Perilunate Dislocations
12.1 Introduction
The classic mechanism of a fall on an outstretched hand can produce a variety of injuries from the distal forearm to the finger tip. Location and severity of the resultant injury depend on the magnitude and direction of the force applied to the hand and wrist.
Perilunate dislocations and fracture-dislocations constitute a rare but potentially serious wrist injury pattern1 that is particularly important as it tends to occur in young people and may lead to considerable long-term morbidity due to the development of radiocarpal arthritis, carpal instability, or median nerve damage.2 The typical mechanism was experimentally evaluated by Mayfield and colleagues and is characterized by hyperextension combined with high-energy trauma. Numerous activities include the risk of such high-energy forces that take effect on the hand and wrist. Typical associated actions are sporting, motor vehicle, and industrial accidents, as well as falls from a height.3 The transmission of force through the wrist at the time of the trauma will dictate the path of damage that results in a spectrum of possible injury patterns.4 The direction of the dislocation in perilunate injuries is predominantly dorsal and about two-thirds of perilunate injuries are associated with fractures (mostly scaphoid fractures).5 The resulting fracture patterns present reconstructive challenges to the hand surgeon. Median nerve contusion and acute carpal tunnel compression are commonly associated with these injuries. Treatment of median nerve pathology plays a significant role in the choice of treatment of the underlying perilunate injury.
A considerable proportion of perilunate dislocations are missed initially.6,7 Forty-one of 166 patients sustaining these injuries reviewed in a multicenter study were missed at initial presentation.5 Since delayed treatment results in significantly worse outcomes, missed perilunate injuries may significantly alter outcome and quality of life.
12.2 Historical Perspective
Joseph Francois Malgaigne first described “perilunate dislocations” in 1855 (reviewed by Kardashian et al3). Different treatment regimens with closed and open reductions have been proposed to treat perilunate injuries since then.8 Initially, the treatment of choice was closed reduction and casting. In 1923, Davis inaugurated a technique using a broomstick as a fulcrum on the palmar aspect of the wrist to reduce the lunate in its fossa.9 This technique was subsequently modified using the thumb as a fulcrum in order to reduce soft tissue damage.10 However, the risk of secondary dislocation as well as nonunion in fracture-dislocations is significantly increased after closed reduction in comparison with open techniques.8 Therefore, open reduction and internal fixation has become the mainstay of treatment.8 Current improvements in the treatment of perilunate injuries have led to more detailed discussions concerning surgical correction and fixation.3
12.3 Anatomy
The wrist is characterized by complex anatomy and a highly functional structural joint. It represents the anatomical bridge between forearm and hand.11 The eight bones of the carpus and the distal ends of the radius and ulna form a complex joint that allows significant multiplanar mobility of the wrist in both flexion/extension and radial/ulnar deviation.12 In addition, the carpus maintains stability during supination and pronation. To have such mobility while also maintaining relative stability, the wrist has a complex configuration and precise interaction of several rows of individual bones, stabilized by multiple critical ligaments.11 The osseous linkage between the forearm and the bones of the hand occurs through the eight bones of the wrist. The articulation of the distal row to the metacarpals is extremely stable and the mobility of the wrist, for the most part, occurs in the proximal carpal row. In addition to the osseous architecture, carpal stability is maintained by the complex configuration of ligaments linking the bones dorsally and palmarly. With respect to the lunate, the carpus is anchored within the lunate fossa of the distal radius by palmar and dorsal intercarpal (intrinsic) and extracarpal (extrinsic) ligaments. Important interosseous ligaments around the lunate are the scapholunate (SL) ligament and lunotriquetral (LT) interosseous ligament. The dorsal extrinsic ligaments are thin, are few in number, and are functionally and structurally reinforced by the floor and septi of the fibrous extensor tendon tunnels.11 The palmar extrinsic ligaments form two V-shaped almost parallel structures with the apices pointing distally. The capitate is the apex distally, and the lunate is the apex proximally. The space between these two complexes forms an inherently weak area, termed the “space of Poirier,” that is often involved in perilunate dislocations.13 Malfunction of the wrist occurs when the structural alignment of the bones has changed or when the ligamentous constraints have been disrupted.
12.4 Classification
Perilunate dislocations represent approximately 10% of all wrist injuries and are diagnosed late in up to 25% of cases. The mechanism of injury is typically a high-energy impact onto an outstretched hand and results in energy transmission to the wrist. Herzberg described three different time frames regarding the onset of treatment. The acute phase is defined as onset of treatment within the first week; the delayed phase is the period between the 7th and the 45th day; and after 45 days the injury is considered to be in the chronic phase.5
The mechanism of perilunate dislocations is a progressive pattern of carpal ligamentous injuries caused by wrist hyperextension and ulnar deviation. This leads to distinct stages of perilunate injuries that were first observed and described by Mayfield and colleagues in the 1980s based on his experimental biomechanical studies14 (▶ Table 12.1, ▶ Fig. 12.1). Mayfield described four stages, with each stage representing a sequential intercarpal injury beginning with scapholunate joint disruption and proceeding around the lunate, creating progressive ligamentous injury and progressive carpal instability.14 Each stage of dislocation may also be associated with specific bony fractures, which if present should alert the physician to the possibility of an occult perilunate ligamentous injury. These associated fractures include fractures of the radial styloid, scaphoid, capitate, and triquetrum.
Stages | Injury |
1 | Rotational dislocation of the scaphoid, LC-joint intact |
2 | Stage 1 with additional subtotal dislocation of capitate and lunate; rupture of the radioscaphocapitate ligament |
3 | Stage 2 with additional lunotriquetral instability or fracture of the triquetrum |
4 | Palmar dislocation of the lunate |

Fig. 12.1 In Mayfield stage 1 to stage 3 injuries the lunate is maintained in the lunate fossa of the radius, whereas the lunate dislocates palmarly in stage 4 injuries.4 (Reprinted from Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am 1980;5:226–241 with permission from Elsevier.)
In Mayfield stage 1 injuries, the force travels between the scaphoid and lunate bones. This energy transmission disrupts the scapholunate ligament and then exits along the midcarpal joint. Mayfield stage 2 injuries result when transmission of force disrupts capitolunate attachments and disrupts the radioscaphocapitate ligament, leading to dislocation of the capitate from the lunate with the lunate remaining in normal position within the lunate fossa of the radius. Such a dislocation is limited in part by the radioscaphocapitate ligament. The Mayfield stage 3 injury appears similar to a stage 2 injury but with the addition of a dislocation of the triquetrum. It occurs due to further extension when energy passes between the lunate and triquetrum, disrupting the lunotriquetral ligament. In all of stages 1 to 3, the lunate maintains its position in the lunate fossa of the radius. Finally, in Mayfield stage 4 injuries, a true lunate dislocation occurs as the lunate attachments to the scaphoid, capitate, and triquetrum are disrupted and the lunate dislocates from the lunate fossa (▶ Fig. 12.1).
In addition to Mayfield’s classification, Johnson, also in 1980, described the concept of “carpal arcs” of the wrist.15 The Mayfield staging of perilunate fracture dislocations is part of a spectrum of wrist trauma and injuries defined as “lesser arc” injuries.16 The dislocation pattern depends on the direction and path of the transmitted force through the carpus. Whereas lesser arc injuries (▶ Fig. 12.4 and ▶ Fig. 12.7) represent truly ligamentous injuries around the lunate, fracture-dislocations occur when the force is transmitted through the scaphoid rather than the scapholunate ligament. These injuries are referred to as greater arc lesions (▶ Fig. 12.3, ▶ Fig. 12.4, ▶ Fig. 12.5). As force passes through the scaphoid, it may then continue through ligamentous structures, creating a transscaphoid perilunate dislocation (Mayfield stage 2 or 3 equivalent fracture-dislocation). In rare cases there are mixed fracture-dislocation patterns.4 Such injuries do not conform to the lesser arc or greater arc force transmission patterns. Accordingly, Bain and colleagues denoted them translunate arc injuries, suggestive of a higher-velocity wrist injury.17 Their description encompasses all perilunate injuries with an associated translunate fracture pattern. These high-velocity wrist injuries lead to further destabilization of the carpus due to the need to first stabilize the lunate bone to itself and then to stabilize the remaining carpal bones to the lunate. Bain and colleagues suggest classifying perilunate injury patterns into three groups: greater arc (defined as any transosseous component), lesser arc (defined as purely transligamentous), and translunate arc (defined as any bony injury to the lunate).17

Fig. 12.2 Preoperative (a) and postoperative radiographs (b) of a patient with a lesser arc injury (Mayfield stage 3) that was treated by open reduction and internal fixation.
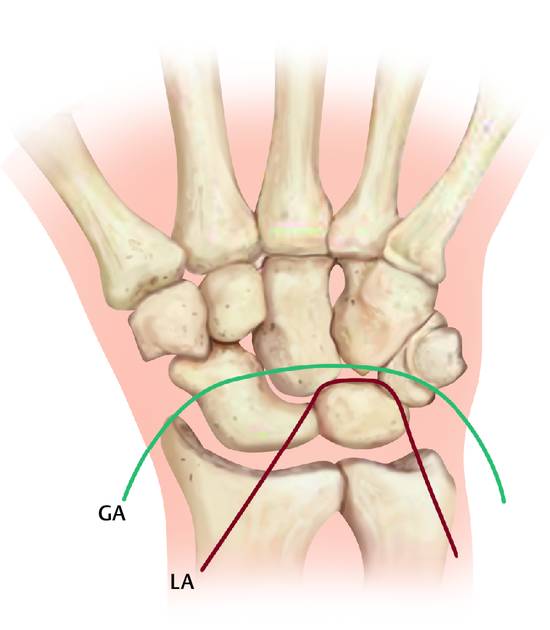
Fig. 12.3 The same patient as in ▶ Fig. 12.2 after 3 years: lateral view (a), PA view (b), and Stecher view (c). The patient showed excellent Mayo and Krimmer wrist scores (90 points) and a good DASH score of 8.33.

Fig. 12.4 Preoperative (a) and postoperative radiographs (b) of a patient with a lesser arc injury (Mayfield stage 3) that was treated by open reduction and internal fixation.

Fig. 12.5 (a and b) Perilunate injuries can be divided into pure ligamentous injuries (lesser arc injuries; LA) and perilunate fracture dislocations (greater arc injuries; GA). The fractures can include scaphoid, capitate, hamate, and triquetrum fractures. (Reproduced from Schmitt, R. and Lanz, U. Bildgebende Diagnostik der Hand; Stuttgart: Hippokrates Verlag; 1996 with kind permission from Hippokrates Verlag.)
12.5 Diagnosis
A detailed history of the injury is of utmost importance for the diagnosis of perilunate injuries. Frequent descriptions reveal typical high-energy traumas such as sporting accidents, falls from a height, or motorcycle accidents. Due to the high-energy trauma mechanisms, the physician should always consider concomitant injuries that may not be restricted to the upper extremity. According to Herzberg and colleagues, 26% and 11% of the patients suffering from perilunate injuries were observed with polytrauma and additional upper extremity injuries, respectively.5
Physical examination should focus on wrist stability, severity of injury, and nerve involvement. The presence of localized swelling over either the dorsum or the palmar aspect of the wrist and deformity at the level of the radiocarpal joint with significant pain on attempted limited range of motion are typical. The usual bony landmarks around the wrist may be obscured by swelling or completely lost due to the dislocation itself.3 Median nerve compression in the carpal tunnel is also frequently observed and should be addressed during the physical examination.
Standard radiographic imaging in standard PA and lateral views allow definitive diagnosis. However, correct diagnosis depends on adequate experience of the observer: this is reflected in the fact that perilunate injuries are frequently missed on conventional radiographs when the patient is not evaluated in a specialized hand trauma center. The “Gilula arcs” described by Gilula and colleagues may help in discovering carpal bony incongruities due to ligamentous and bony injuries in the wrist.18 (▶ Fig. 12.6). These lines outline respectively the proximal and distal margins of the proximal carpal row, and the proximal margin of the distal carpal row. Radiographs should be interpreted using these parallel curves. On the lateral radiograph, the first curve passes between the reciprocal convex and concave articular surfaces of the radius and lunate and is also demonstrated on an AP radiograph. A radiograph of transstyloid fracture dislocations clearly shows the disruption of this primary curve on both views. The second curve passes between the cup-shaped lunate and the head of the capitate on the lateral view and through the midcarpal joint on the AP view. This curve is clearly disrupted following perilunate dislocation and fracture-dislocations, and systematic analysis of the radiographs in this manner will allow easy identification of the injury even in an arthritic wrist.19
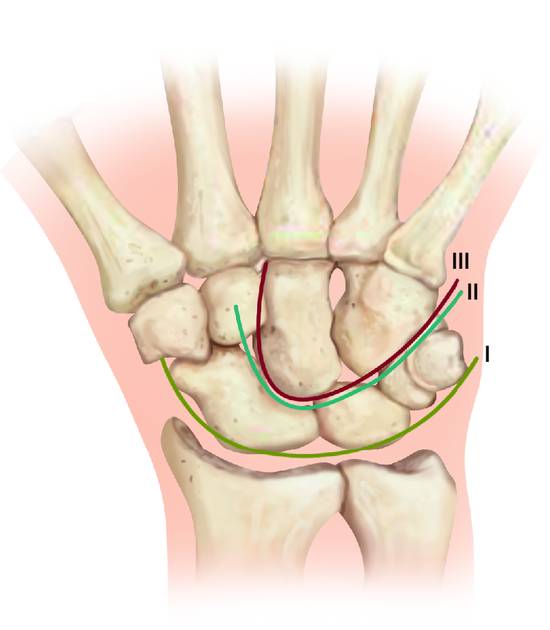
Fig. 12.6 If carpal integrity is maintained, three lines (according to Gilula) can be drawn along the proximal (I and II) and distal (III) carpal rows. These lines should be undisturbed and parallel. (Reproduced from Schmitt, R. and Lanz, U. Bildgebende Diagnostik der Hand; Stuttgart: Hippokrates Verlag; 1996 with kind permission from Hippokrates Verlag.)
In rare cases, computed tomography (CT) may be helpful, when perilunate injuries are associated with difficult bony fractures.3 Bain and colleagues note that CT scan may be useful to better characterize those carpal bone injuries.17 However, our group do not routinely apply CT scans since these may delay operative treatment. Magnetic resonance imaging (MRI) has no role in acute evaluations of perilunate injuries. CT and MRI image quality can be affected by the (in)ability to position the patient’s arm in the scanner.
12.6 Surgical Technique
12.6.1 Closed Reduction
Closed reduction should only be attempted in rare cases. However, we frequently use closed reduction methods to prepare the patient for an open reduction and internal fixation procedure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








