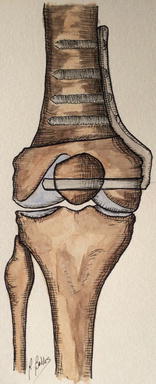
Fig. 6.1
HTO – medial opening wedge
Currently HTO is undergoing a revival, particularly in younger more active patients, due to the desire to preserve the native knee, bone stock, and proprioception and also the possibility to allow physical activities that are not well tolerated with a unicompartmental knee arthroplasty (UKA) [6]. The preference also relates to expectations for physical activities due to the increase in life expectancy [7]. In addition, HTO has become a better option due to new hardware: plates that work like an “internal fixation” allowing a very stable osteosynthesis and periosteal vascular supply preservation. There are also new and more sophisticated bone substitutes and biomaterials that can avoid an iliac crest bone graft harvest and therefore an additional incision with related complications [3, 8, 9].
The first aim of HTO is to eliminate or reduce pain, translating loads to the contralateral femorotibial compartment by correcting deformity. Surgical indications and careful preoperative planning are important to permit long-term satisfying results [10–17]. This chapter will summarize the current knowledge about periarticular knee osteotomies.
6.1.2 Indications and Contraindications (Table 6.1)
Table 6.1
Indications and contraindications in HTO
Indications | Contraindications |
|---|---|
Age between 40 and 70 | BMI >30 (disputable) |
Flexion >90°, lack of extension <20° | Flexion <90°, lack of extension >20° |
Medial femorotibial compartment involvement | Osteoarthritis (3–4° Outerbridge) in contralateral compartment |
Non-reducible deformity | Medial meniscectomy |
Metaphyseal varus | Infection |
Active lifestyle | Rheumatoid arthritis |
Good compliance for rehabilitation | Tibial subluxation >1 cm |
High smokers |
Physical indications include: age between 30 and 70 years; well localized pain at the femorotibial joint line; flexion more than 90° and, if present, a lack of extension <10°; normal or correctable ligamentous status (but anterior cruciate ligament [ACL] or posterior cruciate ligament [PCL] insufficiency is not a contraindication); non-reducible deformity; and patients with an active lifestyle [18].
Physical contraindications include obesity, inflammatory disease, smoking, osteoarthritis or meniscectomy in the contralateral compartment, and tibial subluxation more than 1 cm.
Radiological indications include partial or complete joint space width narrowing in one compartment, no contralateral femorotibial joint space width narrowing or patellofemoral joint space width narrowing, and extra-articular deformity more than 5° [18]. MRI can also be used to more accurately assess the contralateral compartment.
6.1.3 Surgical Techniques
Two techniques have been used for the treatment of medial compartment arthritis: medial opening wedge high tibial osteotomy (OWHTO) (Fig. 6.1) and lateral closing wedge high tibial osteotomy (CWHTO) (Fig. 6.2).
6.1.3.1 Surgical Planning (Table 6.2)
Table 6.2
X-ray needed for a correct planning
Preoperative planning |
Standard x-ray posteroanterior and lateral |
X-ray in Rosenberg view |
Weight-bearing anteroposterior long-leg x-ray |
Sky view patellar x-ray |
Preoperatively, a complete radiological evaluation of the limb is mandatory for accurate planning. This is to determine the mechanical axis and calculate the amount of correction required. The standard x-ray series shows the osteoarthritis grade and the tibial slope, including x-rays done in Rosenberg view (45° of flexion). The weight-bearing anteroposterior long-leg x-ray allows measurement of the HKA angle to plan the correction. The axial patellar x-ray assesses involvement of the femoropatellar joint. A guide to the measurement of the constitutional varus is the epiphyseal axis as defined by Levigne (a line connecting the middle of the tibial joint line and the middle of the line connecting the tibial epiphysis). This axis forms a constant angle of 90° ± 2° to the lateral tibial plateau. The constitutional deformity of the tibia is defined as the angle between the epiphyseal and the tibial mechanical axis. The alignment goal of correction for osteoarthritis is usually 2–3° of mechanical valgus [18].
6.1.3.2 Opening Wedge High Tibial Osteotomy (Table 6.3)
Table 6.3
HTO techniques
Approach and technical considerations |
Lateral closing wedge high tibial osteotomy (using a blade plate) |
Slightly oblique anterolateral skin incision, the insertion of the tibialis anterior is released as a Z-plasty; tibialis anterior and long toe extensor muscle are released from the metaphysis |
Osteotomy of the fibular neck, protect the peroneal nerve |
HTO is done proximal to the tibial tubercle in an oblique direction, using image intensifier |
Introduce the blade plate, perform the distal cut of the osteotomy with the saw; the medial cortex is weakened with a 3.2 mm drill |
Evaluate the femorotibial axis and fix the osteotomy with two bicortical screws |
Medial opening wedge high tibial osteotomy |
Anteromedial skin incision just proximal to the tibial tubercle, retraction of pes anserinus tendons, incision of the superficial MCL |
Perform the osteotomy proximal to the tibial tubercle, first insert two Kirschner guide pins, from medial to lateral, just above the fibular head, use image intensifier; if the position is okay, perform the osteotomy with the saw; first cut the center then the anterior and finally the posterior part of the tibia. Complete the cuts with osteotome |
Subsequently introduce a Lambotte osteotome to open the osteotomy and then introduce as much osteotomes as necessary to obtain the desired correction |
Fix the osteotomy with a plate and screws or staples |
The osteotomy is performed just proximal to the tibial tubercle, having elevated the superficial medial collateral ligament. The plane of the osteotomy is horizontal, slightly different from the medial closing wedge HTO, which is more oblique. First two Kirschner wires are introduced medially. Laterally, these guide pins should be just superior to the head of the fibula. Correct position of the guide pins is assessed using the image intensifier. The direction can be adjusted, if necessary. Using an oscillating saw, the tibial cut is made underneath these guide pins, always staying in contact with them. Firstly, the center of the tibia is cut, followed by the anterior and posterior cortices. The cuts are completed using an osteotome, especially on the anterior cortex, where the patellar tendon is at risk. It is necessary to have an intact lateral hinge for this type of osteotomy. Subsequently, a Lambotte osteotome is introduced into the osteotomy. A second osteotome is then introduced below the first. To open up the osteotomy gently, several more osteotomes are introduced between the first two. In order to maintain the tibial slope, the opening of the osteotomy at the posteromedial cortex should be approximately twice that at the tibial tubercle [19].
Fig. 6.2
HTO – lateral closing wedge
Due to autograft site harvest morbidity, bone substitutes have been used with more frequency, mostly of calcium and phosphate. These substitutes try to reproduce the bone structure, with their porosity, provide a structural support, and allow new vessel and osteoprogenitor cell infiltration promoting new bone formation.
Best results are seen with biomaterials like tricalcium phosphate, calcium phosphate, hydroxyapatite-tricalcium phosphate, and hydroxyapatite only. Substitutes like bioglass, coralline wedges, and combined fillers give high rate of delayed union and nonunion [8].
First treatment with HTO was performed without fixation, but this leads to a high rate of complications including loss of correction, joint stiffness, and patellar tendon contracture. The best fixation is still controversial. Options for fixation include staples, external fixators (axial and circular), and plates (conventional, blade plates, locking plates and with or without spacers). Specific plates such as Puddu plate and Tomofix have demonstrated a high rate of union and less complications [8].
6.1.3.3 Closing Wedge High Tibial Osteotomy (Table 6.3)
The fibular styloid process is first identified, and this procedure usually starts with the osteotomy of fibular head (or neck) or the release of the proximal tibiofibular joint in order to prevent any impingement with the fibula and to allow a final good correction. The surgeon can measure 60 mm distally from the fibular styloid process, in order to define the zone where the fibular osteotomy should be performed. The area between 68 and 153 mm should be avoided, to prevent peroneal nerve palsy [7].
Once the fibular osteotomy is performed, the distal cut of the closing wedge osteotomy is performed. Many surgeons use a guide pin for the distal cut of the osteotomy. The posterior surface of the tibia is protected by a large periosteal elevator, and the patellar tendon is retracted anteriorly. An oscillating saw is used to make the distal cut. An angled cutting guide (6.8 or 10°) is introduced in the distal cut of the osteotomy, and the proximal cut is then made using this angle. The cutting guide should be introduced and impacted on the medial cortex. An oscillating saw is used. The bone wedge is removed. The medial cortex is weakened with a 3.2 mm drill. The wedge is closed, and using a long metal bar positioned on the center of the femur head and in the middle of the ankle joint, the mechanical femorotibial axis is evaluated. The metal bar should pass just laterally to the lateral tibial spine. Computer-assisted surgery can also be used if available.
The osteotomy can be fixed with staples, blade plate, or locking plates.
6.1.4 Results (Tables 6.4 and 6.5)
Table 6.4
Systematic review HTO (closing wedge)
Author | Journal/year | Average age | Osteoarthritis classification | Cohort (operated knees) | Device used | Follow-up (years) | Preop average angle | Postop average angle | Results | Scores | Complication rates | Complications | Survival |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Gstöttner et al. [6] | Arch Orthop Trauma (2008) | 54 years (19–74) | – | 134 | Staple | 12.4 years (1–25) | FTA varus 6–10° 57 %, 11–15° 21 %, 1–5° 18 % | FTA valgus (1 year fu) 1–5° 60 %, 0–5° 20 %, 5–10° 20 % | Survivorship: 94 % 5 years fu, 80 % 10 years fu, 65.5 % 15 years fu, 54 % 18 years fu; predictor factors: age. Not predictor factors: gender, mechanical axis | – | 28 % | 7 % DVT, 5 % peroneal nerve palsy, 2 % sup infection, 14 % delayed union | 39 % converted to TKA |
Papachristou et al. [7] | International Orthopaedics (2006) | 51 years (26–60) | Ahlbäch 32 % grade I, 23% grade II, 45 % grade III | 44 | Staple | 10 years (5–17) | FTA 177.7° | FTA 185.8° | Postop: 88 % pain relief. 10 years fu: 27.2 % excellent, 9.09 % good, 11.3 % fair-poor. 10–15 year fu: 4.5 % excellent, 15.9 % good, 15.8 % fair-poor | HSSK preop: 52 points. HSSK postop: 83.5 points excellent-good, 58.83 points fair-poor | 11 % | 4.5 % Sup. infection, 4.5 % tibial fracture, 1 % pulmonary embolism | – |
Koshino et al. [8] | The Knee (2006) | 59.6 years (40–73) | Ahlbäch 60 % grade II, 35 % grade III, 6 % grade IV | 241 | Plate + screws | 68 knees included 19 years (15–28) | FTA 186° ± 6.5° | FTA 171° ± 7.5° | 15–28 years fu: 98 % satisfied | HSSK preop: 21 % 60–69 points fair,78 % 59 points poor. HSSK postop: 65 % 85–100 points excellent, 25 % 70–84 points good, 10 % 60–69 points fair | 6 % | 4.4 % peroneal nerve palsy, 1.4 % tibial fracture | 16 % converted to TKA/MUA at final fu |
Aoki et al. [32] | JBJS (2006) | 59.8 years (47–72) | HUGS 25 % grade II, 55 % grade III, 20 % grade IV | 86 | External fixator | 56 knees included 11 years (10–15) | FTA 185.4° (180–198°) | FTA 170.6° (163–183°) | 18 % good, 45 % fair, 37 % poor | TKSS preop: 53.2 (35–65), poor. Postop: 74.4 (50–95), fair | 28 % | 23 % delayed union, 3 % peroneal nerve palsy, 2 % superficial infection | 3 % converted to TKA |
Sprenger et al. [5] | JBJS (2003) | 69 years (47–81) | Ahlbäch 57 % grade I, 54 % grade II, 3 % grade III | 76 | Plate + screws | 10.8 years | – | – | Survivorship: 86 % 5 years fu, 74 % 10 years fu, 56 % 15 years fu. Mean patient satisfaction 9.5 years. No differences in: age, gender, weight, Ahlbäck (except grade II vs. III) | HSSK <70 points survivorship: mean 7.4 years | 21 % | 43 % nerve palsy, others not reported | 34 % converted TKA |
Aglietti et al. [17] | JKS (2003) | 58 years (36–69) | – | 120 | 32 % plaster cylinder cast 68 % screw + cylinder cast | 61 knees included in 15 years (10–21) | Average varus angle 4.7° ± 5° | – | Preop pain: 66 % moderate, 33 % severe. Postop pain: 16 % mild, 21 % moderate, no severe pain reported | HSSK final fu: 46 % excellent, 25 % good, 21 % fair, 8 % poor | 9 % | 4 % DVT, 1 % fatal PE, 5 % delayed union | 25 % converted TKA average time conversion 11 years (7–17) |
Benzakour et al. [23] | International Orthopaedics (2010) | 55 years (40–72) | Ahlbäch 20 % grade I, 35 % grade II, 37 % grade III, 8 % grade IV | 106 | Plate/staples/molded cast | 15 years (5–27) | Average varus angle 11° | – | 12 % excellent, 30 % good, 31 % fair, 27 % poor | HSSK improvement: 86 % score improvement at final fu | 11 % | 2 % implant removal, 2 % sup infection, 1 % hematoma, 1 % art. fracture, 2 % cortical fracture, 1 % DVT, 1 % nerve palsy, 2 % dystrophy | 10 % converted TKA, 2 % re-osteotomy |
Douglas et al. [16] | Clin Orthop Relat Res (1999) | 55 years (16–76) | – | 94 | Staples/external fixator | 61 knees included in 14 years (10–22) | – | – | Survivorship estimate of failure: 73 % at 5 years, 51 % at 10 years, 39 % at 15 years, 30 % at 20 years. Risk factors associated: >50 years, prev arthroscopy, <120° flexion arch, high BMI, lat thrust | – | 20 % | 15 % delayed union, 10 % nonunion, 3 % art. fracture, 16 % sup infection, 2 % deep infection, 2 % instability, 25 % DVT, 3 % perennial nerve palsy | 20 % converted TKA at latest fu |
Yasuda et al. [19] | Clin Orthop Relat Res (1992) | 60 years (47–72) | Sasaki 18 % stage II, 58 % stage III, 24 % stage IV | 86 | External fixator | 51 knees included in 11 years (10–15) | FTA 185.5° (175–185°) | FTA 6 years fu: 169° ± 5.4°. 10 years fu: 170° ± 6.3° | Preop: 7 % fair, 93 % poor. 6 years fu: 63 % good, 25 % fair, 12 % poor. 10 years fu: 18 % good, 45 % fair, 37 % poor | TKSS improvement: 54 % 6 years fu, 49 % 10 years fu. WAS improvement: 2 % 6 years fu, 2 % 10 years fu. PS improvement: 4 % 6 years fu, 3 % 10 years fu | 5 % | 2 % peroneal nerve palsy, 1 % sup infection, 1 % delayed union | 2 % converted TKR <5 years of fu |
Fletcher et al. [22] | Clin Orthop Relat Res (2006) | 42 years (15–76) | Ahlbäch 64 % grade I, 28 % grade II, 8 % grade III | 372 | Staple/plate + screws | 301 knees included in 18 years (12–28) | Average varus angle 6° (13–15°) | 66 % postop varus deformity 5° (1–12°)/34 % postop valgus deformity 3° (1–10°) | 33 % excellent, 44 % good, 7 % fair, 15 % poor protecting factors outcome: <50 year, BMI <25, Ahlbäch grade I, postop valgus angle >6°. No correlation: gender, preop varus angle | – | 3 % | 1 % DVT, 1 % sympathetic dystrophies, 1 % fixation failure, 0.3 % other complications | 7 % converted TKA/4 % converted MUA revision end point 8 years |
Majima et al. [18] | Clin Orthop Relat Res (2000) | 59 years (47–70) | – | 48 | External fixator | 26 knees included in 12 years (10–15) | FTA 185.1 ± 6.3° | FTA 171° ± 6.1° | – | TKSS preop: 7 % fair, 93 % poor. Postop: 1 year 49 % good, 51 % fair, 1 % poor. 10 years 17 % good, 44 % fair, 39 % poor | 4 % | 4 % skin necrosis. No serious complications observed | 4 % converted TKA <7 years fu |
Yasuda et al. [20] | Bulletin HJDOT (1991) | 59 years (37–76) | HUGS 14 % grade II, 58 % grade III, 27 % grade IV | 86 | External fixator | 55 knees included in 12 years (10–15) | FTA 186° (175–195°) | FTA 170.6° (10 years fu) | Preop: 11 % fair, 89 % poor. 6 year fu: 62 % good, 23 % fair, 15 % poor. 10 year fu: 25 % good, 36 % fair, 38 % poor | TKSS preop: 60.2 points, poor. Postop: (6/10 years fu) 89.7 points, fair; 81.4 points, fair. WAS preop: 11.2. Postop: (6/10 years fu) 17.3, 14.1. PS preop: 13.5. Postop: (6/10 years fu) 27.4, 23.3 | 7 % | 4 % peroneal nerve palsy, 1.5 % delayed union, 1.5 % sup infection | 4 % converted TKA <5 years fu |
Ivarson et al. [21] | JBJS (1999) | 73 years (52–87) | – | 99 | Staple | 65 knees included in 11.9 years (11–13) | – | – | Satisfaction: 5.7 years fu; 57 % good/78 % acceptable/11, 9 years fu; 43 % good 60 % acceptable pain at rest: prep 65 %/5.7 years fu: 38 %/ 11.9 years fu: 30 % | LST: 11.9 years fu; 64 ± 21; fair | 12 % | 9 % sup infection, 2 % DVT, 1 % peroneal nerve palsy | 6 % converted TKA and 1 % converted MUA <5.7 years fu |
Van Raaij et al. [33] | Acta Orthopaedica (2008) | 49 years (24–67) | Ahlbäch 5 % grade 0, 43 % grade I, 44 % grade II, 8 % grade III | 100 | Staple | 12 years (10–16) | FTA 6.5° | – | Regression model, high risk to conversion to TKA: woman, Ahlbäch >2. No risk associated with BMI and preop HKA angle | – | 4 % | 1 % overcorrection (varus HTO), 1 % symptomatic exostosis, 3 % peroneal nerve palsy | 25 % converted TKA < average of 6 years. Probability of surviving HTO 75 % at 10 years fu |
Schallberger et al. [27] | Knee Surg Sports Traumatol Arthrosc (2011) | 40 years (15–68) | – | 71 | OWHTO: plate + screws. Iliac crest CWHTO: plate + screws | 54 knees included in 13.5 years (13–21) | FTA 178° (171–184°) | FTA 190° (184–190°) median correction 10° | Osteotomy survival was of 98 % after 5 years, 92 % after 10 years, and 71 % after 15 years | Average VAS at final fu: 0, range 0–4 (0–10). MSI: 80 %, range 30–100 (0–100) at final fu. Medial KOOS score: 71, range 9–100. Median WOMAC score: 84, range 9–100, both at final fu | – | – | 24 % converted TKA, 76 % survivor HTO at final fu OWHTO vs. CWHTO no significant difference in survival and score outcome |
Babis et al. [29] | J Orthop Sci (2008) | 53 years (19–71) | – | 54 | Plate + screws | 36 knees included in 10 years (7–14) | FTA 186.6° ± 3° | FTA 177.2 ± 3.61° (2 months fu) | Satisfaction 35 % excellent, 16 % good, 11 % fair, 19 % poor result or had failed. No risk factors: age, BMI, preop medial load, preop/postop medial line obliquity | HSSK preop: 49 points, poor. At final fu: 77 points, good | – | – | 31 % converted to TKA <7.6 years fu osteotomy survival rate 89 % at 5 years/76 % at 10 years |
Omori et al. [30] | J Orthop Sci (2008) | 59 years (40–69) | KLC 16 % grade II, 73 % grade III, 10 % grade IV | 68 | Plate + screws | 48 knees included in 17.1 years (14–24) | FTA 185.4 ± 4.4 | FTA 169.1 ± 4.5 (6.5 years fu)/169.8 ± 5.2 (17.1 years fu) | 77 % satisfied, 33 % unsatisfied | JOA score 48 knees. Preop: 59.1 points, poor. 6.5 years fu: 86.3 points, good. >10 years fu: 83.1 points, good | 4 % | 2 % peroneal nerve palsy, 2 % delayed union | – |
Akizuki et al. [28] | JBJS (2008) | 63 years (45–76) | KLC 6 % grade II, 33 % grade III, 61 % grade IV | 132 | Plate + screws | 94 knees included in 16.4 years (16–20) | FTA 183.7° (177–195) | – | 74 % excellent/good at final fu | HSSK preop: 60.7 points, fair. 5 years fu: 90 points, excellent. Final fu: 84 points. Good risk factors: BMI, prep range of movement | 13 % | 4.2 % peroneal nerve palsy, 0.8 % DVT, 2.5 % skin necrosis, 0.8 % sup infection, 1.6 % nonunion, 1.6 % early loss correction | 7.4 % converted to TKA. Survivorship 97.6 % at 10 years fu/90.4 % at 15 years fu |
Hoells et al. [31] | JBJS (2014) | 50 years (26–66) | 1 % mild, 10 % moderate, 89 % severe | 164 | Plate + screws | 95 knees included in 10 years | – | – | Improved survival rates: age <50 year, BMI <30, WOMAC >45 | WOMAC: preop, 61/ 5 years fu; 88 /10 years fu: 84 TKSS: prep 130/5 years fu; 181/10 years fu; 168 | 7 % | 1 % PE, 2 % sup infection. 3 % delayed union, 1 % nonunion | Survivorship 87 % at 5 years of fu/79 % at 10 years fu |
Table 6.5
High tibial osteotomy (opening wedge)
Author | Journal/year | Average age | Side | Osteoarthritis classification | Cohort (operated knees) | Device used | Graft | Follow-up (years) | Preop average angle | Postop average angle | Results | Scores | Complication rates | Complications | Survival |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Hernigou et al. [13] | The knee (2001) | 59 years (35–73) | Medial opening wedge | – | 245 | Plate + screws | Cement block | 87 knees included in 10 years (6–15) | – | 75 % desired correction (3–6° valgus), 5 % overcorrected, 20 % undercorrected | Survivorship (Kaplan- Meier): 94 % (5 years), 85 % (10 years), 68 % (15 years) | – | 4 % | 1.6 % postoperative infection, 0.4 % vascular injury, 0.4 % DVT, 0.4 % non-union, 0.8 % delayed union | 87 patients (10 years fu): 26.4 % converted TKR, 73.5 % satisfied |
Hernigou et al. [11] | International Orthopaedics (2010) | 60 years (43–67) | Medial opening wedge | – | 53 | Plate + screws | Resorbable tricalcium phosphate | 10 years (8–12) | FTA 162° (158–165°) | FTA 180° (173–190°) 10–12 years | 10 years fu: 81 % excellent-good/1.3 % fair/ 11.3 % poor | – | 4 % | 3.7 % fixation system complain (before 4 years after OWTO) | 9.4 % converted TKA, 1.8 % converted MUA (before 7 years after OWTO) |
Marti et al. [14] | JBJS (2001) | 43 years (17–66) | Lateral opening wedge | Ahlbäck 41 % grade I, 53 % grade II, 5.8 % grade III | 36 | Plate 53 % Screw 8.8 % Ext. fix. 3 % Staple 5.8 % None 30 % | Iliac crest | 11 years (5–21) | FTA 11.6° (4–22) | FTA 5.1° (−5–13) | 0 % progression OA, 0 % loss ROM after follow up | LGS 26 % excellent 62 % good 9 % fair 3 % poor | 15 % | 9 % nerve palsy, 3 % superficial infection, 3 % thrombophlebitis | 3 % converted to arthrodesis because severe pain (before 6 years after OWTO) |
Benzakour et al. [23] | International Orthopaedics (2010) | 55 years (40–72) | Medial opening wedge | Ahlbäch 20 % grade I, 35 % grade II, 37 % grade III, 8 % grade IV | 118 | Plate/staples/molded cast | Iliac crest | 15 years (5–27) | FTA 133° | – | 12 % excellent/30 % good/31 % fair/27 % poor | KSS improvement: 67 % score improvement at final fu | 11 % | 2 % re-osteotomy, 2 % implant removal, 2 % sup. infection, 1 % hematoma, 1 % art. fracture, 2 % cortical fracture, 1 % DVT, 1 % nerve palsy, 2 % dystrophy | 10 % converted TKA |
Hernigou et al. [10] | JBJS (1987) | 60 years (43–77) | Medial opening wedge | Ahlbäch 37 % grade I, 48 % grade II, 11 % grade III, 2 % grade IV, 1 % grade V | 89 | Plate + screws | Iliac crest | 76 knees included in 11.5 years (10–30) | FTA 172° (158–179) | FTA 182° (173–190°) | Final follow up preop pain: 55 % severe/49 % moderate/5 % mild postop pain: 13 % severe/16 % moderate/16 % mild/55 % none | – | – | – | 18 % knees required revision at 5–10 years: 5 % MUA, 4 % bicompartmental, 10 % re-osteotomy |
Saragaglia et al. [15] | International Orthopaedics (2011) | 53 years (32–74) | Medial opening wedge | Ahlbäch 22 % grade I, 34 % grade II, 35 % grade III, 9 % grade IV | 124 | Plate + screws | Tricalcium phosphate | 107 knees included in 10 years (8–14) | FTA 172° (162–179°) | FTA 182° (178–186°) | HTO survivorship: 89 % in 5 years/74 % in 10 years 88 % satisfaction at final fu | LS: preop 65.4 ± 13.3 points/postop 88 ± 12.7 points (51–100) KOOS score 86 ± 4.6 points (25–100) | 22 % | 8 % tibial plateau fracture, 2 % DVT, 3 % PE, 6 % delayed union, 3 % screw breakages | 12 % converted TKA at 8 ± 3 years |
6.1.4.1 Outcomes
There are 25 published series of high tibial osteotomy with an average of more than 10 years of follow-up currently in the literature [3, 6, 7, 9–12, 16, 20–35]. The studies were divided into two groups: opening wedge high tibial osteotomy (OWHTO) and closing wedge high tibial osteotomy (CWHTO).
CWHTO
The CWHTO results included 2091 operated knees. The mean follow-up range is from 10 to 18 years. There are different kinds of devices that have been used to fix the osteotomy: plate and screws 42 %, staples 31 %, external fixture 26 %, and cylinder plaster 1 %. In literature, the average femorotibial angle pre- and post-operation is 177°–186° and 169°–190°, respectively.
Good results have been reported regarding survival rates, >survivorship at 5 years of follow-up from 73 to 98 %, at 10 years of follow-up from 51 to 92 %, and more than 15 years of follow-up from 39 to 71 % [7, 20, 25]. Koshino et al. reported a satisfaction rate at final follow-up for excellent/good results of 98 % at 15–28 years of follow-up [22]. Sprenger et al. reported excellent/good patient satisfaction of 9.5 years after HTO [7].
Risk factors that have been associated with poor outcomes are age more than 50 years at time of surgery, less than 120° of flexion, high BMI, lateral thrust, more than Ahlbäck grade I articular degeneration in contralateral compartment, and excess postoperative valgus angle [10, 22, 25, 30, 31, 35].
Survival rates are influenced by preoperative mechanical axis, gender, and WOMAC >45 [7, 10, 20, 31, 33, 35]. Van Raaij et al. associated low grades of survival rates in women [35]. Conversion rates included for conversion to total knee arthroplasty or unicompartmental arthroplasty are from 3 to 39 % [2, 6, 7, 10, 20, 25, 27–29, 31, 35].
OWHTO
The OWHTO results included 665 operated knees. Literature shows the prevalence of the medial opening osteotomy technique except Marti et al. who perform a lateral opening osteotomy [26]. Mean follow-up range is from 10 to 15 years.
The fixation devices used were plate and screws, staples, screws, external fixator, and modulated cast. Tricortical iliac crest was used in 50 % of the articles, tricalcium phosphate was used in 33 % of the studies, and 16 % used cement block. Average femorotibial angle pre- and post-operation is 133°–172° and 180°–182°, respectively.
Good results have been reported regarding survival rates, survivorship at 5 years of follow-up from 89 to 94 %, at 10 years of follow-up from 74 to 85 %, and more than 15 years of follow-up around 68 %, reported by Hernigou et al. [9, 24]. Hernigou et al. mentioned a satisfaction rate at 10 years follow-up for excellent/good results of 81 % and Saragaglia et al. 88 % excellent/good results at final follow-up [9, 22].
6.1.4.2 Complications (Tables 6.4, 6.5, 6.6 and 6.7)
Table 6.6
Advantages and disadvantages of the two different techniques
Surgical techniques: advantages and disadvantages |
Closing wedge high tibial osteotomy |
Lateral |
Peroneal nerve palsy |
Potentially less accurate |
Potential changes in patellar height (patella alta) |
Opening wedge high tibial osteotomy |
Medial |
Fracture of the lateral hinge or the tibial plateau |
Creates less deformity than CW in tibial metadiaphysis |
Potential increase in tibial posterior tibial slope |
Potential changes in patellar height (patella infera) |
Table 6.7
Complications in HTO
Complications |
|---|
Malunion |
Nonunion |
Patella infera or patella alta |
Stiffness |
Loss of correction |
Hardware failure |
Compartmental syndrome |
Neurologic injury (peroneal nerve palsy) |
Vascular injury |
Infection |
Proximal tibial fracture |
For CWHTO complication rates, the average is from 3.3 to 28 %. The most frequent complication reported in this group is peroneal nerve palsy with rates from 2 to 43 % [7, 20, 22, 26, 34], followed by delayed union with an average of 2–23 % [6, 20, 25, 32, 34]. Other important complications are deep vein thrombosis, pulmonary embolism, superficial infection, skin necrosis, and sympathetic dystrophies. OWHTO complication rates are 3 to 22 %, mainly due to tibial plateau fracture in 10 %, nerve palsy in 10 %, and delayed union in 10 %. Other important complications are superficial infection and vascular problems [3, 9, 11, 16, 23, 25].
6.1.5 Discussion
Knee joint realignment is intended to redistribute knee joint forces from the affected area to the unaffected side to interrupt the vicious cycle of destruction and malalignment described by Coventry who postulated arbitrarily that varus knees should be overcorrected by osteotomy to 5° of valgus [31]. The majority of authors have reported satisfactory results in the short to midterm, but these results gradually deteriorated over time, especially at more than 10 years after surgery. The most important finding of this review is the high survival rate of HTO which after 5 years of follow-up is over 95 %, after 10 years of follow-up is around 80 %, and more than 15 years of follow-up is more than 50 % for both techniques.
The percentage of satisfactory results (excellent/good) after HTO was over 80 % after long-term follow-up for both techniques. Looking at patients converted to TKA, most operations were performed more than 10 years after HTO. Generally, osteoarthritis progressed, and increasing symptoms became the indication for further surgery. Total knee arthroplasty should be reserved for unicompartmental or bicompartmental diseases in older and/or lower demand patients [29]. The success of osteotomies depends primarily on correct indication. Patients should have good pain tolerance because a low pain threshold is often a negative factor in the outcome of the treatment of musculoskeletal disease. Precise planning and appropriate surgical technique achieving the desired correction are fundamental [29]. Aglietti et al. reported that opening wedge technique creates less deformity than the closing with tibial metadiaphyseal mismatch that might interfere with a subsequent revision to TKA [6]. But hinge position can affect the change in posterior tibial slope. Medial OWHTO, in particular, is associated with an increased posterior slope (PTS) compared to CWHTO, due to an increased anterior positioning of the wedge. Anterior and superior translation of tibial plateau is followed by an earlier contact with femoral condyle. CWHTO is more commonly associated with a decrease in PTS. El-Azab et al. described PTS in OWHTO preop/postop with locking and no locking plate, 7.7°/9.1° and 5°/8.1°, respectively, and PTS in CWHTO preop/postop of 5.7°/2.4° [36]. Understanding of anatomy, and careful surgical technique can avoid unintentional changes in tibial slope.
Regarding the patellar height CWHTO is associated with an increased patellar height due to lowering the joint line, and in OWHTO descent of the patella is constant. Tigiani et al. observed a patella elevation in 57 % of CWHTO (Caton-Deschamps index), associated with a post-operation correction of knee axis less than 10°. OWHTO postoperation knee axis correction more than 15° is associated with a patella baja [37].
Regarding the filler used Lash et al. detailed that allograft is used in 25.9 %, autograft 29.5 %, tricalcium phosphate 12.6 %, calcium phosphate 7.2 %, hydroxyapatite-tricalcium phosphate 3.4 % (which is associated with higher rates of loss of correction), bioglass 1.7 %, combined fillers 0.9 %, coralline wedge 0.9 %, hydroxyapatite 0.4 %, and no filler 17.3 % [8].
For Benzakour et al. opening technique did not give significantly better clinical outcome than closing technique [11]. Opening and closing wedge HTO have similar results in functional outcome and survival. Literature comparing clinical outcome after opening versus closing wedge HTO is very limited and long-term comparisons are lacking, with only two authors reporting the comparison [11, 29]. Our results not only confirm the long-term effectiveness of valgisation high tibial osteotomy as treatment for medial compartment osteoarthritis, but there is also evidence that the opening wedge technique can have a long-lasting effect similar to the traditional closing wedge high tibial osteotomy. This has a high clinical relevance currently, as an increasing percentage of HTO are done using the opening wedge technique, and long-term experiences are very limited [29]. The main reason for the good clinical outcome is the good alignment which has been described as the most important factor for good long-term clinical results [22].
There is still considerable discussion about which factors affect the long-term outcome of HTO. Two of the most important factors are the correction angle at surgery and the preoperative severity of knee osteoarthritis. Regarding the correction angle, previous studies have reported that the optimum clinical outcomes were associated with a correction of 6–16° valgus, and an undercorrection less than 5° was strongly related to a high failure rate [6, 7, 22].
Douglas et al. showed that preoperative knee flexion of less than 120 was related to significantly lower survival, but Aglietti et al. did not relate failure to either flexion contracture or lack of extension. We found that the preoperative range of movement of <100 was significantly associated with early failure [6, 25].
6.1.6 Conclusions
In summary, opening and closing wedge high tibial osteotomies are successful and durable methods of treatment for unicompartmental degenerative diseases with associated varus in active patients. Survival of both techniques is comparable in most series and is associated with low complication rates, high satisfaction, and high activity levels of the survivors.
6.2 Distal Femoral Osteotomy
6.2.1 Introduction
Historically, the first treatment for genu valgum was osteotomy, but with the advent of TKA and UKA, they have been used less commonly. Today, osteotomy represents a valid option which allows postponing TKA and thereby preserving the native knee.
Degeneration of the tibiofemoral compartment leads to a valgus deformity that is frequently a consequence of partial or total lateral meniscectomy. Other causes are post-traumatic, partial epiphysiodesis and growth disorders. The purpose of osteotomies around the valgus knee is to relieve the lateral knee compartment and to displace the loads medially.
Proximal tibial varus osteotomy can be used for minor genu valgum deformities, but not for major angulations, or if the projected obliquity of the joint is more than 10°. Distal femoral osteotomy (DFO) is a good option because tibial osteotomies for large deformities produce medial tilt of the joint line, which may increase lateral shear forces and lateral subluxation during gait [5]. The most commonly performed techniques are the lateral opening or the medial closing, with dome osteotomy rarely used [38–40].
The aim of this section is to analyze the literature about DFO regarding indications, results, functional outcomes, and survivorship.
6.2.2 Indications and Contraindications (Table 6.8)
Table 6.8
List of indications and contraindications of DFO
Indications | Contraindications |
|---|---|
Age <60 male, age <55 female | BMI >30 (disputable) |
Flexion >90°, lack of extension <20° | Flexion <90°, lack of extension >20° |
Lateral femorotibial compartment involvement | Osteoarthritis (3–4° Outerbridge) in medial compartment |
Mechanical angle deformity localized in the femur | Medial meniscectomy |
Genu valgum | Infection |
Active lifestyle | Rheumatoid arthritis |
Good compliance for rehabilitation | Tibial subluxation >1 cm |
Valgus deformity >20° (disputable) | |
High smoking |
Appropriate indications for DFO are critical for final stability and good outcomes [40, 41]. Painful valgus deformity with related osteoarthritis in the lateral compartment is the absolute indication for DFO [42–46]. Better results have been seen in patients with mild osteoarthritis [47] and in valgus deformity not more than 20° due to the significant ligamentous laxity [48]. McDermott et al. stated that arthritis of the medial knee compartment is not an absolute contraindication, as long as it is minor compared to the lateral compartment. In addition, there must be good bone stock, normal circulation, a stable joint, and knee flexion >90° [15]. A small lack of extension may be tolerated and corrected during surgery [49].
Absolute contraindications include severe osteoarthritis of the medial compartment of the knee, severe tricompartmental osteoarthritis, and tibiofemoral subluxation [44, 46]. Osteoporosis is a relative contraindication because, despite a rigid femoral fixation, the cortical bone of the proximal segment can often subside into the cancellous bone of the distal segment when the patient weight-bears, resulting in unwanted axial deviation [45].
For Stahelin et al. contraindications are also valgus deformity due to obliquity of the tibial plateau, inflammatory arthritis, instability due to laxity of the medial collateral ligament, lack of extension >15°, and severe osteoporosis [45]. Puddu et al. included BMI >30 and severe bone loss (more than a few millimeters) of the lateral tibia or femur, since after intervention congruent weight-bearing on both tibial plateaus is not possible [48].
Femoropatellar involvement for Stahelin et al. is an absolute contraindication [45], but Zarrouck et al. and Wang et al. treated, respectively, nine patients and eight patients with DFO associated with patellofemoral osteoarthritis in which they performed a lateral release in 15 patients, distal realignment in one, and combined proximal and distal realignment in one patient. The final results at last follow-up were satisfactory [43, 46]. The proposed reason is because distal varus osteotomy decreases the Q angle between the quadriceps tendon and the patellar tendon, which reduces the magnitude of the patella’s lateral traction forces [5].
6.2.3 Surgical Technique (Table 6.9)
Table 6.9
DFO surgical techniques
Approach and technical considerations |
|---|
Medial closing wedge distal femoral osteotomy |
Approach medial side, proximal to the adductor tubercle and the anterior side of the femoral articular surface |
Osteotomy technique osteotomy trait parallel to the joint line. Do x-ray to ascertain that the chisel has not penetrated the intercondylar notch or the anterior femoral surface. Important to leave untouched the lateral cortex. Removal of a 5–10 mm bone wedge from the distal femur. Fixation with different hardware mostly a 90°degree offset dynamic compression blade plate or Tomofix |
Lateral opening wedge distal femoral osteotomy |
Approach lateral side, distal third of the femur 15 cm proximal to the joint line until the Gerdy’s tubercle, carried down from the vastus lateralis muscle |
Osteotomy technique If deformity is metaphyseal, osteotomy cut must be parallel and 30 mm proximal to the joint line; if diaphyseal it must be oblique to the joint line. Opening wedge filled up with auto-allograft, PRP, and bone cement and fixed with different hardware mostly the 95° blade plate, Puddu plate, or Tomofix |
Tibial medial closing wedge osteotomy was the first technique performed, but results have been reported not to be as good as those of proximal tibial valgus osteotomy for varus deformity. For corrections more than 12° of valgus, HTO is not recommended because the joint line, after bone removal, will be oblique medially inducing an increase in femorotibial shear stress. DFO will give much better results at long follow-up. Actually, the most commonly performed is the medial closing DFO as reported in multiple studies [42, 45, 46, 48–63].
All authors agree with regard to preoperative assessment: standard x-ray posteroanterior and lateral in which the tibial slope can be assessed, AP x-ray in Rosenberg view to quantify the compartmental involvement of osteoarthritis, weight-bearing anteroposterior long-leg x-ray to measure the angle deformity between the femur and tibia (mechanical or anatomic axis) and calculate the desired correction, and axial view of the patella to evaluate any osteoarthritis in the femoropatellar joint (Table 6.8). MRI scan is also a useful supplement to more accurately assess articular cartilage pathology.
6.2.3.1 Technique: Medial Closing Wedge DFO (Fig. 6.3)