Percutaneous Pinning for Proximal Humerus Fractures
Leesa M. Galatz
DEFINITION
Proximal humerus fractures are defined as those of the proximal portion of the humerus involving the shoulder joint.
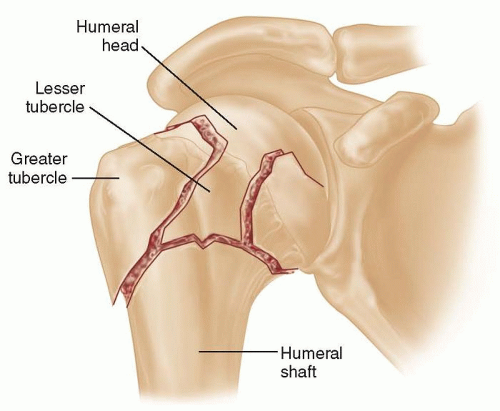
Fracture lines divide the proximal humerus into parts defined by anatomic structures that arise from early centers of ossification.
These “parts” first were described by Codman and led to development of the Neer classification,7 which is commonly used today.
The parts refer to the head of the humerus, the greater tuberosity, the lesser tuberosity, and the shaft (FIG 1).
Proximal humerus fractures are classified as two-, three-, or four-part fractures according to the Neer classfication.7
Displacement of a “part” is classically defined as 1 cm of displacement or 45 degrees of angulation. Importantly, displacement is not necessarily an indication for surgery but only a criterion for classification.
The type of fracture, degree of displacement, and the likelihood of osteonecrosis, as well as patient considerations, all factor into surgical decision making.
ANATOMY
The proximal humerus arises from four distinct centers of ossification: the humeral head, the greater tuberosity, the lesser tuberosity, and the shaft.
The greater tuberosity has three distinct facets for the insertion of the supraspinatus, the infraspinatus, and the teres minor muscles of the rotator cuff.
The lesser tuberosity is the insertion site for the subscapularis muscle.
The rotator interval lies between the upper subscapularis and the anterior border of the supraspinatus.
The long head of the biceps tendon lies in a shallow groove on the anterior proximal humerus and enters the glenohumeral joint at the rotator interval.
The proximal 3 cm of the long head of the biceps tendon lies deep to the interval tissue intra-articularly.
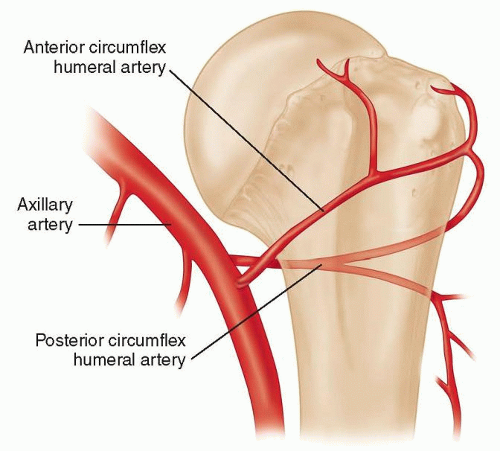
The anterior humeral circumflex artery (FIG 2) courses laterally along the inferior subscapularis.
The anterolateral branch of the anterior humeral circumflex artery travels superiorly along the lateral aspect of the biceps groove and enters the humeral head at the proximal-most aspect of the groove, providing about 85% of the blood supply to the humeral head.1
The posterior humeral circumflex artery gives off several small branches that run adjacent to the inferior capsule of the shoulder, providing most of the remaining blood supply.
The pectoralis major muscle inserts on the proximal shaft of the humerus lateral to the long head of the biceps tendon. The latissimus dorsi muscle inserts onto the proximal shaft medial to the biceps groove.
PATHOGENESIS
Proximal humerus fractures occur in a bimodal distribution.
Most proximal humerus fractures are “fractures of senescence” in older individuals with age-related osteopenia. They commonly result from low-energy injures such as tripping and falling.
They also occur in younger individuals as the result of highenergy injuries such as motorcycle or automobile accidents.
Associated nerve injuries can occur and usually resolve spontaneously. Axillary nerve neurapraxia is the most common.
NATURAL HISTORY
Eighty-five percent of proximal humerus fractures can be treated nonoperatively.7
Displacement at the surgical neck is better tolerated than displacement at the greater tuberosity.
Because of the vast range of motion (ROM) of the shoulder in multiple planes, the arm can compensate for translational displacement or angulation at the surgical neck.
Displacement of the tuberosities, however, affects the mechanics of the rotator cuff and is very poorly tolerated.
Four-part fractures have an extremely high incidence of avascular necrosis—45% in Neer’s classic series—with the exception of valgus impacted four-part fractures in which the incidence is only 11%.8
In most four-part fractures, the blood supply from the anterior humeral circumflex artery is disrupted, contributing to the high incidence of avascular necrosis.
The posterior humeral circumflex artery also contributes to humeral head vascularization, and the incidence of avascular necrosis increases with lateral displacement of the humeral head in four-part fractures.
The blood supply is maintained in most valgus impacted fractures by the branches from the posterior humeral circumflex artery along the intact medial periosteal hinge (FIG 3), making this particular fracture configuration very amenable to fixation.
PATIENT HISTORY AND PHYSICAL FINDINGS
A complete history of injury is important to determine the mechanism of injury. It is helpful to differentiate low-energy from high-energy injuries.
Elderly individuals often sustain proximal humerus fractures as the result of low-energy injuries such as slipping and falling. These injuries often are very amenable to minimally invasive fixation techniques because the displacement is manageable and the periosteal sleeve between fracture fragments often is intact. The rotator cuff often is intact as a sleeve. All these qualities facilitate minimally invasive reduction and fixation techniques.
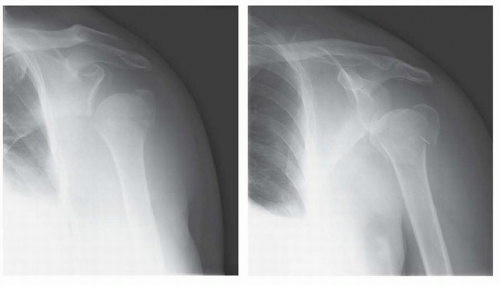
FIG 3 • Valgus impacted fractures maintain blood supply to the articular surface via ascending branches off the posterior humeral circumflex artery along the intact medial periosteal hinge.
In younger individuals, proximal humerus fractures often result from higher energy injuries. These fractures commonly have greater fracture fragment displacement, rotator cuff tears between the tuberosities, and disruption of the periosteal sleeve. These factors do not necessarily preclude percutaneous pinning but make it more challenging and should be considered in preoperative planning.
Other important aspects of the history include the following:
Previous history of injury to the affected shoulder
Previous shoulder function
History of numbness or tingling in the affected extremity
Rule out elbow and wrist fractures, especially in osteoporotic patients with injuries resulting from a fall on an outstretched arm.
Patients often hold the shoulder inferior on the affected side.
Examination should include skin integrity, presence of ecchymosis, downward carriage of shoulder girdle, and deformity consistent with shoulder dislocation or acromioclavicular joint separation.
Examine for possible associated nerve injury (usually neurapraxia) by testing sensation to light touch in individual nerve distribution, two-point discrimination, and muscle strength (testing is limited to isometric at shoulder because of limited ROM and pain).
Pay particular attention to axillary nerve function as injuries are common.
Possible associated vascular injury can be determined by testing radial pulse and capillary refill.
IMAGING AND OTHER DIAGNOSTIC STUDIES
A trauma series of radiographs of the shoulder should be obtained (FIG 4).
The series includes an anteroposterior (AP) view of the shoulder, a scapular AP view, a scapular Y view, and an axillary view.
A complete series with these views allows the fracture configuration to be determined in sufficient detail.
A computed tomography (CT) scan is helpful in many cases and should be obtained if there is any question regarding the
extent of fracture involvement or the level of displacement of the fragments. It also is helpful if there is any question of joint dislocation or glenoid fracture.
Radiographs are used to determine whether the fracture is a two-, three-, or four-part fracture and to assess the degree of displacement.
Three-dimensional reconstructions of the CT scan can be helpful in fracture evaluation but are not routinely required.
DIFFERENTIAL DIAGNOSIS
Acromioclavicular joint separation
Glenohumeral joint dislocation
Humeral shaft fracture
Scapulothoracic dissociation
Elbow and wrist fractures (may coexist)
NONOPERATIVE MANAGEMENT
Minimally displaced fractures can be treated nonoperatively.
Displacement at the surgical neck is well tolerated.
An AP view of the shoulder can be misleading in the case of a surgical neck fracture.
The pectoralis major muscle exerts an anterior force on the shaft, resulting in anterior displacement of the shaft relative to the humeral head.
A scapular Y or axillary view can exhibit this angular deformity.
Displacement of the greater tuberosity is less well tolerated.
Historically, 1 cm of displacement has been used as the criterion for clinically significant tuberosity displacement.
Recently, however, even 5 mm of displacement has been considered an operative indication.
Patients wear a sling for 2 to 3 weeks or until the proximal humerus feels stable with gentle internal or external rotation of the arm.
Patients should be instructed to remove the sling for elbow, wrist, and hand ROM to avoid stiffness of these joints.
Early signs of healing (eg, callus formation) also are helpful indicators of when it is safe to commence ROM exercises.
In borderline instances, it is better to err toward a longer period of immobilization to ensure healing because shoulder stiffness is easier to address than a nonunion.
Therapy begins with passive stretching until 6 weeks when active ROM and strengthening can be started, progressing as tolerated.
SURGICAL MANAGEMENT
Preoperative Planning
All imaging studies should be reviewed carefully to determine the type of fracture, the degree of displacement, fracture configuration, and bone quality.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree