14 Percutaneous Cement Augmentation Systems
14.1 Introduction
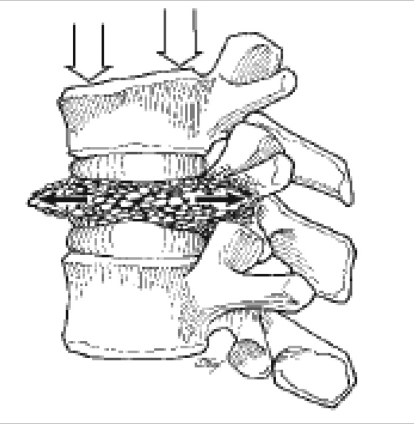
Vertebral compression fractures (VCFs) can result from complications associated with osteoporosis, spinal trauma, or vertebral metastases (▶ Fig. 14.1).1,2 Osteoporotic VCFs are the most prevalent, with an estimated incidence of 1.4 million per year.3 VCFs are associated with significant morbidity, including functional limitations, significant pain, and kyphotic deformity.4,5 Although nonoperative therapy remains the first-line treatment, surgical correction is indicated in cases of uncontrolled pain or progressive deformity.2 Minimally invasive approaches to VCFs involve percutaneous vertebroplasty or kyphoplasty, with cement augmentation of the vertebral body. Vertebral body cement augmentation is associated with the benefits of improved pain control and may help correct angular deformity.
14.1.1 Components
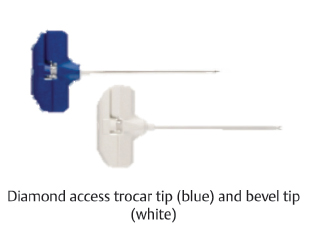
Both vertebroplasty and kyphoplasty are performed under biplanar fluoroscopic guidance. In both procedures, a cannulated trocar is introduced into the vertebral body in conjunction with a spinal needle inserted via a transpedicular route.6 Trocars can be inserted either unilaterally or bilaterally, depending on the location of the compression deformity and the practitioner’s preference. These trocars can accommodate supplementary equipment, including biopsy needles to produce specimens for oncologic testing and drills for removal of bone to create a space for balloon insertion.
Fig. 14.1 Depiction of a vertebral compression fracture with associated forces. (Adapted from Baaj AA, Mummaneni PV, Uribe JS, Vaccaro AR, Greenberg MS. Handbook of Spine Surgery; New York, NY: Thieme; 2012.)
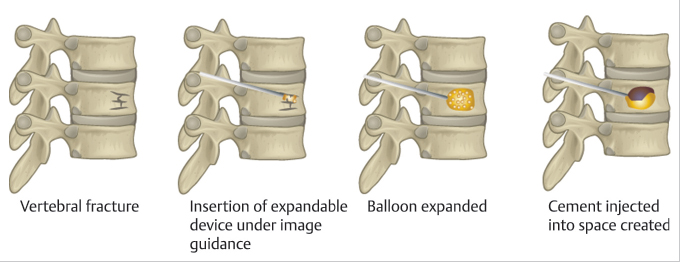
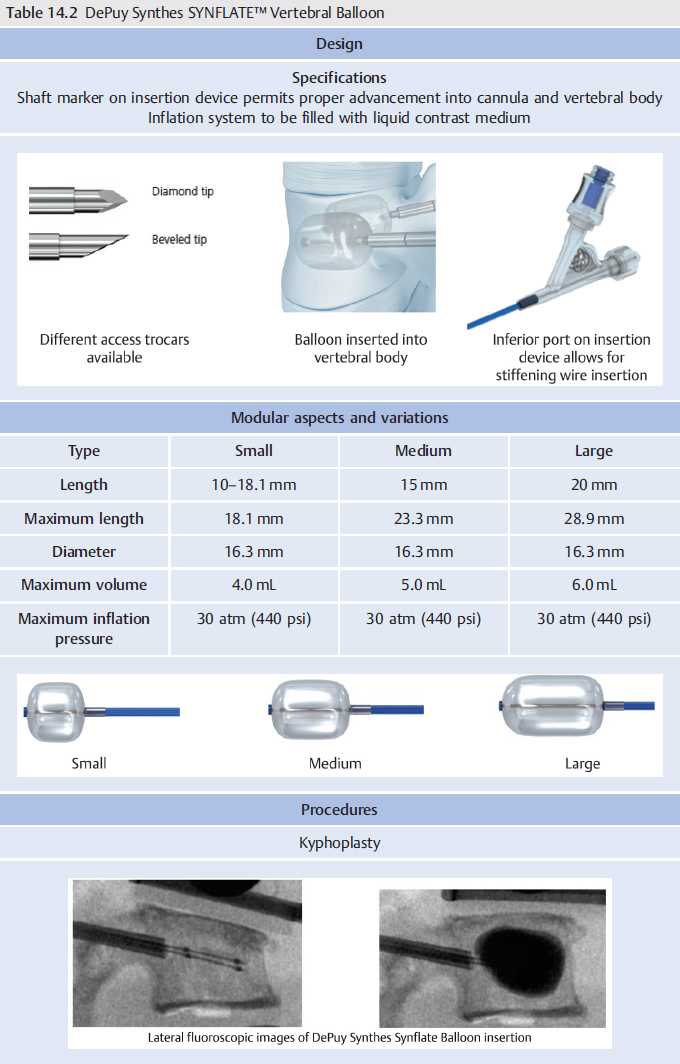
In kyphoplasty, orthopaedic balloons are inserted through the trocars into the vertebral body. These balloons are inflated under pressure within the vertebral body, helping create a potential space for cement insertion.7 The balloons are typically radiopaque and their inflation can be monitored via fluoroscopic guidance. In vertebroplasty, pressurized cement is inserted through the trocar without using a balloon dilator. Shen et al compared the efficacy of kyphoplasty using a vertebral dilator and balloon kyphoplasty to treat osteoporotic thoracolumbar compression fractures.8 The authors reported postoperative change in the lordosis was significantly greater in the dilator kyphoplasty group than in the balloon kyphoplasty group (–9.51 vs. −7.78 degrees, p < 0.001). These findings suggested the vertebral dilator kyphoplasty allows for greater correction of lordotic angle; however, additional prospective studies are required to draw conclusions regarding long-term clinical efficacy.
In both vertebroplasty and kyphoplasty, bone cement is injected through the trocar into the vertebral body. The cement fills the potential space within the vertebral body and provides mechanical support after setting. The bone cement is most commonly comprised of polymethyl methacrylate (PMMA) mixed with barium sulfate. PMMA is a cement polymer that is widely used in orthopaedics due to its biocompatibility and ability to harden quickly.9 Before injection, PMMA bone cement is mixed with a contrast agent such as barium sulfate, so its introduction into the vertebral body can be fluoroscopically monitored (▶ Fig. 14.2).7
14.1.2 Outcomes
Multiple level I studies and meta-analyses have been performed with the purpose of analyzing the differences in postoperative outcomes between VCF treatment modalities.10,11,12 Klazen et al performed a prospective, randomized controlled trial (RCT) of 202 patients undergoing either percutaneous vertebroplasty or conservative management for acute VCFs with Visual Analog Scale (VAS) pain ratings greater than 5.12 The authors demonstrated that patients receiving cement augmentation had significantly greater pain relief at 1 month and 1 year posttreatment compared to the conservative management group. Furthermore, from a cost perspective, it was noted that cement augmentation was a cost-effective modality when a cutoff of €30,000/qualityadjusted life year (QALY) was used. Farrokhi et al performed a similar prospective RCT with 82 patients undergoing treatment for acute osteoporotic VCF with percutaneous vertebroplasty or conservative management.11 The patients receiving percutaneous vertebroplasty not only had significantly greater improvements in pain up to 6 months postoperatively but also had greater improvements in disability as measured by the Oswestry Disability Index (ODI) up to 36 months posttreatment. Additionally, the incidence of subsequent vertebral fracture was lower in the cement augmentation group compared to the conservative group (2.2 vs. 13.3%). Using a meta-analysis, Zhao et al compared the efficacy and safety of vertebroplasty, kyphoplasty, and conservative treatment.13 The authors reported patients who underwent vertebroplasty experienced the greatest pain relief. However, kyphoplasty was the most effective in improving daily function and quality of life. The study also demonstrated that patients who underwent kyphoplasty experienced the lowest incidence of new fractures.
14.1.3 Complications
While promising data exists regarding the utility of percutaneous cement augmentation for improvement in clinical outcomes, the technique is not devoid of complications. The most prominent complication is extravasation of cement out of the vertebral body, with reported incidences ranging from 5.0 to 76.83% depending upon the detection modality used.14,15,16,17,18,19 Although the incidence of cement leakage can be high, most cases are asymptomatic and require no further treatment. While symptomatic cases are rare, they can have significant morbidity and must be managed carefully.20 Sequelae from symptomatic leakages can include pulmonary embolism, venous embolism leading to cardiovascular collapse, neurologic deficits from spinal stenosis, and adjacent level vertebral fracture.14,15,16,21,22,23,24 Compared to kyphoplasty, vertebroplasty is associated with a higher incidence of extravasation-related complications as there are higher intraosseous pressures during cement insertion.14,17,24
A current trend and recent area of interest within the literature has been the use of unilateral approaches to percutaneous cement augmentation. Published investigations comparing unilateral and bilateral procedures have been supportive of the utility of a unilateral approach, demonstrating similar clinical and radiographic outcomes with distinct perioperative advantages.25,26,27,28 For example, Yan et al conducted a prospective study of 316 patients with single-level osteoporotic VCFs treated with either unilateral or bilateral percutaneous balloon kyphoplasty.25 In regard to perioperative factors, the unilateral approach was associated with lower cement volume delivery, shorter operative times, and a reduced radiation dose compared to the bilateral approach. Clinically, both groups demonstrated similar improvements in pain and quality-of-life metrics at final follow-up of at least 24 months postoperatively. Radiographically, both groups had similar improvements in vertebral body height, while the unilateral group had greater kyphotic angle reduction compared to the bilateral group. Total costs were also similar for both groups, taking into account operating room costs, instrument costs, and surgeon’s fees. While these investigations suggest the possible superiority of unilateral cement augmentation approaches over bilateral approaches, further investigation is still required to make any definitive conclusions.
14.2 Percutaneous Cement Augmentation Systems
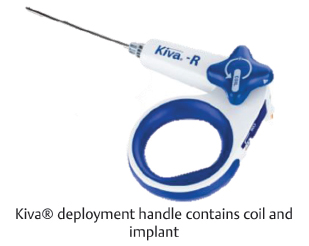
Table 14.1 Benvenue Medical Kiva® Vertebral Compression Fracture Treatment System
Design | ||
Specifications Implant designed as a mechanical support structure to contain and direct flow of cement Flexible implant made from PEEK-OPTIMA® | ||
| ||
Modular aspects and variations | ||
Bone access needle Diamond trocar tip Bevel tip | Implant 20 × 15 mm | Deployment handle Ability to select right or left access |
|
| |
Procedures | ||
Percutaneous vertebral compression fracture | ||
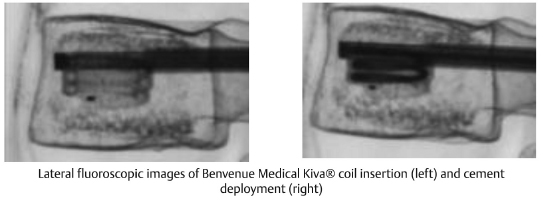
| ||