Lambotte’s 7 steps of fracture treatment have stood the test of time. Incision, preparation of the bone ends, reduction, temporary fixation, permanent fixation, closure, and dressing are modified to suit the needs of each fracture and each patient. One specific patient characteristic, obesity, has provided complex challenges in fracture care. This article reviews the challenges of obesity as they relate to the 7 steps of lower extremity periarticular fracture care. Specifically, helpful modifications to these 7 steps are provided for the treatment of tibial plateau fractures and tibial plafond fractures. As there is little published evidence with respect to the treatment of these injuries in the obese population, the suggestions that are provided are based on the extrapolation from published evidence of fracture care in other areas in patients with obesity, logic, and personal experience with fracture care in patients with obesity.
Lambotte’s 7 steps of fracture treatment have stood the test of time. Incision, preparation of the bone ends, reduction, temporary fixation, permanent fixation, closure, and dressing are modified to suit the needs of each fracture and each patient. One specific patient characteristic, obesity, has provided complex challenges in fracture care. This article reviews the challenges of obesity as they relate to the 7 steps of lower extremity periarticular fracture care. Specifically, helpful modifications to these 7 steps are provided for the treatment of tibial plateau fractures and tibial plafond fractures. As there is little published evidence with respect to the treatment of these injuries in the obese population, the suggestions that are provided are based on the extrapolation from published evidence of fracture care in other areas in patients with obesity, logic, and personal experience with fracture care in patients with obesity.
Steps of periarticular fracture care in patients with obesity
Incision (Including Positioning and Approach)
A surgical incision is a means to an end in fracture care. The desired ends include visualization of the fracture, preparation of the bone ends, reduction of the fracture, and fixation of the fracture. These ends need to be accomplished in the absence of wound healing complications. Obesity complicates reaching each of these ends. Modifications of the technique of the surgical incision are therefore useful.
Position must first be addressed as it allows access to the proposed location of the incision. Proper positioning of the patient begins at the operating room bed. Standard operating room beds may not be sufficient to allow for treatment of lower extremity periarticular fractures in the morbidly obese. Knowledge of the maximum weight allowance is necessary, which is provided in the technical specifications that come with the bed and is often listed on the bed itself. The location of the weight can be just as important as the amount of weight involved. Obesity takes different forms, and each form provides a different challenge. Truncal obesity leads to a significant shift in the patient’s center of gravity when rotational adjustments are made with the bed or bumps are placed under the hip. Overcoming the exaggerated lower extremity externally rotated resting posture in the patient with obesity is challenging and often requires these rotational adjustments to be made with the bed. This adjustment necessitates diligence before preparing and draping in placement of restraints to counteract the unwanted vectors that are created by bed rotation and shifts in the center of gravity. These restraints must distribute the force over a large area to limit the stress placed on the soft tissue envelope and thereby limit skin breakdown or neuropathies created through surgical positioning. Extra large belts and belt extensions are available and logically beneficial in this population. Using more than a single belt helps provide a second checkrein but should be balanced with the understanding that more pressure points are being created.
Once a bed with adequate weight allowance is chosen, modification of the bed to allow for increased width is often necessary. Thigh obesity creates an obligatory abduction at the level of the hips secondary to medial thigh abutment. This abduction increases the width of the bed required, as the limb extends distally. Once the ankles are reached, both feet may not be adequately supported. A published modification is to place an arm board distally, parallel to the long axis of the bed. Although increasing bed width, this modification comes at a cost. Many arm boards are not radiolucent, creating impairments in radiographic visualization when working at or distal to the knee. This situation can be remedied in single-extremity trauma by placing the arm board under the nonoperative extremity and moving the patient slightly toward the arm board in an effort to better center the injured extremity onto the radiolucent bed. Having the arm board slightly more elevated than the bed allows for a ramp effect to decrease the risk of the patient rolling off the bed. The arm board supplementation technique creates another issue that should be evaluated before beginning the procedure. C-arm machines vary in the diameter of the geometric arm. Increasing the width of the operative field may make moving from an anteroposterior to a lateral position for radiography challenging or even impossible. Even larger-diameter c-arms are taxed by increasing the width of the operative bed ( Fig. 1 ).

Once the patient is appropriately positioned and secured on a radiolucent bed of adequate dimensions and weight allowances, attention can be placed on preparing and draping. Intertriginous zones and folds must be aggressively cleansed ( Fig. 2 ). Personal hygiene can often be challenging in this population, and these folds have the potential to harbor bacterial contaminants that could create postoperative wound infections. Handling an unstable extremity during the preparation may require more than one assistant for the following reasons: (1) instability is magnified by the weight of the limb, (2) preparation time may be extended to cover the additional surface area, and (3) hoisting the extra weight of the limb can lead to premature exhaustion.

After adequate preparing and draping, the surgical approach is finally possible. As previously noted, a surgical incision is a means to an end in fracture care. The desired ends include visualization of the fracture, preparation of the bone ends, reduction of the fracture, and fixation of the fracture. These ends need to be accomplished in the absence of wound healing complications. Decisions are made by balancing desires with requirements. Doing so in periarticular fracture care in patients with obesity has led to 2 different strategies. First, larger approaches have been used to allow for adequate visualization and reductions, with the acceptance of increased wound healing complications. Second, limited incision approaches have been used in an effort to decrease wound healing complications but often at the expense of quality and construct stability. If the first approach is chosen, every care should be taken to limit wound healing complications through atraumatic soft tissue handling, careful closure, and even possibly wound healing enhancement techniques, such as use of incisional wound vacuum-assisted closure devices. If the second approach is chosen, special instrumentation, patience, and honing indirect reduction techniques should be the focus.
Preparation of the Bone Ends and Reduction
Each periarticular fracture can be divided into its component fractures: the articular fracture and the fracture that creates separation between the epiphysis and the diaphysis. The caveat to this rule is the partial articular fracture (eg, lateral tibial plateau fracture). These component fractures have different requirements and can be approached as such. It is generally accepted that the quality of a fracture reduction is inversely related to the maintenance of blood supply to the fracture fragments. It is not hard to enact an anatomic reduction if all the deforming forces (and therefore all the viability) are removed. Similarly, it is not hard to maintain soft tissue attachments if reduction is not a primary concern. To resolve this conflict, it is necessary to understand the reduction requirements of the area involved. It is generally accepted that the articular fracture component mandates an anatomic reduction in an effort to limit the risk of posttraumatic arthritis. This reduction is typically accomplished via an open (possibly extensile) approach and direct reduction techniques with visualization of the fracture reduction. In contrast, the fracture component that creates separation between the epiphysis and diaphysis has different reduction requirements. All that is typically required is a functional reduction (restoration of length, alignment, and rotation). Because of the less-stringent reduction requirement, this reduction can often be accomplished while preserving nearly all viability via a limited approach with indirect reduction techniques and radiographic confirmation of the reduction.
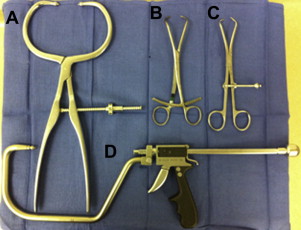
In the obese population, the articular reduction for tibial periarticular fractures can be challenging. Limb geometry differs greatly between the 2 populations. Open approaches to the articular surface typically have to be larger because the visual field decreases as the depth of approach increases. Adjunctive aids become even more important. The universal distractor (Synthes, WestChester, PA, USA) improves joint visualization and limits unwanted deforming forces (which are often accentuated by the increased size of the limb). A headlight is especially useful as the depth of approach increases. Once adequate visualization is present, unique reduction difficulties are encountered. Standard clamps were designed for average-sized individuals. These clamps often fit poorly in the morbidly obese population. Although the bone diameter varies little compared with the nonobese population, the soft tissue circumference varies greatly. This increase in soft tissue circumference can lead to soft tissue crushing with standard clamp designs. The excursion of a clamp and the maximum distance between the 2 arms are linked by the clamp design. Design parameters such as the clamp arm shape, the ability of the clamp to disarticulate, and the locking mechanism affect its use ( Fig. 3 ). Periarticular clamps, pelvic clamps, and collinear clamps should be available when attempting tibial reductions in the obese population. When both tines of the clamp are placed through the surgical approach, periarticular designs are less beneficial and even create a disadvantage when compared with the standard clamp designs; however, when one or both tines of the clamp need to be placed through a percutaneous incision, soft tissue crushing can be prevented with these alternative clamp designs.