A body mass index (BMI) greater than 30 is becoming increasingly common in the United States. Surgery for pelvic and acetabular fractures in this population is particularly problematic because conventional treatment often requires large surgical exposures. The surgery for both these fractures is technically difficult because of the volume of soft tissue and proneness to complications. Wound problems and infections are particularly common after open surgery in obese patients, and these increase linearly with the BMI. In this article, we present a small consecutive series over 14 months on obese patients who underwent percutaneous treatment of their pelvic or acetabular fractures.
Defined as a body mass index (BMI) greater than 30, calculated as the weight in kilograms to the height in meters squared, obesity in the United States is becoming increasingly common. Data from the National Health and Nutrition Examination Survey obtained in 2007 to 2008 showed that 33.8% of the adult population was obese. The steady increase in this population over 20 years has been described as an epidemic, although recent data suggest that the rate of increase appears to be slowing, both in adults and children. The implications of this expanding obese population for the trauma orthopedic community are enormous because this population is a discreet group that has a different physiology from the general adult population. Obese patients have higher rates of preexisting comorbidities; their metabolic response to trauma is different and they have higher rates of perioperative complications, such as wound sepsis and venous thromboembolism. In addition, there is evidence to suggest that the obese population is at a greater risk of pelvic injuries than the general population.
Through multiple studies, surgical treatment of fractures involving the pelvis and acetabulum has been shown to carry a much greater morbidity when performed in obese patients. For pelvic ring injuries, overall complication rates of surgery have been reported to be as high as 54%, with wound sepsis being by far the biggest component. In the acetabulum, rates of wound infection, thromboembolism, and operative blood loss are also increased 2-fold, and these rates follow a linear relationship with body mass, with overall complication rates reaching as high as 63% in morbidly obese patients (BMI>40).
With such a bloodcurdling complication profile from traditional surgery, a less-invasive surgical option for these challenging fractures in this high-risk population is potentially very attractive. If the infection rate alone could be reduced, without altering functional outcome, it would yield a huge benefit. For more than 10 years at our institution, we have been percutaneously treating all pelvic ring injuries and many of the acetabular fractures, particularly in high-risk patients, such as those who are obese.
In this article, we present a small consecutive series over 14 months on obese patients who underwent percutaneous treatment of their pelvic or acetabular fractures.
Patients and methods
A retrospective review was performed using our hospital surgical database, after institutional review board approval. Over a 14-month period, between January 2008 and March 2009, the authors performed pelvic or acetabular surgery on 117 consecutive patients. A chart review of each of these surgeries revealed a calculated BMI of 30 or more in 38 patients. Height and weight data were unavailable in one patient, but no other history of obesity was noted in their chart. Of the 38 obese patients, 24 had a pelvic ring injury, 17 had an acetabular fracture, and 3 had a combination of both. Overall, the authors treated 16 pelvic ring injuries and 7 acetabular fractures using percutaneous techniques, making a total of 23 fractures in 20 patients. The fracture types are summarized in Table 1 . Full medical records were available for review in all 20 patients.
| Pelvic Ring | Anterior Plating Only | Percutaneous ± Anterior Plating |
|---|---|---|
| APC-2 | 5 | 4 |
| APC-3 | — | 6 |
| LC-2 | — | 2 |
| LC-3 | — | 2 |
| Vertical Shear | — | 2 |
| Jumpers Fracture | — | — |
| Total | 5 | 16 |
| Open Fractures | — | 1 |
| Acetabulum and Pelvis | — | 3 |
| Acetabulum | Open | Percutaneous |
| Posterior Wall | — | — |
| Posterior Column | — | — |
| Anterior Wall | — | — |
| Anterior Column | — | — |
| Transverse | — | 1 |
| Transverse Posterior Wall | 4 | 2 |
| Posterior Column, Posterior Wall | 4 | — |
| T-Type | 1 | 1 |
| Anterior Column, Posterior Hemitransvserse | — | — |
| Associated Both Column | 1 | 3 |
| Total | 10 | 7 |
The mean age of the 20 patients was 35 and the average BMI was also 35, with only one patient exceeding the threshold of 40 for being morbidly obese (discussed later in Case Example: Patient 14). There were 14 men and 6 women. Pelvic ring injuries were classified using the system of Young and colleagues and acetabular fractures by that of Letournel and Judet.
Primary outcome measures were postoperative complications requiring repeat surgery, wound infection, deep vein thrombosis (DVT), pulmonary embolus (PE), and radiographic appearance both immediately postoperatively and at follow-up. Deep wound infections were defined as those requiring surgical debridement.
Radiographic Review
Patients with pelvic ring injuries underwent anteroposterior (AP), inlet, and outlet views on admission and at each follow-up, whereas those with acetabular fractures had AP and Judet views. Fracture displacement was measured using pixel calibration with a standard ruler from the Picture Archive Communication System (PACS-MagicWeb, Siemens Inc, New York, New York, USA). Measurements were performed by 2 independent observers (P. B. and J. G.) and a mean calculated. Where multiple views were available, measures showing maximal displacement were chosen.
For the pelvic ring, the method the authors used for measuring displacement was the same as that by LeFaivre and colleagues. A horizontal line is drawn across the superior end plate of the fifth lumbar vertebra. By using this line as a reference from which to make either horizontal measurements (in-line) or vertical ones (perpendicular), the maximum displacement of the anterior and posterior ring could be measured. Displacements were calculated by comparing normal bony landmarks to either the reference line or a perpendicular to it. When there were both pelvic ring and acetabular fractures, bony landmarks that were not involved with the hip injury and whose position was fixed to the constant fragment of the ilium were chosen. The reduction postoperatively and at latest follow-up was recorded and graded according to the method of Tornetta and Matta, with excellent grade being a residual displacement of 0 to 4 mm; good, 4 to 10 mm; fair, 10 to 20 mm; and poor, greater than 20 mm.
For the acetabular fractures, choosing a grading system was more difficult. The authors used the system of Anderson and colleagues, recently described for the assessment of femoral head medialization after a modified Stoppa approach. This approach involves taking a line from the spinous process of L5 down to the symphysis pubis and measuring the difference in the distance between this line and the center of the femoral head on each side. We have graded this as good (0–4 mm), fair (4–10 mm), and poor (greater than 10 mm). Our second outcome was radiological signs of arthritic change at final follow-up, graded 1 to 4 (1, normal appearance; 2, osteophytes; 3, narrowed joint space; 4, bone on bone).
Surgical Technique
General considerations
For both the pelvic ring and acetabulum, patients were positioned supine on a radiolucent bed with the abdomen and ipsilateral lower extremity prepped free. The weight limit of the operating room table was checked in supermorbidly obese patients, and nitrous oxide was avoided with anesthesia because excessive bowel gas can limit fluoroscopic visualization. Intra-abdominal contrast was flushed out where possible. Patients were paralyzed during surgery. Postoperatively, patients were restricted to 3 months of toe-touch–weight bearing on the side of the pelvic ring injury or acetabular fracture.
Pelvic ring
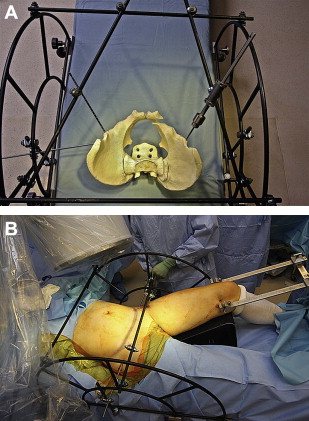
The technique we used for percutaneous pelvic ring fixation has been well documented in the past and involves the use of a pelvic reduction frame. ( Fig. 1 ) In short, this system enables one side of the pelvis to be stabilized to the operating table, while the other can be manipulated and fine-tuned with a high degree of radiological accuracy and control. One of the strengths of this system is that it allows near-anatomic reductions of the pelvic ring, without the need for either open approaches or multiple assistants. Our standard fixation was with transsacral iliosacral screws in both S1 and S2, although this varied according to patient anatomy. For the anterior pelvic ring, the technique of fixation depended on the fracture configuration and the soft tissue envelope. Although some symphyseal disruptions were treated with a standard plate and screws, when soft tissues were poor or the fracture was open, an external fixator was used. In one case, a cerclage wire was used. Pubic ramus fractures were generally treated with column screws in this study.
Acetabulum
Screw pathways for fixing acetabular fractures are well described in the literature and are not discussed here. Reduction maneuvers can be divided into closed and open techniques. In any periarticular fracture, there are usually some capsular attachments to the joint fragments, which remain intact after the injury. If patients can be bought to the operating room within a few hours of their accident, simple fracture patterns such as transverse configurations can be reduced by manipulation of the hip. The most commonly used, of course, is in-line traction, but forced internal or external rotation, flexion, and abduction are all maneuvers that have yielded anatomic reductions for us. Clearly, as time passes, these closed reduction maneuvers become increasingly unlikely to work and most displaced acetabular fractures require some form of open reduction with mini incision.
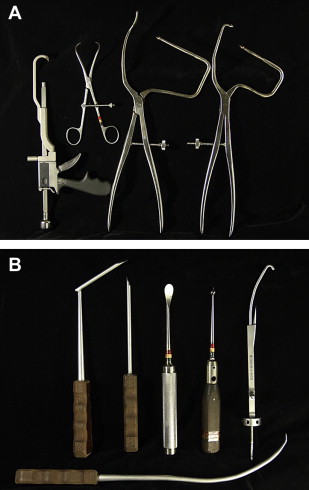
With the hip flexed up, we perform open reductions with mini incision through a small lateral window, approximately 1 to 2 cm behind the anterior superior iliac crest. A 3- to 5-cm incision is made, and after sharply dissecting off the oblique abdominal wall muscle attachment to the crest, a Cobb elevator can be passed down the inner table directly onto the fracture fragments. In high juxta- and transtectal injuries, the fracture lines can be directly palpated with a finger through the mini lateral window, which gives an additional reading for reduction over fluoroscopy alone. Specialized pelvic reduction clamps have been designed and developed by Charles Reinert, which have sufficient excursion to allow clamping of fractures around voluminous soft tissue envelopes ( Fig. 2 ). These clamps allow for transverse fractures to be rotated and compressed, for a displaced dome fragment to be squeezed back down, and for quadrilateral plate medialization to be keyed in. The combination of traction, specific manipulation, and percutaneous clamps allows us to achieve fluoroscopically excellent reductions in most of these cases. If we think that an excellent reduction cannot be achieved minimally invasively, we treat these injuries with open internal fixation via well-described approaches. We should also stress that this approach is not straightforward surgery, particularly in those who are obese, and is a technique that has evolved at our institution over the last 10 to 15 years. Each fracture pattern is unique and requires a slightly different screw configuration and reduction maneuver. We advise surgeons who are keen to try this technique to begin with simple, less-displaced fracture patterns before moving on to more complex ones.
Once an acceptable reduction is obtained, the fracture is stabilized with large fragment 6.5-mm or 7.3-mm cannulated screws. The choice of screw pathways is specific to the fracture configuration.
Statistical Analysis
All statistical tests were tabulated using SAS JMP v7 software (SAS Institute Inc, Cary, NC, USA). A Student t -test was used to compare means of continuous variables. Statistical significance was set at a P value of less than .05.
Results
Pelvic Ring
The 16 pelvic fractures had a mean follow-up of 9.7 months (3–24), and there were no deaths. One patient requested to be transferred out of state postoperatively and was subsequently lost to follow-up. The mean initial displacement of the fractures was 22 mm, and final reduction was good or excellent in 15 of the 16 patients, with 7 having a displacement of 4 mm or less. None of the fractures went down by a reduction grade between postoperative and follow-up radiographs. There was a highly significant difference between initial and postoperative displacement ( P = .0007) but not between the postoperative and final displacement ( P = .54). Pelvic ring results are summarized in Table 2 .
| Patient | Age (y) | Sex | BMI | Follow-Up Time (mo) | Fracture Type | Initial Displacement (mm) | Postoperative Displacement (mm) | Final Displacement (mm) | Final Grade |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 49 | M | 31 | 3 | APC-2 (open) | 18 | 7 | 9 | Good |
| 2 | 19 | M | 31 | 4 | APC-3 | 10 | 3 | 2 | Excellent |
| 3 | 47 | F | 31 | 15 | APC-2 | 7 | 3 | 4 | Excellent |
| 4 | 16 | M | 33 | 14 | APC-3 (bilateral) | 6 | 4 | 4 | Excellent |
| 5 | 33 | M | 33 | 3 | LC-3 | 4 | 2 | 2 | Excellent |
| 6 | 34 | M | 34 | 8 | APC-3 | 70 | 8 | 6 | Good |
| 7 | 62 | M | 35 | 9 | APC-3 | 22 | 2 | 2 | Excellent |
| 8 | 26 | F | 36 | 7 | LC-3 | 15 | 6 | 8 | Good |
| 9 | 46 | M | 32 | Lost to follow-up | Vertical shear | 47 | 8 | 8 | Good |
| 10 | 16 | F | 34 | 24 | LC-2 | 13 | 3 | 4 | Excellent |
| 11 | 30 | M | 34 | 19 | APC-3 | 38 | 5 | 5 | Good |
| 12 | 49 | M | 36 | 8 | APC-3 | 17 | 2 | 2 | Excellent |
| 13 | 67 | F | 37 | 9 | LC-2 (bilateral) | 15 | 11 | 16 | Fair |
| 14 | 21 | F | 45 | 7 | APC-2 (bilateral) | 40 | 7 | 8 | Good |
| 15 | 25 | M | 39 | 8 | APC-2 | 12 | 5 | 6 | Good |
| 16 | 16 | M | 36 | 8 | Vertical shear | 22 | 7 | 8 | Good |
| Mean | 35 | — | 35 | 9.7 | — | 22 | 5 | 5.3 | — |
Complications
There were no infections in this group, either superficial or deep, and there were no postoperative DVTs or PEs. Three patients, in whom adequate prophylaxis was impossible, received temporary central venous filters, but all 3 filters were subsequently removed. There were no new postoperative neurologic deficits. There were 2 scheduled returns to the operating theater, for supplementary anterior fixation. One of these (patient 6) patients was a 34-year-old man with a severe AP compression (APC) type 3 injury. Having stabilized his pelvic ring posteriorly, the anterior plating was postponed by 2 weeks because of an open laparotomy wound, which extended very distally. Once his soft tissues were more compliant, the symphysis was plated, with no further complications. The second case is reported later in the section Patient 14: Case Example.
The least favorable outcome was observed in a 67-year-old lady (the oldest in this series) with moderately displaced bilateral insufficiency fractures and unilateral ramus fractures after a fall down the steps. Her BMI was 37, and it was thought initially that she could be treated nonoperatively. However, as a result of ongoing pain and further displacement observed on serial radiographs, the patient required surgery at 17 days. Bilateral posterior percutaneous iliosacral screws were passed after closed reduction with the frame, and postoperative radiographs showed some improvement (from 15 to 11 mm of displacement). However, her follow-up radiographs showed that she had “settled” back to the preinjury position. With a displacement of 16 mm at follow-up, the patient’s result was graded as “fair.”
There were no cases of heterotopic ossification (Brooker grade 2 or worse) on the last follow-up radiographs, but 3 of the 16 patients with pelvic ring injuries did undergo removal of symptomatic hardware after bony union.
Acetabulum
The 7 acetabular fractures treated percutaneously had a mean follow-up of 9.1 months (4–18 months) with none lost to follow-up and no deaths. One patient had an undisplaced, transverse, posterior wall fracture, but all the others were initially displaced with a mean of 17 mm (9–22 mm). Patient data for the acetabular fractures are summarized in Table 3 .






