(1)
Department of Orthopedic Surgery Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands
Abstract
Tendoscopy of the peroneal tendons is a useful tool to diagnose and treat peroneal tendon disorders. Diagnosis of a length rupture of the peroneal tendons remains one of the main indications. Synovectomy, adhesiolysis, and removal of an exostosis can be performed endoscopically with low morbidity and an excellent functional outcome. In this chapter, the anatomy, pathology, indications, and surgical technique are described.
Posterolateral ankle pain most often is caused by disorders of the peroneal tendons.
The main indications for peroneal tendoscopy are synovectomy and adhesiolysis.
Diagnosis of a suspected (length) rupture of the peroneal tendons is another main indication for peroneal tendoscopy.
23.1 Introduction
In the absence of intra-articular pathology, posterolateral ankle complaints most often are caused by disorders of the peroneal tendons. In the event of failure of conservative treatment, disorders like tenosynovitis, partial tendon rupture, hypertrophic tendinopathy, and a prominent peroneal tubercle can be treated by open surgery.
Postoperative open surgical treatment requires plaster immobilization to prevent equinus malformation and to stimulate wound healing (Lapidus and Seidenstein 1950; Richardson 1993). An endoscopic procedure offers several advantages such as less morbidity, reduction in postoperative pain, functional aftertreatment, and outpatient treatment (Van Dijk et al. 1997; de Leeuw et al. 2009). A cadaver study was performed, and subsequently, in a prospective study, diagnostic and therapeutic tendoscopy (tendon sheath endoscopy) was performed.
23.2 Pathology
Lateral ankle pain is a problem seen very frequently, usually after a traumatic event. Peroneal tendon pathology is not always recognized as a cause of lateral ankle pain. Peroneal tendon disorders are often associated and secondary to chronic lateral ankle instability. As the peroneal muscles act as lateral ankle stabilizers, more strain is placed on these tendons in chronic lateral ankle instability resulting in hypertrophic tendinopathy, tenosynovitis, and ultimately in (partial) tendon tears (Yao et al. 1995; Myerson 1992; Richardson 1992). Diagnosis may be difficult in a patient with lateral ankle pain. Peroneal tendon dislocation and tenosynovitis can be established by means of physical examination (Fig. 23.1). In case of (subtotal) tears of peroneus brevis or longus tendon, supplemental investigations like MRI and sonography are helpful in confirming the diagnosis (Yao et al. 1995). Postsurgery and posttraumatic adhesions and irregularities in the posterior aspect of the fibula (i.e., tendon sliding channel) can be responsible for symptoms in this region as well (Reilingh 2010 a, b).


Fig. 23.1
Palpation of the peroneal tendons. (a) Palpation at the insertion of the peroneus brevis at the basis of the fifth metatarsal. (b) Palpation of the peroneal tendons distal from the lateral malleolus. (c) Palpation of the peroneal tendons behind the lateral malleolus
Pathology of the peroneal tendons consists of tenosynovitis of the peroneal tendons, tendon dislocation or subluxation, (partial) rupture, and snapping of one or both of the peroneal tendons. They account for the majority of symptoms at the posterolateral side of the ankle joint (Roggatz and Urban 1980; Schweitzer 1982). Rheumatoid tenosynovitis or a bony spur also can cause posterolateral ankle pain. A differentiation must be made with (fatigue) fractures of the fibula, lesions of the lateral ligament complex, and posterior impingement of the ankle (os trigonum syndrome).
23.3 Anatomic Study
Seven ankles in five specimens with no previous history of ankle pathology were dissected. Special attention was paid to the relation of the peroneal tendons to each other, to the posterolateral aspect of the distal fibula, and to the lateral bony aspects of the calcaneus and cuboid.
A consistent (seven of seven) membranous mesotendineal structure was found between both tendons and tendon sheath (Fig. 23.2). This thin vincula-like structure runs between the peroneus longus and the peroneus brevis tendon and is dorsally attached to the dorsolateral aspect of the fibula. When stretched out, it provides an intertendinous distance of 3–4 cm. The distal fibers of the peroneal brevis muscle belly gradually transform to this membranous layer to end approximately at the tip of the fibula. This vincula runs all the way down to the distal insertion of the tendons. The vascularization of the tendons depends on their vincula (Fig. 23.3). Proximal to the lateral malleolus, the peroneus brevis tendon has a flat contour. Just distal to the tip of the lateral malleolus, the tendon becomes round and crosses around the peroneus longus tendon. The posterolateral part of the fibula constitutes a sliding channel for the two peroneal tendons. In three of the seven explorations, the bony prominence on the calcaneus was found in between both tendons, some 4–5 cm distal from the tip of the fibula.
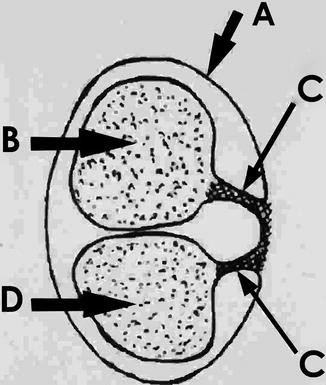
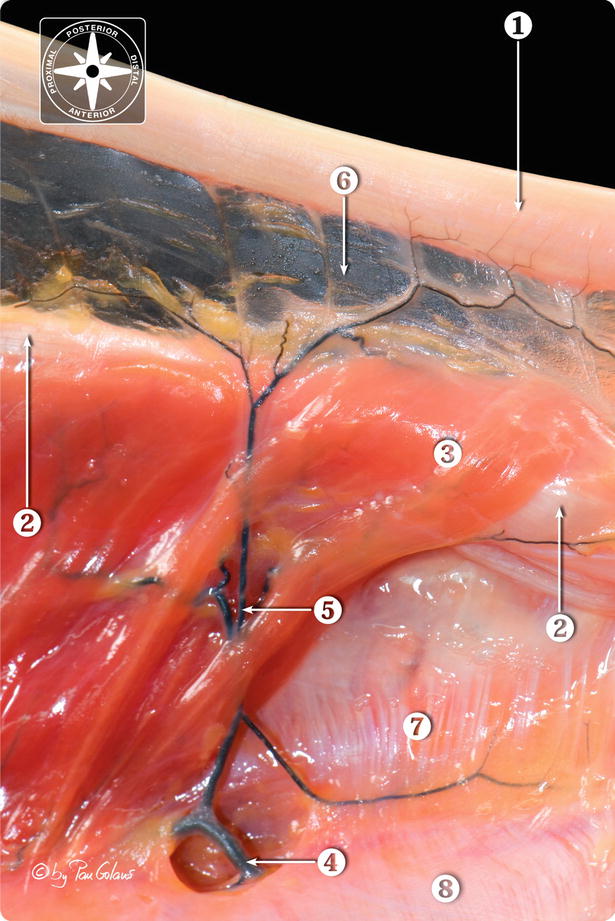
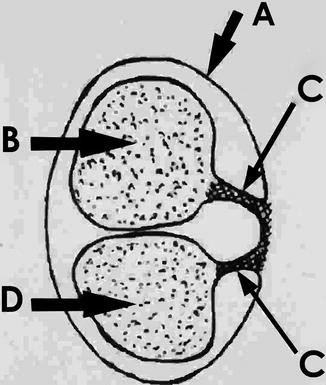
Fig. 23.2
Schematic drawing of a cross section of the peroneal brevis (B) and longus (D) tendons with their vincula (C) and tendon sheath (A)
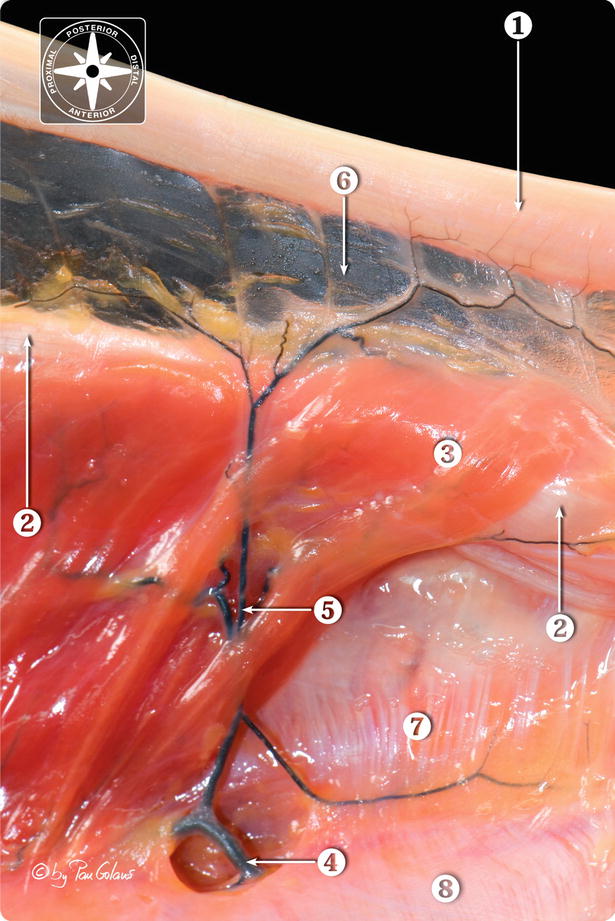
Fig. 23.3
Photomacrography of the peroneal tendons vincula/mesotendon at the level of retromalleolar area. In this lateral view, the peroneal tendons were displaced from its original position. 1 Peroneus longus tendon, 2 peroneus longus brevis tendon, 3 peroneus brevis muscle belly, 4 peroneal artery, 5 artery of the vincula/mesotendon, 6 vincula/mesotendon, 7 floor of the peroneal tendon sheath, 8 posterolateral intermuscular septum (displaced) (With kind permission of © Pau Golanó 2013)
23.4 Surgical Technique
An anatomical study was performed to verify portal relations. Access to the tendon can be obtained anywhere along its course (Van Dijk et al. 2010). However, the two main portals are located directly over the tendons 2 cm distal and 2 cm proximal of the posterior edge of the lateral malleolus (Fig. 23.4). The distal portal is made first: The incision is made through the skin only and the tendon sheath is penetrated by the sleeve with a blunt trocar. The 2.7-mm arthroscope with an inclination angle of 30° is introduced and the tendon sheath is filled with saline. The 1-mm needle scope and the 1.8-mm arthroscope were used at first but were found to give inferior access and view. Another important advantage of the 2.7-mm arthroscope is the better flow which is necessary when surgery is undertaken.
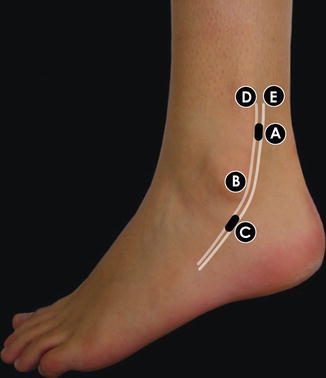
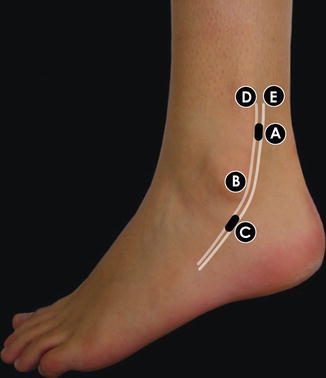
Fig. 23.4
Left ankle: the two main portals are located directly over the peroneal tendons 2 cm distal and 2 cm proximal to the posterior edge of the lateral malleolus. (A proximal portal, B lateral malleolus, C distal portal, D peroneus longus tendon, E peroneus brevis tendon)
Under direct vision, the proximal portal is made by introduction of a spinal needle and subsequently an incision is made through the skin into the tendon sheath. Instruments like a blunt probe, scissors, retrograde knife, and shaver system can be introduced. The distal portal allows a complete overview over both tendons from 6 cm above the level of the posterior tip of the lateral malleolus (Fig. 23.5). Distally, at the level of the peroneal tubercle, both tendons separate and get surrounded by their own tendon sheath. Both tendons and tendon sheath are inspected by rotating the scope around the tendons.
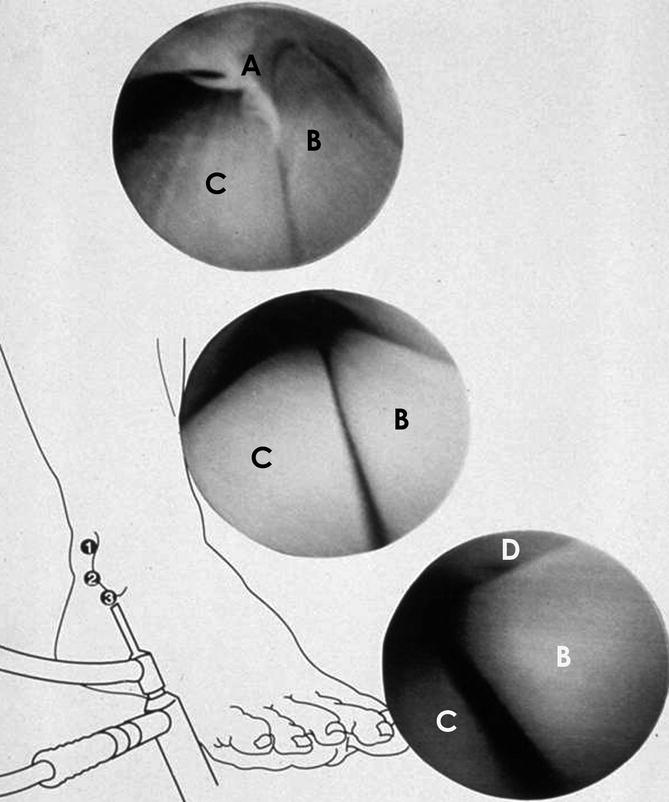
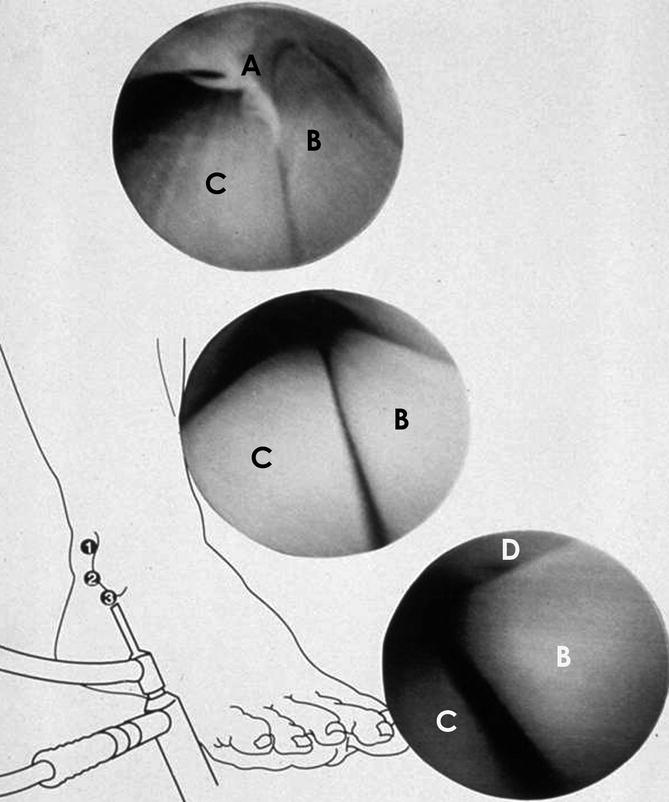
Fig. 23.5




Arthroscopic appearance of the anterior aspect of both peroneal tendons of the right ankle. (1) Proximal view: the vincula which attaches both tendons to the tendon sheath, arises from the posterior surface of both tendons (not visible here). More proximally, both tendons get separated by a membrane. Above this level both tendons have their own tendon sheath. (2) Middle view: both tendons are located in the same tendon sheath. The vincula are posteriorly located and therefore not visible in this picture. (3) Distal view: more distally, both peroneal tendons curve around the tip of the lateral malleolus in the sliding channel. (A free edge of the tendon; sheath membrane between both tendons, B peroneal brevis tendon, C peroneal longus tendon, D lateral malleolus)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








