to diagnosis of DVT was 11 (range 1–29) days. All DVT occurred in patients greater or equal to 40 years old in below-knee cast immobilization, with some patients having undergone immobilization for less then 10 days. There were no major bleeding complications reported. Five minor complications were reported consisting of 4 small local hematomas at the injection site and 1 incidence of facial eczema.
The study by Patil and colleagues32 focused on conservative treatment of ankle fractures with cast immobilization (see Table 1). The mean time of immobilization was 42 (range 21–49) days, which was the longest mean immobilization time of all 3 studies included in our systematic review of conservative treatment of traumatic injuries of the foot and ankle. None of the patients received antithrombotic pharmacologic prophylaxis. All patients were screened for DVT using DUS at the time of cast removal. A total of 5 DVT occurred with 3 being distal and 2 being proximal. All DVT were asymptomatic. There was no PE reported. The mean age of those who developed a DVT was 50 (range 18–69) years. Four of the 5 patients had a body mass index (BMI) greater than 28. Three of the 5 patients had a current tobacco use history. All patients with a DVT were allowed to bear full weight in their cast during treatment. No minor or major bleeding complications were reported.
Riou and colleagues34 provide the largest number of patients in their prospective, multicenter observational study (see Table 1). Administration of antithrombotic pharmacologic prophylaxis was not standardized but based on the discretion of the treating emergency room physician due to the concern for potential development of DVT/PE. The 4 risk factors found to be the most influential for prompting the treating emergency room physician to start antithrombotic pharmacologic prophylaxis was the need for cast immobilization, the requirement for non–weight-bearing, and severe or moderate injury. A total of 1680 patients received antithrombotic pharmacologic prophylaxis (specific medication not stated), and 1059 patients received no prophylaxis. As administration of antithrombotic pharmacological prophylaxis was at the discretion of the treating emergency room physician and not standardized, the type prescribed was not reported. Antithrombotic pharmacologic prophylaxis continued for the entire period of immobilization with a mean immobilization time of 22 days. All patients were screened for DVT using DUS on completion of their immobilization period. There were a total of 177 (6.4%) DVT reported with 172 being distal and 5 being proximal. One DVT progressed to a PE (0.04%). There were 27 (15.3%) symptomatic DVT. The study found that the risk factors prompting antithrombotic pharmacologic prophylaxis were accurate for predicting patients at high risk for developing DVT/PE. Age greater than 50 years was found to be an additional risk factor for the potential to develop DVT/PE. Obesity, previous history of DVT/PE, family history of DVT/PE, and malignancy could not be assessed as potential risk factors for DVT/PE because of the small proportion of patients with these factors included in the study. The study could not assess the protective role of antithrombotic pharmacologic prophylaxis; however, the investigators believed that the role of antithrombotic pharmacologic prophylaxis was favorable because of the low reported incidence of DVT/PE. No minor or major bleeding complications were reported; however, the investigators stated that complications related to the use of antithrombotic pharmacologic prophylaxis were low and not usually severe. The investigators suggested that the risk-versus-benefit potential weighted favorably for the use of antithrombotic pharmacologic prophylaxis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree